Phased Approach to Respond to Community Inquiries: Phase 2
Phase 2: Criteria to Determine Continued Assessment of a Report of an Unusual Pattern of Cancer
This section outlines the process for reviewing data and criteria for decision making to determine continued assessment. As described previously, population mobility, historic opportunities for exposure, and other factors may limit analyses and interpretation of data. Other important considerations are presented later in this section.
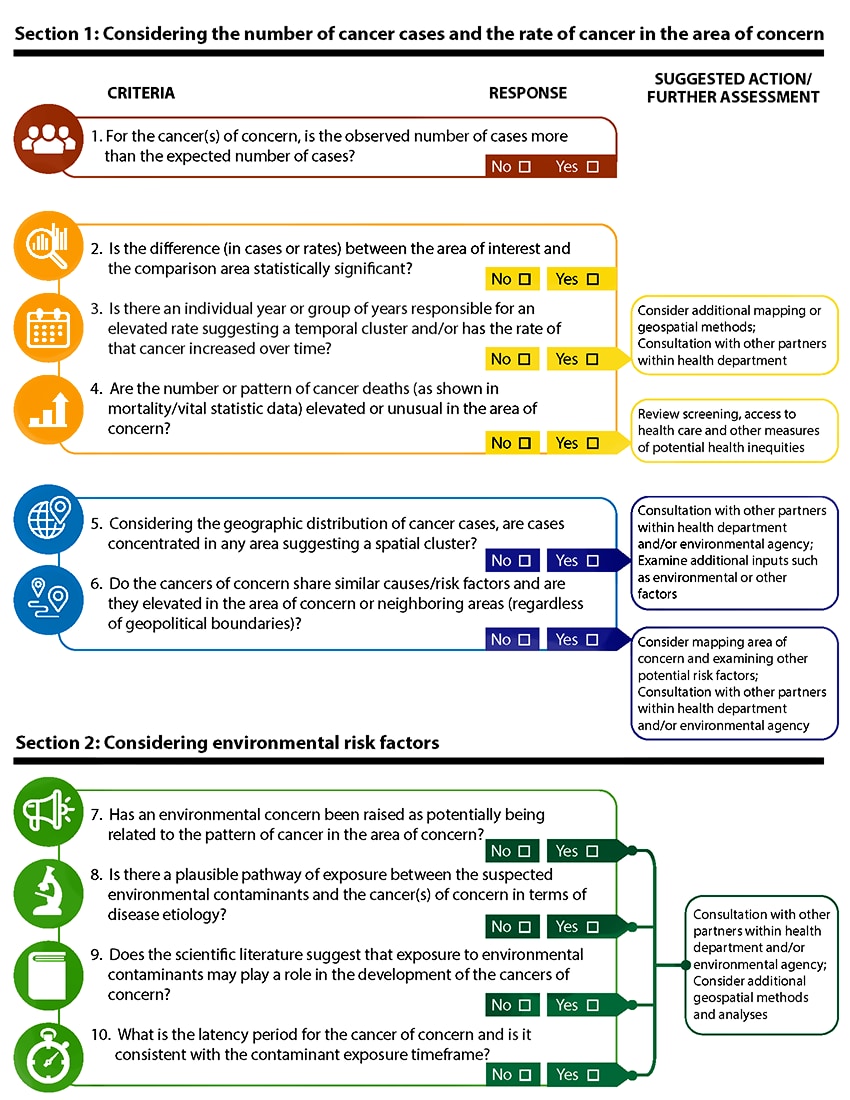
The following criteria are meant to assess the cancer(s) of concern and/or related environmental risk factors. These criteria promote further assessment of unusual patterns of cancer that may not always meet the formal definition of a cancer cluster. The form below is included on the Resources and Tools webpage and can be used as a decision-making guide for assessing the criteria. A discussion on how to evaluate the criteria follows. Resources and capacity may dictate the extent to which the criteria can be fully evaluated.
Proceeding Based on Responses to Criteria
Use the following information below to determine next actions. A downloadable form can be on the found in Resources and Tools webpage.
If ALL answers to sections 1 and 2 above are “No”
- No further assessment needed at this time.
