Diagnostic Methods
Poliovirus can be detected in specimens from the throat, feces (stool), and occasionally cerebrospinal fluid (CSF) by isolating the virus in cell culture or by detecting the virus by polymerase chain reaction (PCR).
CDC laboratories conduct testing for poliovirus, including:
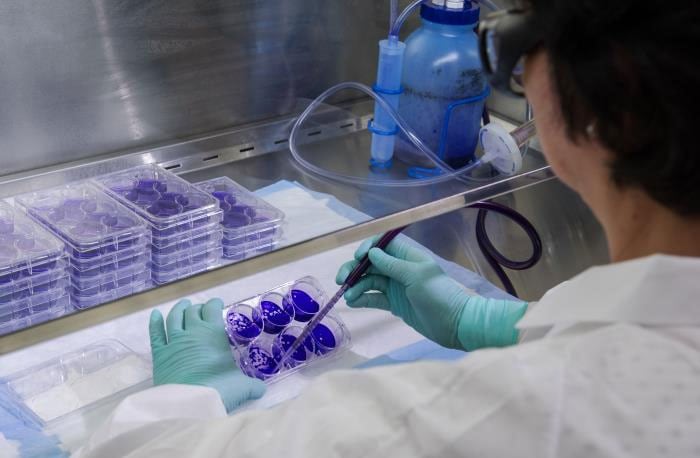
- Culture
- Intratypic differentiation
- Genome sequencing
- Serology
Virus isolation in culture is the most sensitive method to diagnose poliovirus infection. Poliovirus is most likely to be isolated from stool specimens. It may also be isolated from pharyngeal swabs. Isolation is less likely from blood or CSF.
To increase the probability of isolating poliovirus, collect at least two stool specimens 24 hours apart from patients with suspected poliomyelitis. These should be collected as early in the course of disease as possible (ideally within 14 days after onset).
Real-time reverse transcription PCR is used to differentiate possible wild strains from vaccine-like strains (“intratypic differentiation”), using virus isolated in culture as the starting material.
Partial genome sequencing is used to confirm the poliovirus genotype and determine its likely geographic origin.
Serology may be helpful in supporting the diagnosis of paralytic poliomyelitis, particularly if a patient is known or suspected to not be vaccinated. An acute serum specimen should be obtained as early in the course of disease as possible, and a convalescent specimen should be obtained at least 3 weeks later.
Detection of poliovirus in CSF is uncommon. CSF usually contains an increased number of leukocytes [from 10 to 200 cells/mm3 (primarily lymphocytes)] and a mildly elevated protein (from 40 to 50 mg/dL). These findings are nonspecific and may result from a variety of infectious and noninfectious conditions.
For more information on specimens, see Polio Specimen Collection, Storage, and Shipment.