Poliomyelitis: Clinical Presentation
Updated August 10, 2022
In July 2022, CDC was notified of a case of polio in an unvaccinated individual from Rockland County, New York, caused by vaccine-derived poliovirus type 2. CDC is consulting with the New York State Department of Health on their investigation. This does not change CDC recommendations for polio vaccination. CDC urges everyone who is not fully vaccinated to complete the polio vaccination series as soon as possible. Small updates were made on these pages to emphasize vaccination recommendations for adults, clarify next steps when suspecting a case of polio, and update references.
Although poliovirus is no longer endemic in the United States, it’s important that healthcare professionals rule out poliovirus infection in cases of unexplained acute flaccid paralysis (AFP) that are clinically compatible with polio, particularly those with anterior myelitis, to ensure that any importation of poliovirus is quickly identified and investigated. See the MMWR case study on AFP for more information.
There has not been a case of wild polio acquired in the United States since 1979. The last imported case of wild polio was in 1993. However, poliovirus infections still occur in some countries and could easily be brought into the United States. In the last decade, many polio-free countries have had cases of polio imported through international travel.
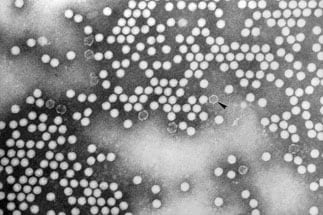
Poliovirus is a member of the Enterovirus genus, family Picornaviridae. Enteroviruses are transient inhabitants of the gastrointestinal tract and are stable at acidic pH. Picornaviruses are small, ether-insensitive viruses with an RNA genome. Poliovirus is highly contagious and causes polio, or poliomyelitis, a serious and debilitating disease.
There are three poliovirus serotypes (PV1, PV2, and PV3) with minimal heterotypic immunity between them. That is, immunity to one serotype does not produce significant immunity to the other serotypes.
Poliovirus infects only humans. Infection is more common in infants and young children. Polio occurs at an earlier age among children living in poor hygienic conditions. In temperate climates, poliovirus infections are most common during summer and autumn. In tropical areas, the seasonal pattern is less pronounced.
The virus enters through the mouth and multiplies in the oropharynx and gastrointestinal tract. The virus is usually present in nasopharyngeal secretions for 1 to 2 weeks and can be shed in stools for several weeks after infection, even in individuals with minor symptoms or no illness.
Most people infected with poliovirus will not have any visible symptoms. About one out of four people will have flu-like symptoms. These symptoms usually last 2 to 5 days, then go away on their own.
Fewer than 1% of people will have weakness or paralysis in their arms, legs, or both. The paralysis can lead to permanent disability and death.
The poliovirus incubation period for nonparalytic symptoms is 3 to 6 days. The onset of paralysis usually occurs 7 to 21 days after infection.
Polio vaccine provides the best protection against polio.
CDC recommends that children and adults who are unvaccinated or incompletely vaccinated get polio vaccine to protect against polio, or poliomyelitis.
For specific vaccination recommendations visit: Polio Vaccination: For Healthcare Providers.
Adults who had paralytic poliomyelitis during childhood may develop noninfectious post-polio syndrome (PPS) 15 to 40 years later. PPS is characterized by slow and irreversible exacerbation of weakness often in those muscle groups involved during the original infection. Muscle and joint pain also are common manifestations. The prevalence and incidence of PPS is unclear. Studies estimate that 25–40% of polio survivors suffer from PPS.
 [PDF - 2 MB]
[PDF - 2 MB]Acute flaccid paralysis (AFP) is a manifestation of a wide spectrum of clinical diseases. Worldwide, children younger than 15 years are the age group at highest risk of developing polio and some other forms of AFP. Even in the absence of laboratory-documented poliovirus infection, AFP is expected to occur at a rate of at least 1 per 100,000 children annually. It can result from a variety of infectious and noninfectious causes. Known viral causes of AFP include enterovirus, adenovirus, and West Nile virus. However, AFP caused by these agents is very uncommon in the United States. A study examining AFP in 245 children younger than 15 years in California from 1992-1998 found the most common diagnoses were Guillain-Barré Syndrome (23%), unspecified AFP (21%), and botulism (12%).