- Summarize collected information in a written report or letter; provide summary to the inquirer/cPOC. The summary should include the following:
- Background information on patterns of cancer observed (rates and geography)
- An explanation of how the agency investigated the inquiry about unusual patterns of cancer
- A review of findings regarding the cancer(s) of concern
- A discussion of risk factors for the cancer(s) mentioned in the original inquiry
- Agency plans or next steps based on the findings
- A note or reference about routine monitoring and follow up
- Continue routine monitoring as appropriate, and plan to include this cancer and area of concern in routine evaluation of cancer data (to determine if the pattern changes):
- Conduct routine monitoring aimed at identifying unusual patterns of cancer using geospatial/statistical tools (and data that may be routinely available at geographic levels lower than the state as a whole).
- Maintain the feedback loop with the original inquirer and establish procedures for future updates (e.g., making more geographically granular data available on the health department website).
If answer to question 1 is “Yes,” AND answer to any other question in section 1 is “Yes”
Further assess the cancer pattern. This assessment may include consultation and/or referral to a cancer prevention and control program for consideration of intervention activities or additional information gathering such as a case series analysis, described more in Phase 3. Further assessment could also include defining the geographic area or time frame of concern using spatial and temporal methods.
If answer to any question in section 2 is “Yes”
Consider information from section 2 (environmental data and environmental risk factors) during the additional assessment and/or referral to, or collaboration with, another agency (e.g., the local water department, the state environmental regulatory agency, ATSDR).
In all of the scenarios presented above, the following actions should be considered:
- Communicate with the inquirer (about types of cancer and area of concern) to help raise cancer awareness and provide a state/local health official the opportunity to explain how cancer rates are calculated.
- Summarize the information from the decision template form (after completing Phase 2). This summary should describe the information evaluated and what type of follow up steps might be taken. The summary can also include next steps in terms of monitoring the pattern of the cancer(s) of interest in the area of concern to determine whether the pattern of cancer changes.
- Consider presenting the information in a community meeting or public availability session, prior to issuing any type of media release (if, for example, the inquiry was made on behalf of a neighborhood or organized group).
Considerations When Reviewing Data in Section 1
- Use the statistical significance of the SIR as part of the criteria discussed below to help determine next steps in the investigation. While statistical significance should not be the deciding factor, it does provide some measure of whether cancer seems to be occurring unusually in time, space, or both. Additional information for interpretation of results, such as the magnitude of the estimate and a discussion of confidence intervals, is provided in Appendix A.
- Consider examining other factors such as access to care or recommended cancer screening rates if an observed cancer rate is lower than expected.
- Consider reviewing the distribution of diagnoses by characteristics such as age, sex, and histology (cell type) compared to national and state distributions, which may highlight important differences for review.
- Look at incident cases for each year (if possible, for the cancer type) within the 5- or 10-year period used to calculate the SIR or standardized mortality ratio (SMR) to determine the potential for a temporal pattern. For example, are the majority of cases within the 5- or 10- year time period occurring within a 1- or 2-year part of that overall period? This type of focused evaluation of a potential temporal pattern can also be instructive in better understanding the potential for some factor (or set of factors) to have played a role in cancer occurrence. Depending on the cancer(s) of concern and the geographic area, small case numbers can impact analyses. Some patterns observed in shorter time periods may be the result of other factors such as random fluctuation or population movement over time.
- Use mortality data to further determine patterns of cancer. In some cases, primary or secondary intervention activities by other parts of the health department could be considered. For example, if the incidence rate in the community is low, but the death rate is high for a particular cancer, this may suggest inequities in access to healthcare and/or environmental justice issues.
- Evaluate the geographic distribution of cancer cases within the area of concern to determine the likelihood of a spatial cluster. Pre-defining the geographic boundaries for the area of interest and qualitative and quantitative evaluation of the data is important in this process. Consider limitations regarding population mobility and latency of specific cancers.
- Evaluate the pattern of cancers of concern in neighboring areas (e.g., census tracts or neighborhoods) and border communities within and across state lines. This may identify regional trends and patterns. This is of particular importance if an environmental concern is also expressed in the neighboring area. This approach provides an opportunity to evaluate geographic patterns that may emerge without reliance on geopolitical boundaries.
- When selecting comparison populations, ensure that areas that are similar demographically are not also similar in terms of environmental hazards and contamination. Ensuring such appropriate comparisons can help address issues of environmental justice and health equity. See Appendix B for more about spatial and temporal methods to quantitatively evaluate unusual patterns. Technical assistance can be requested from CDC/ATSDR if more guidance and expertise are needed.
- Data considerations discussed in the proactive evaluation section may also be useful in this phase.
