Colorado Tick Fever
- Home
- Tick ID
- Overview of Tickborne Diseases
- Lyme Disease
- Tickborne Relapsing Fever (TBRF)
- Hard Tick Relapsing Fever
- Anaplasmosis
- Ehrlichiosis
- Rocky Mountain Spotted Fever
- Rickettsia parkeri Rickettsiosis
- Tularemia
- Babesiosis
- Heartland and Bourbon Virus Diseases
- Colorado Tick Fever
- Powassan Virus Disease
- Tickborne Diseases Abroad
- Tick Bites/Prevention
- Lyme Disease Prophylaxis After Tick Bite
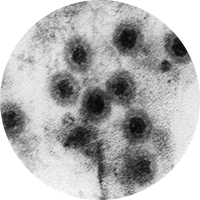
Agent
Colorado tick fever virus
Where Found
The geographic range of Colorado tick fever virus includes the Western United States, primarily Colorado, Utah, Montana, and Wyoming. Although rare, the virus can also be transmitted from person-to-person via blood transfusion.
Incubation Period
1–14 days
Signs and Symptoms
- Fever, chills, headache, myalgias, and lethargy
- ~50% of patients have a biphasic illness with symptoms remitting after 2 to 4 days, but then recurring 1 to 3 days later.
- Conjunctival injection, pharyngeal erythema and lymphadenopathy may be present.
- Maculopapular or petechial rash in <20% of patients
- Prolonged convalescence characterized by weakness and fatigue is common in adults.
- Life-threatening complications and death are rare and usually associated with disseminated intravascular coagulation or meningoencephalitis in children.
General Laboratory Findings
- Leukopenia
- Moderate thrombocytopenia
Laboratory Diagnosis
Preliminary diagnosis of Colorado tick fever (CTF) is based on signs and symptoms, places and dates of travel, activities, and history of potential tick exposure. Acute samples should be tested by reverse-transcriptase polymerase chain reaction (RT-PCR) to detect viral RNA as antibody production is delayed until 14–21 days after onset of symptoms.
Note: CSF, cerebrospinal fluid; CNS, central nervous system
| Timing of specimen collection | Specimens | Preferred Test |
|---|---|---|
| <14 days after symptom onset | Serum (CSF if suspected CNS involvement) | RT-PCR for viral RNA |
| ≥14 days after symptom onset | Serum (CSF if suspected CNS involvement) | Antibody testing*; consider RT-PCR for samples from days 14-21 |
*If possible, acute and convalescent samples, collected at least 2 weeks apart, with the convalescent sample collected at least 3 weeks after symptom onset, should be obtained to look for seroconversion or a 4-fold rise in antibody titers typically using a plaque reduction neutralization test (PRNT).
Note: CTF testing is available at some commercial and state health department laboratories and at CDC. Contact your state or local health department for assistance with diagnostic testing. CTF cases are reportable to local public health authorities in certain states.
Treatment
No specific antiviral treatment is available. Patients with suspected CTF should receive supportive care as appropriate. Patients with confirmed CTF should defer blood and bone marrow donation for at least 6 months after recovery.
References
Brackney MM, Marfin AA, Staples JE, et al. Epidemiology of Colorado tick fever in Montana, Utah, and Wyoming, 1995–2003. Vector Borne Zoonotic Dis 2010;10:381–385.
Centers for Disease Control and Prevention. West Nile virus and other nationally notifiable arboviral diseases—United States, 2016. MMWR 2018; 67(1);13-17.
Staples JE, Fischer M. Coltiviruses (Colorado Tick Fever). In: Principles and Practice of Pediatric Infectious Diseases, 5th edition. Eds: Long SS, Prober CG, Fischer M. Elsevier 2018:1119–1121.
Goodpasture HC, Poland JD, Francy DB, et al. Colorado tick fever: clinical, epidemiologic, and laboratory aspects of 228 cases in Colorado in 1973–1974. Ann Intern Med 1978;88:303–310.
Kadkhoda K, Semus M, Jelic T, Walkty A. Case report: a case of Colorado tick fever acquired in southwestern Saskatchewan. Am J Trop Med Hyg. 2018;98:891–893.
Lambert AJ, Kosoy O, Velez JO, et al. Detection of Colorado Tick Fever viral RNA in acute human serum samples by a quantitative real-time RT-PCR assay. J Virol Methods 2007;140:43–48.
McDonald E, George D, Rekant S, et al. Notes from the field: Investigation of Colorado tick fever virus disease cases — Oregon, 2018. Morb Mortal Wkly Rep. 2019;68:289–290.
Romero JR, Simonsen KA. Powassan encephalitis and Colorado tick fever. Infect Dis Clin North Am 2008;22:545–559.
Williamson BN, Fischer RJ, Lopez JE, et al. Prevalence and strains of Colorado tick fever virus in Rocky Mountain wood ticks in the Bitterroot Valley, Montana. Vector Borne Zoonotic Dis. 2019;19:694–702.
Yendell SJ, Fischer M, Staples JE. Colorado tick fever in the United States, 2002-2012. Vector Borne Zoonotic Dis 2015;15:311–316.