Monitoring Selected National HIV Prevention and Care Objectives By Using HIV Surveillance Data United States and 6 Dependent Areas, 2019: Figures
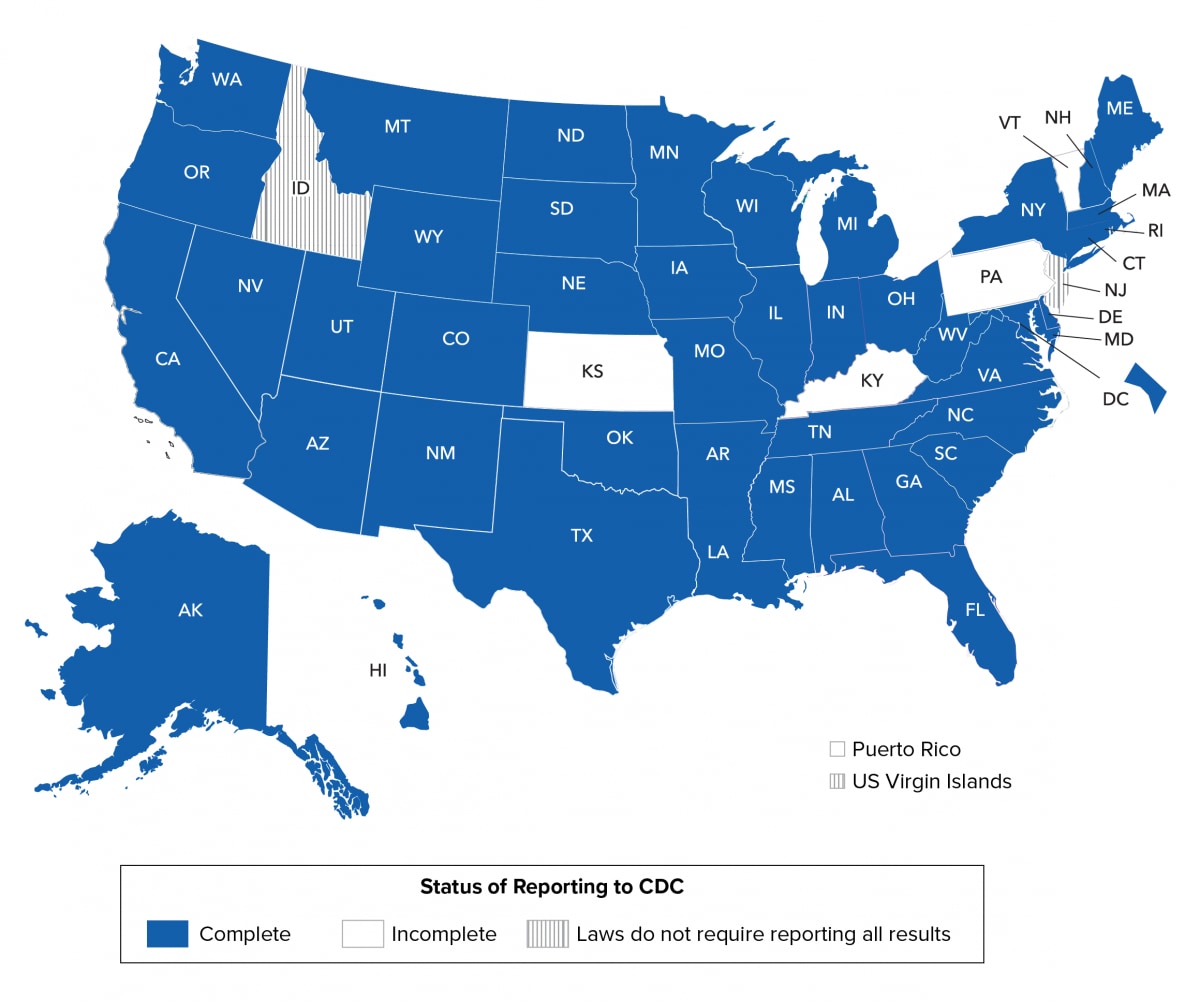
Note. See Technical Notes for more information on areas with complete laboratory reporting.
