Proactive Evaluation and Routine Monitoring of Cancer Data
Evaluating unusual patterns of cancers most commonly begins with an inquiry originating outside of a STLT partner organization and mostly from community concerns. While it is important for communities to be able to identify concerns and bring them to health departments, STLT partners have access to cancer data that can be evaluated in a proactive manner. Based on STLT survey feedback, about half of the responding public health agencies analyze cancer incidence data on a routine basis to proactively look for geographic areas with elevated cancer rates. Therefore, in addition to describing responsive approaches for addressing concerns raised by communities, the guidelines encourage proactive evaluation of cancer registry data to monitor cancer trends and identify unusual patterns.
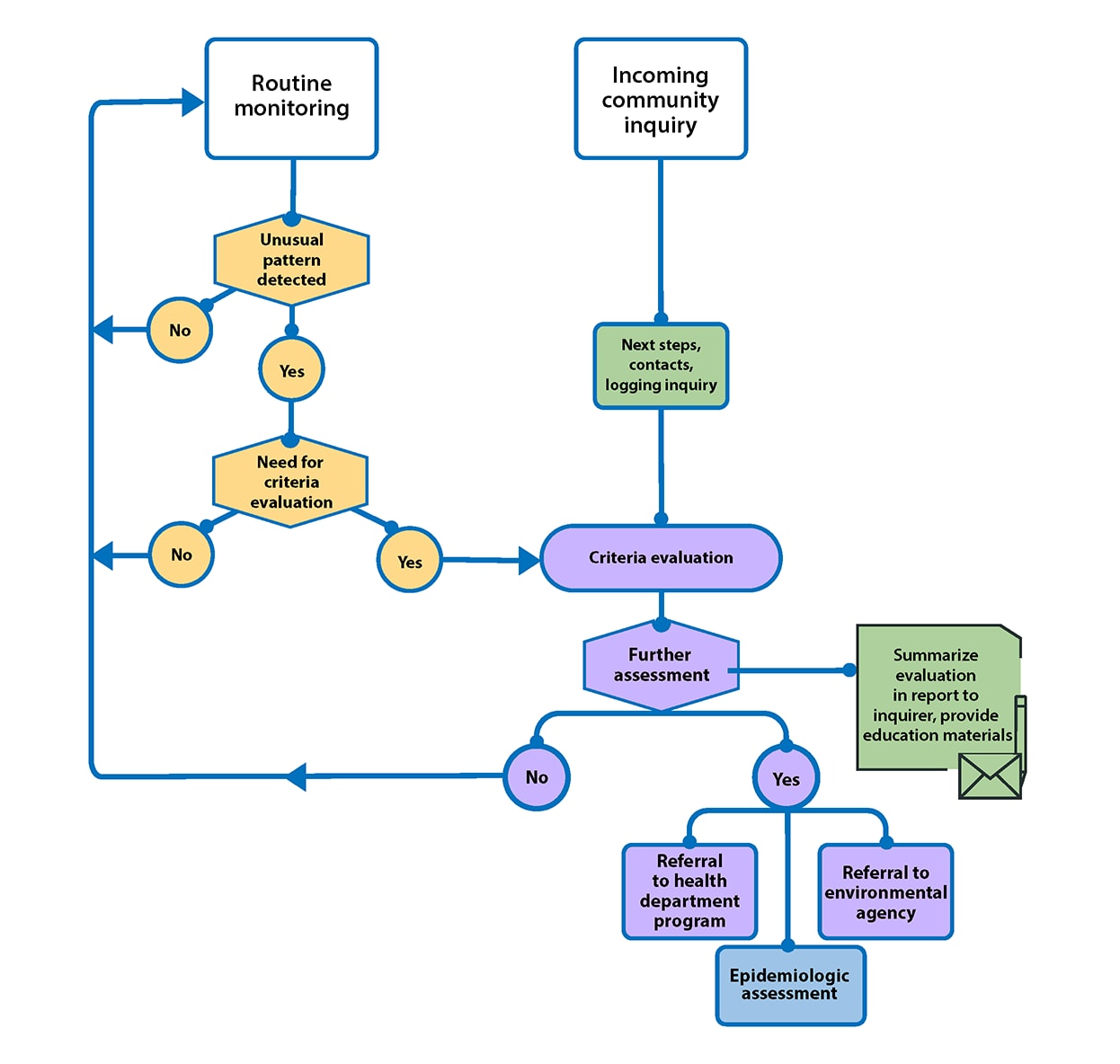
The proactive evaluation of cancer registry data is consistent with the 10 Essential Public Health Services (EPHS) by sustaining an ongoing understanding of health in the jurisdiction through the collection, monitoring, and analysis of health data and other factors to identify threats, patterns, and emerging issues, notably with an emphasis on disproportionately affected populations (24,25). State resources may limit or impact the frequency for which state health departments have capacity to do proactive monitoring or carry out routine monitoring. Further, geographic areas with small populations and selection of geographic boundaries may impact the frequency with which this type of monitoring may detect meaningful differences. Figure 2 outlines the enhanced process for evaluating patterns of cancer routinely and evaluating community inquiries about unusual patterns of cancer and environmental concerns. More details associated with the process are provided later in this document.