Polio Case Definition and Diagnosis
A probable case of polio is defined as an acute onset of flaccid paralysis of one or more limbs with decreased or absent tendon reflexes in the affected limbs, without other apparent cause, and without sensory or cognitive loss.
Paralysis usually begins in the arm or leg on one side of the body (asymmetric) and then moves towards the end of the arm or leg (progresses to involve distal muscle groups). This is described as descending paralysis. Many patients with AFP will have a lumbar puncture and analysis of cerebrospinal fluid (CSF) performed as part of their evaluation. Detection of poliovirus in CSF from confirmed polio cases is uncommon, and a negative CSF test result cannot be used to rule out polio.
Consider polio in patients with polio-like symptoms, especially if the person is unvaccinated, incompletely vaccinated, recently traveled abroad to a place where polio still occurs, or was exposed to a person who recently traveled to one of these areas. Only healthcare workers with evidence of complete polio vaccination should attend to the patient.
If you suspect polio:
- Practice good hand hygiene and contact precautions when interacting with the patient.
- Evaluate the patient for flaccid weakness and document tone, reflexes, and muscle strength.
- Poliomyelitis has been classified as immediately notifiable, extremely urgent. Contact the state or local health department immediately to report a patient with suspected poliomyelitis.
- Work with the state and local health department to order poliovirus testing:
- Collect appropriate stools (whole stool) and throat specimens (OP swab): 2 specimens of each taken at least 24 hours apart during the first 14 days after onset of paralytic disease.
- Store specimens at –20 degrees celsius and ship frozen.
- For questions, contact the CDC Emergency Operations Center at 770-488-7100.
The rapid investigation of suspected polio cases is critical to identifying possible poliovirus transmission and implementing proper control measures. For more information see CDC poliomyelitis guidelines for epidemiologic, clinical, and laboratory investigations of AFP to rule out poliovirus infection.
Paralytic polio has been classified as “Immediately notifiable, Extremely Urgent,” which requires that local and state health departments contact CDC within 4 hours.
Non-paralytic polio has been classified as “Immediately notifiable, Urgent,” which requires that local and state health departments contact CDC within 24 hours.
CDC (Emergency Operations Center, 770-488-7100) will provide consultation regarding:
- The collection of appropriate clinical specimens needed for poliovirus detection
- The initiation of appropriate consultations and procedures to rule out or confirm poliomyelitis
- The compilation of medical records
For more information about what should be collected as part of a case investigation see:
- Polio – Vaccine Preventable Diseases Surveillance Manual
- Suspected Polio Case Worksheet [PDF – 95KB]
Each state and territory has regulations or laws governing the reporting of diseases and conditions of public health importance. These regulations and laws list the diseases to be reported and describe those persons or groups responsible for reporting such as healthcare providers, hospitals, laboratories, schools, daycare and childcare facilities, and other institutions. Contact your state health department for reporting requirements in your state.
- Progress Toward Polio Eradication — Worldwide, January 2020–April 2022
- Polio – Vaccine Preventable Diseases Surveillance Manual
- Guidance for Assessment of Poliovirus Vaccination Status and Vaccination of Children Who Have Received Poliovirus Vaccine Outside the United States
- Paralytic syndromes in children: epidemiology and relationship to vaccination.
- Acute Flaccid Paralysis with Anterior Myelitis — California, June 2012–June 2014
- Zangwill KM, Yeh SH, Wong EJ, Marcy SM, Eriksen E, Huff KR, et al. Paralytic syndromes in children: epidemiology and relationship to vaccination. Pediatr Neurol. 2010;42(3):206-12.