![cdc-hiv-surveillance-vol26-no-2-2 Among 33,795 persons with an HIV diagnosis during 2019, in 45 jurisdictions with complete laboratory reporting, the stage of disease at time of diagnosis was classified as follows: stage 0 (7.9%), stage 1 (25.9%), stage 2 (30.7%), stage 3 (AIDS) (20.2%), and stage unknown (15.3%). A higher percentage of persons had HIV diagnosed at an earlier stage (stage 0, 1, or 2: 64.5%) than at the late stage (stage 3 [AIDS]: 20.2%).](/hiv/images/library/reports/hiv-surveillance/vol-26-no-2/cdc-hiv-surveillance-vol26-no-2-2-large.png?_=55247)
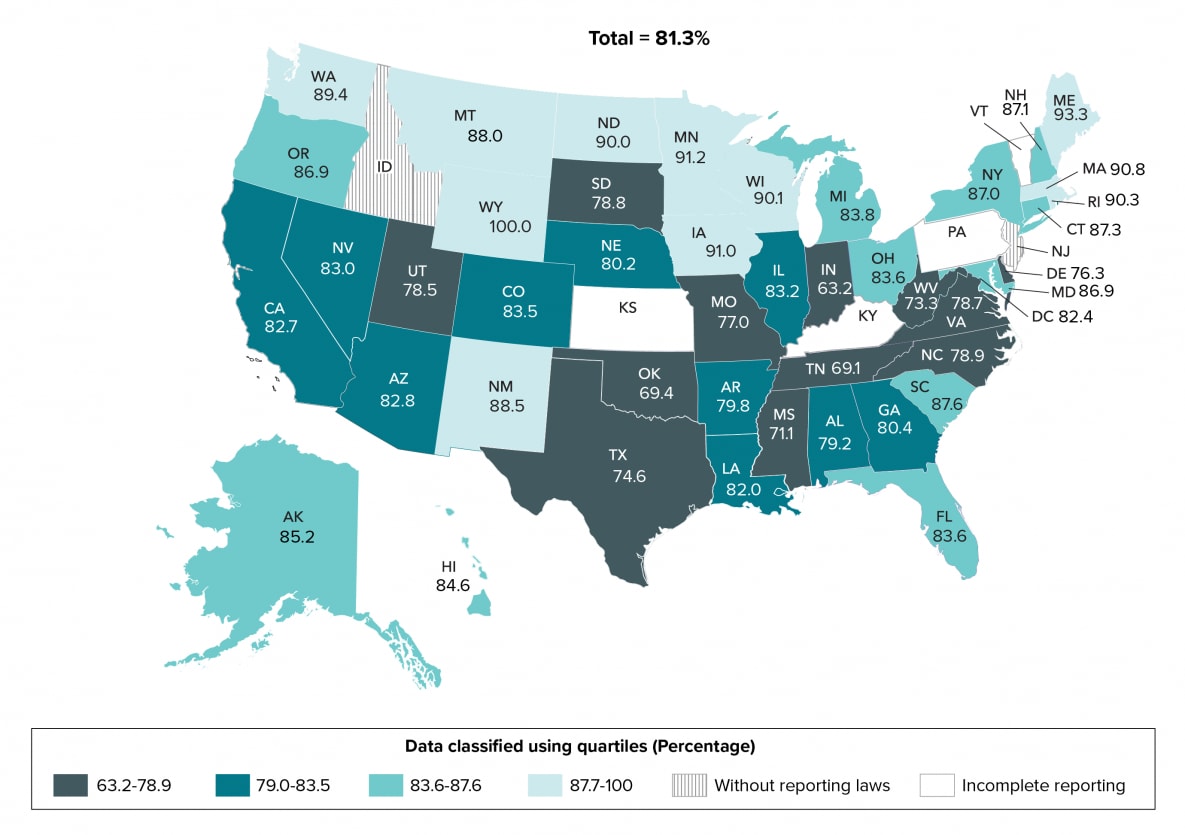
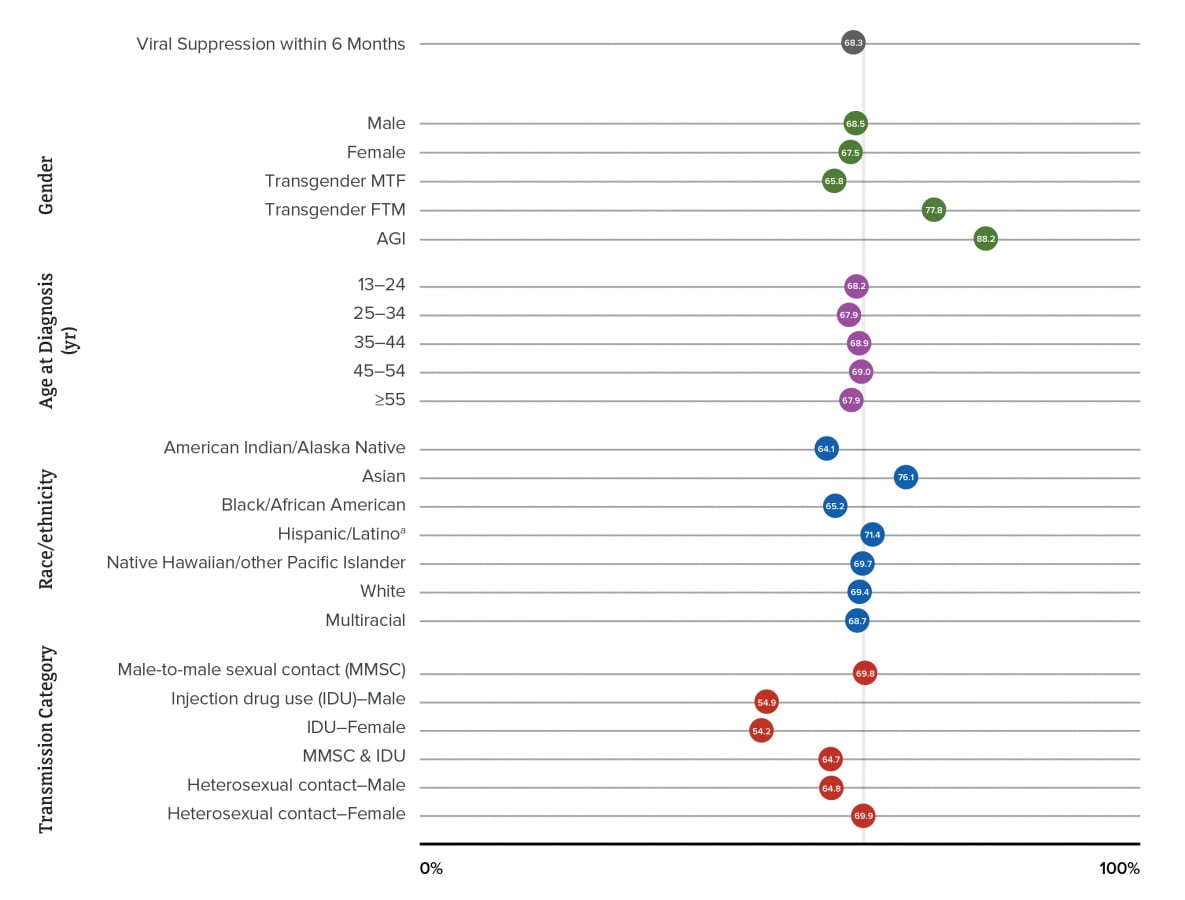
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
