Facts about Gastroschisis
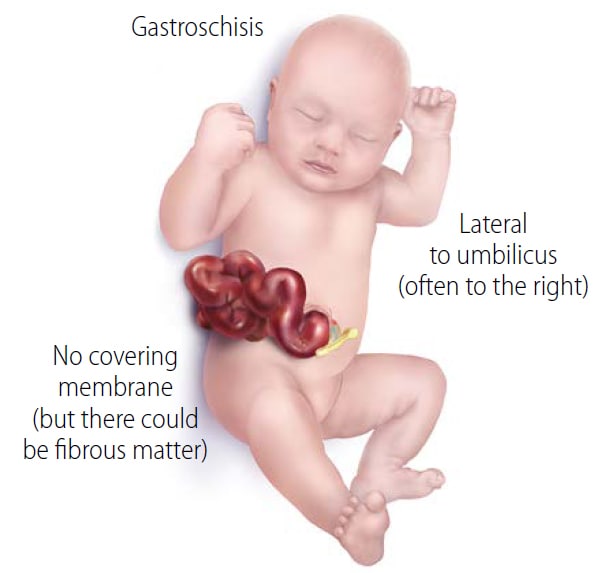
Gastroschisis (pronounced gas-troh-skee-sis) is a birth defect where there is a hole in the abdominal wall beside the belly button. The baby’s intestines, and sometimes other organs, are found outside of the baby’s body, exiting through the hole.
What is Gastroschisis?
Gastroschisis is a birth defect where a hole in the abdominal (belly) wall beside the belly button allows the baby’s intestines to extend outside of the baby’s body. The hole can be small or large and sometimes other organs, such as the stomach and liver, can be found outside of the baby’s body as well.
Gastroschisis occurs early during pregnancy. The hole is usually to the right side of the belly button. Because the intestines are not covered in a protective sac and are exposed to the amniotic fluid, they can become irritated, causing them to shorten, twist, or swell.
How Many Babies are Born with Gastroschisis?
Researchers estimate that about 1 in every 1,953 babies are born each year in the United States with gastroschisis. Several studies have shown that gastroschisis has become more common, particularly among younger mothers.1-3
Causes and Risk Factors
The exact causes of gastroschisis are often unknown. Gastroschisis is likely caused by a combination of genes and other factors, such as things the mother comes into contact within her environment, what the mother eats or drinks, or certain medicines used during pregnancy.
Like many families affected by birth defects, CDC wants to find out what causes them. Understanding factors that are more common among babies with birth defects will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011) and the Birth Defects Study To Evaluate Pregnancy exposureS (BD-STEPS, which began with births in 2014), to understand the causes of and risks for a number of birth defects, including gastroschisis.
Recently, CDC researchers have reported important findings about some factors that affect the risk of having a baby with gastroschisis:
-
- Genitourinary infections: Women who reported a genitourinary infection within three months before or three months after becoming pregnant had an increased chance of having a baby with gastroschisis compared to women who reported a genitourinary infection during the second or third trimester of pregnancy.5
CDC continues to study birth defects like gastroschisis to learn how to prevent them. If you are pregnant or thinking about getting pregnant, talk with your doctor about ways to increase your chance of having a healthy baby.
Diagnosis
Gastroschisis can be diagnosed during pregnancy or after the baby is born. During pregnancy, there are screening tests (prenatal tests) to check for birth defects and other conditions. Gastroschisis might result in an abnormal result on a blood or serum screening test or it might be seen during an ultrasound (which creates pictures of the baby’s body while inside the womb).
Treatments
Gastroschisis is immediately seen at birth. Soon after the baby is born, surgery will be needed to place the abdominal organs inside the baby’s body and repair the defect. Even after the repair, infants with gastroschisis can have problems with nursing and eating, digestion of food, and absorption of nutrients.
If the gastroschisis defect is small (only some of the intestine is outside of the belly), it is usually treated with surgery soon after birth to put the organs back into the belly and close the opening. If the gastroschisis defect is large (many organs outside of the belly), the repair might be done slowly, in stages. The exposed organs might be covered with a special material and slowly moved back into the belly. After all organs have been put back in the belly, the opening is closed.
Babies with gastroschisis often need other treatments as well, including receiving nutrients through an IV line, antibiotics to prevent infection, and careful attention to control their body temperature.
Other Resources
The views of this organization are its own and do not reflect the official position of CDC.
- The Global Gastroschisis Foundation
The Global Gastroschisis Foundation helps children and families affected by gastroschisis. The website has resources for connecting with other families and ways to raise awareness about gastroschisis.
References
- Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS. National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
- Kirby RS, Marshall J, Tanner JP, et al.; for the National Birth Defects Prevention Network. Prevalence and correlates of gastroschisis in 15 states, 1995 to 2005. Obstet Gynecol. 2013 Aug; 122 (2 Pt 1):275-81.
- Jones AM, Isenburg J, Salemi JL, et al.; for the National Birth Defects Prevention Network. Increasing prevalence of gastroschisis—14 States, 1995-2012. MMWR morb Mortal Wkly Rep. 2016 Jan 22;65(2):23-6.
- Bird TM, Robbins JM, Druschel C, Cleves MA, Yang S, Hobbs CA, the National Birth Defects Prevention Study. Demographic and environmental risk factors for gastroschisis and omphalocele in the National Birth Defects Prevention Study. J Pediatr Surg. 2009;44:1546-1551.
- Feldkamp ML, Arnold KE, Krikov S, Reefhuis J, Almli LM, Moore CA, Botto LD. Risk of gastroschisis with maternal genitourinary infections, National Birth Defects Prevention Study 1997-2011. BMJ Open. 2019; 9:e026297.