Considerations When Reviewing Data in Section 2
- Collaborate with internal and external partners, as needed, if an environmental concern is identified or suggested. Collaborate with these partners to acquire or review environmental data. Remember, the community member/inquirer may provide useful information associated with environmental concerns, such as historic land use of the area or concerns about potential contamination related to former use of a property. Census data can indicate population changes over time, but the inquirer may also have qualitative, historic information relative to population change. This information on population change and land use can have significant impacts on decisions associated with the likelihood that exposure to environmental hazards might be associated with cancer occurrence, particularly as it relates to cancer latency/development periods as well as biologic plausibility.
- Consider the biologic plausibility of the cancer(s) of concern being associated with the environmental factors for investigatory purposes as well as for risk communication. Consideration of the possible exposure routes is a principal factor in understanding whether cancer and exposure to environmental agents are potentially connected. Responding to environmental concerns may be important even if the cancer patterns do not suggest a plausible relationship.
Other Considerations
- Community members may have a list of individuals diagnosed with cancer or a map presenting individual addresses. While health officials cannot publicly confirm whether individuals on such a list or map have cancer (due to patient confidentiality and privacy laws), nor can they use personally identifiable information (PII), some non-PII information can help identify the types of cancer(s) of concern as well as the time period and geographic area of interest. Cancer incidence data must be confirmed through the cancer registry data. Sharing information about confidentiality and privacy laws associated with individual health outcomes with the community may be useful.
- Periodically, community inquiries may involve concerns about unusual patterns of cancer(s) in a school, preschool, or daycare setting, which can involve both students and staff members. Work closely with school officials to determine the cancer(s) and environmental concerns reported, the population at risk, and the time frame during which the cancers were diagnosed. For concerns that include occupational populations (e.g., teachers and staff members), state and federal occupational health officials should be consulted. Consider whether community-level environmental factors or concerns are present and whether a community-based investigation approach is appropriate. If the school setting remains the focus, information about the total population at risk will be needed (specific to age and sex if possible) to calculate a cancer rate among the relevant population, but such information might not be available. Population and other sociodemographic data from the U.S. Department of Education’s National Center for Education Statistics may be helpful. If population and case information is available, a similar approach to addressing community-based concerns about unusual patterns of cancer can be used for assessment in these settings.
- Collaborate with other partners as needed. As mentioned previously, have a plan to reach out to collaborators to discuss the cancer inquiry and data evaluation. Collaborators could include other staff members within the health department and potentially other health agencies such as local health jurisdictions or tribal health agencies. For example, concerns associated with occupational exposures should be discussed with state and federal occupational health officials. PEHSU clinicians may offer information related to exposure risk reduction measures when possible and provide several resources and expertise related to children, expectant parents and families. PEHSUs can provide technical environmental medicine expertise, advice on risk reduction activities, and can be a trusted voice in community engagement.
Communication Reminders
- Review with the inquirer what data was included in the assessment. When an SIR or SMR is calculated, describe how the numerator and the denominator are determined, and explain how these data are used to calculate an observed rate and an expected rate of cancer.
- Describe the process used to evaluate cancer patterns in a given area. Discuss why rates are generally calculated in 5- or 10-year intervals to enhance statistical stability due to the small number of annual events in smaller geographic areas.
- Explain how comparing cancer patterns across communities and/or counties is important.
Response Associated with a Need for Further Assessment
As mentioned above, a report should be prepared that summarizes all of the steps taken to evaluate the information and concerns initially reported and why further assessment is advised. The report should include the following:
- Description of the results from the 10-criteria evaluation [PDF – 169 KB] to determine what further actions are taken.
- Assessment of any environmental concerns that have been expressed and/or explored
- Clear description of next steps, if any
- An estimated time frame for when the inquirer might learn of new information
The report should also include the following information, as appropriate:
- If the next steps are associated with actions the responding program must undertake (e.g., a case series analysis, case-control study, etc.), then describe the actions that would be necessary to undergo such an analysis.
- If the further assessment involves action by another program within the health agency, then include the program and a contact person.
- If the action(s) to be taken involve an agency external to the health department, then provide the agency, program name, and a point of contact.
Establishing Strong Relationships and Partnerships with the Community
When further assessment activities are warranted, develop and implement a community engagement plan. Developing a plan together with community partners to share information on a regular basis regarding cancer and environmental health investigations will enhance trust and credibility. Consider including the following people:
- Personnel within the health department with expertise in establishing strong relationships, such as public health nurses and/or social workers (i.e., to serve as aPOCs)
- Local medical professionals, such as PEHSU clinicians
- A trusted community member (i.e., to serve as a cPOC)