Strengthening Partnerships
All states have population-based cancer registries and conduct routine reviews of cancer incidence data. While cancer registry personnel (as data stewards) routinely review data, partnering with epidemiologists, statisticians, environmental health scientists, and other agency health officials who conduct community cancer investigations could promote the following:
- Awareness and attention to unusual patterns of cancer
- A more routine and robust evaluation of cancer data
- A more proactive (as opposed to responsive) approach to the evaluation of cancer data
State program organization and resources differ, and it may be useful to clarify roles with community members.
The Value of Making Cancer Rates Publicly Available
Strong partnerships between population-based cancer registries and other public health professionals can aid in addressing community concerns and questions about unusual patterns of cancer within certain geographic areas. One critical way to do this is for cancer registry, environmental health, and other staff members to work together to make sub-state level cancer rates publicly available. To supplement the annual review of cancer registry data, many states have provided data at a more geographically granular level, while using methods to preserve privacy and confidentiality, (e.g., county and census tract-level cancer rates) as part of the CDC Environmental Public Health Tracking Program (26,27). Other states may have differing state laws or regulations or do not have the same resources and expertise, and they may not be able to publish their cancer data similarly.
Evaluating Patterns of Cancer
Partnerships with cancer registry personnel and access to registry data enable state health officials to calculate cancer-specific crude and adjusted rates for predetermined geographic locales such as counties and census tracts. Health officials can use data available from state cancer registries to proactively evaluate and routinely monitor estimates of expected rates for cancers and explore how the rates compare to what is observed, which is known as calculating a standardized incidence ratio (SIR).
The SIR is an estimate of the observed cancers in a population compared to what might be expected if the population had the same cancer experience as some larger comparison population, such as the state as a whole (28). Age-adjusted county rates can generally be compared to the same cancer-specific, age-adjusted rate estimated for that state (29,30). Appendix A further discusses considerations for calculating the SIR and for reference populations. CDC’s National Environmental Public Health Tracking Program publishes county-level cancer rates and counts as well as standardized incidence ratios on their Tracking Network Data Explorer (31). Having these data readily available may allow states to proactively evaluate and routinely monitor potential issues that may warrant further assessment. Additionally, the Tracking Network Data Explorer also publishes environmental data facilitating further exploration of potential risk factors, especially when resources to collect new data may be limited. If resources are available, Phase 2 and the appendices of this document describe additional analytical methods for consideration.
If the observed number of cases is the same as the expected number of cases, the value of an SIR is 1.0, sometimes multiplied by 100 for presentation. The interpretation of the SIR is not straightforward. For routine evaluation, SIRs that deviate from 1.0 (or 100) may be examined further, with consideration of the confidence intervals (see Appendix A for additional guidance). In addition to the SIR, programs may consider visualization methods and techniques to examine cancer rates relative to the distribution of population characteristics and/or potential environmental risk factors (32). Programs may apply spatial, temporal, or spatiotemporal methods designed to identify unusual distributions or unusual patterns to evaluate the distribution of cancers either in supplement to, or in parallel with, routine evaluation of the SIR (see Appendices A & B for more details).
Determining the Need for Criteria Evaluation
If an unusual cancer pattern is identified, STLT programs responsible for proactive evaluation and routine monitoring of cancer rates should actively seek out other internal partners as appropriate (such as cancer registry personnel, environmental public health programs, or cancer control programs) to discuss findings, gather additional data, and develop a follow-up plan if warranted. Programs should consider factors in the geographic areas where an unusual pattern was identified to determine steps in further assessment. For example, there may be times when cancer control programs have enhanced recommended cancer screening efforts in an area resulting in higher rates of a particular cancer. Other risk factors such as smoking, physical activity, and nutrition can affect cancer incidence in a community (9). In other cases, small numbers may limit the interpretability of the findings and thus ongoing routine monitoring to evaluate the pattern over time is optimal without the need for more immediate further evaluation. However, in some instances, patterns may suggest the need for further evaluation and the use of the 10-criteria assessment tool [PDF – 169 KB] can be utilized (referenced in Phase 2: Assessment of Criteria). Limitations associated with resources and data availability (for example, frequency of analysis, migration of population, choice of geographic boundaries, or changes in other risk factors) may impact findings.
Processes should be in place in advance to inform communities when an unusual pattern is observed and further assessment is warranted. Working with the agency’s communications team to discuss SIR interpretations and messaging is an important step. Resource materials can be found on the Resources and Tools webpage. Community discussions about how to move forward should consider specific community needs (e.g., language and other cultural factors). Oftentimes local health officials are aware of community leaders in their jurisdiction who might serve as a good partner and resource.
Additional Data Sources
Additional data sources may provide more timely information on cancer patterns. Mortality data may be useful as a supplemental data source to the cancer registry data. State vital statistics registries provide access to cancer mortality data (33). Review of mortality data may be particularly helpful in addressing or understanding issues associated with disease burden or issues related to health equity such as differential access to care. In addition, evaluating mortality data along with cancer incidence data may provide insights regarding potential elevations in cancer that warrant further evaluation.
Electronic health record (EHR) data are becoming more readily available and may serve as an additional data resource in the future. EHR data may provide access to timelier data that are able to reflect more real-time reporting of cancer data. However, evaluations of the strengths and limitations of EHR as surveillance tools may need to be addressed before these data are used routinely. Data modernization activities at CDC are currently reviewing the feasibility of more routine usage of EHR data.