![cdc-hiv-surveillance-vol26-no-2-3 The highest percentage for persons whose infection was diagnosed at an earlier stage (stage 0, 1, or 2) by selected characteristics was for persons of AGI, transgender FTM persons, persons aged 13–24 at time of diagnosis, American Indian or Alaska Native persons, males with infection attributed to male-to-male sexual contact and injection drug use (MMSC-IDU), and males with infection attributed to MMSC. The highest percentage for persons whose infection was diagnosed at a late stage (stage 3 [AIDS]) by selected characteristics was for females, males, persons aged ≥45 years at time of diagnosis (45–54 years: 31.3%, ≥55 years: 34.4%), Asian persons, and males with infection attributed to heterosexual contact.](/hiv/images/library/reports/hiv-surveillance/vol-26-no-2/cdc-hiv-surveillance-vol26-no-2-3-large.png?_=55300)
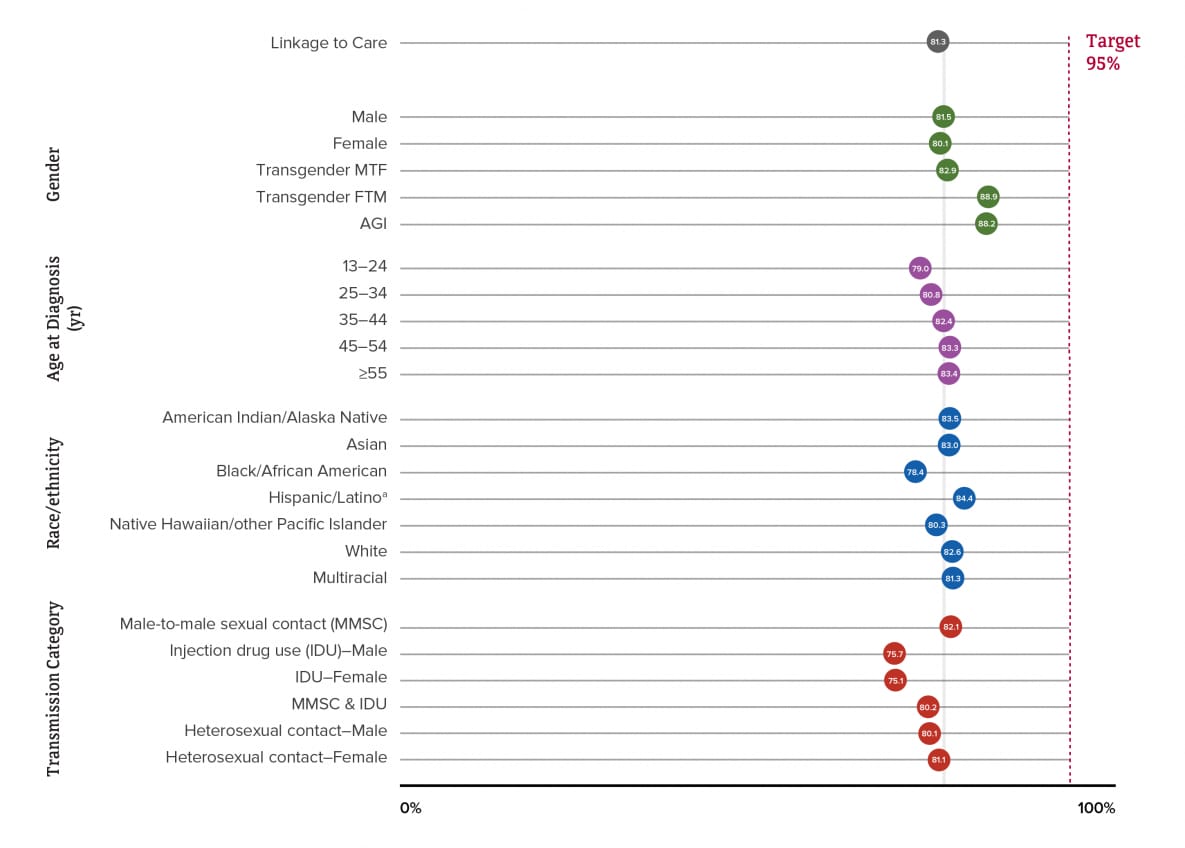
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
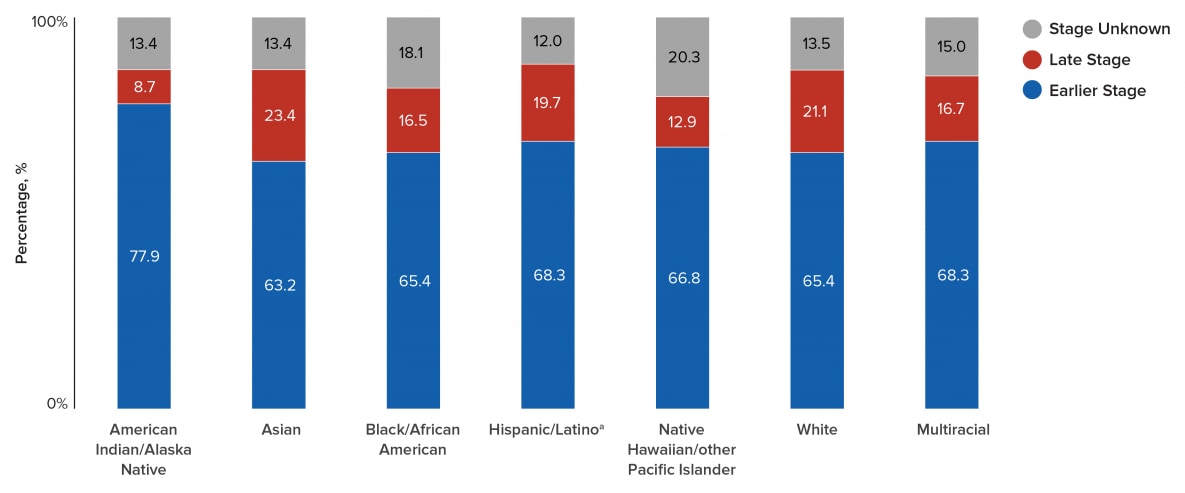
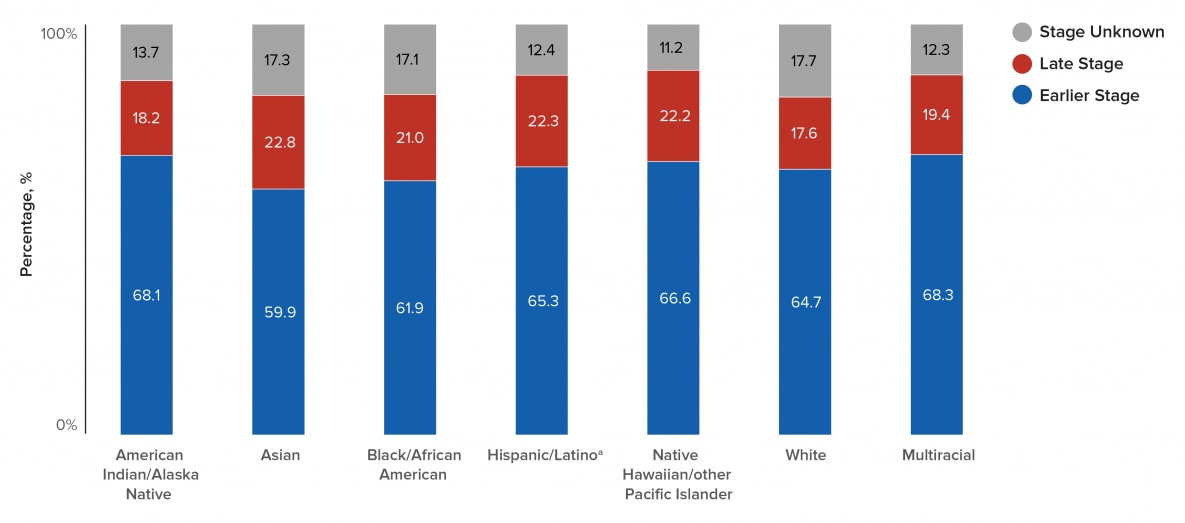
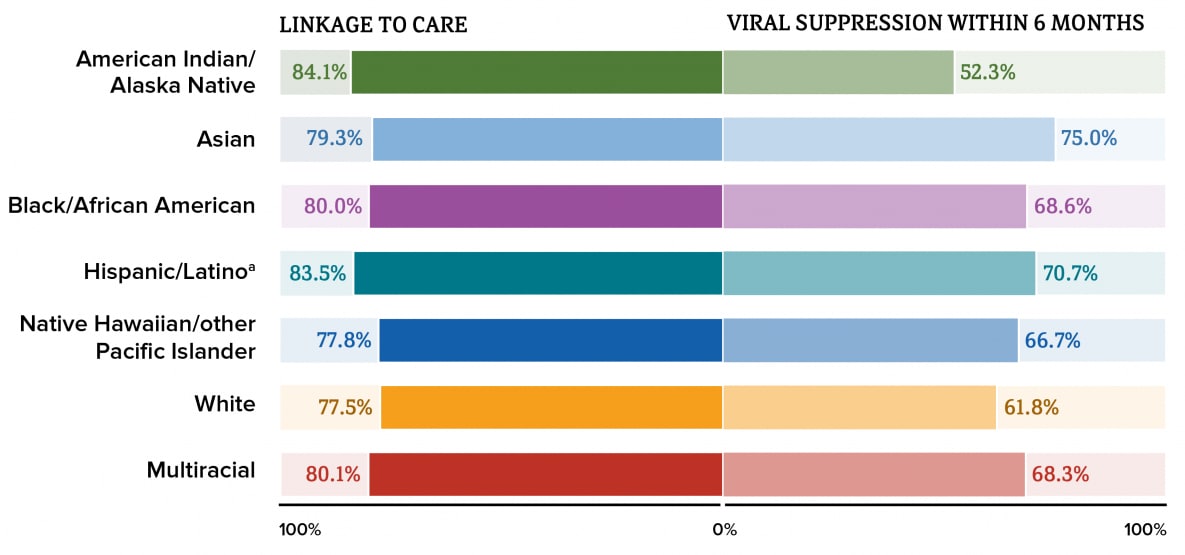
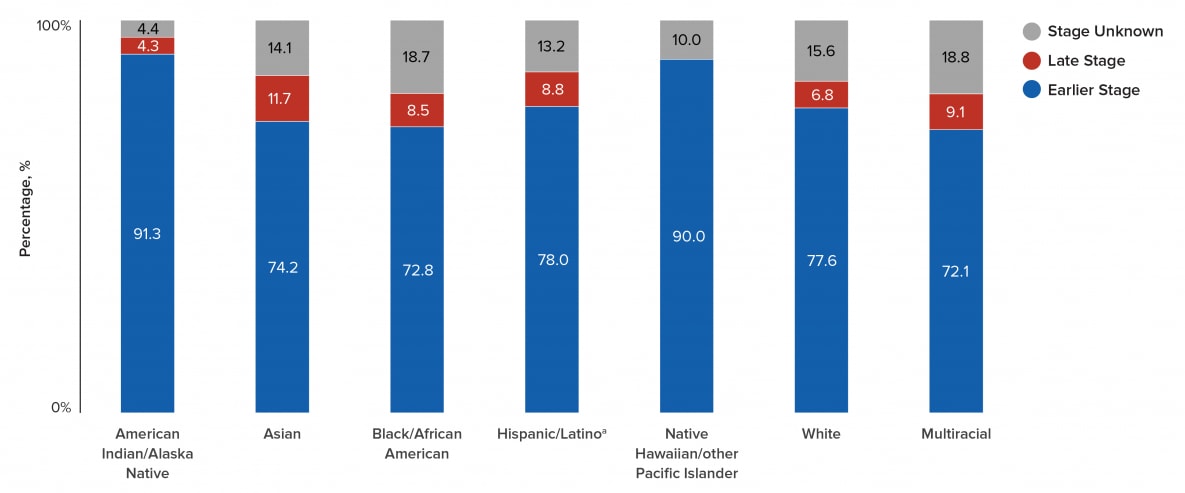
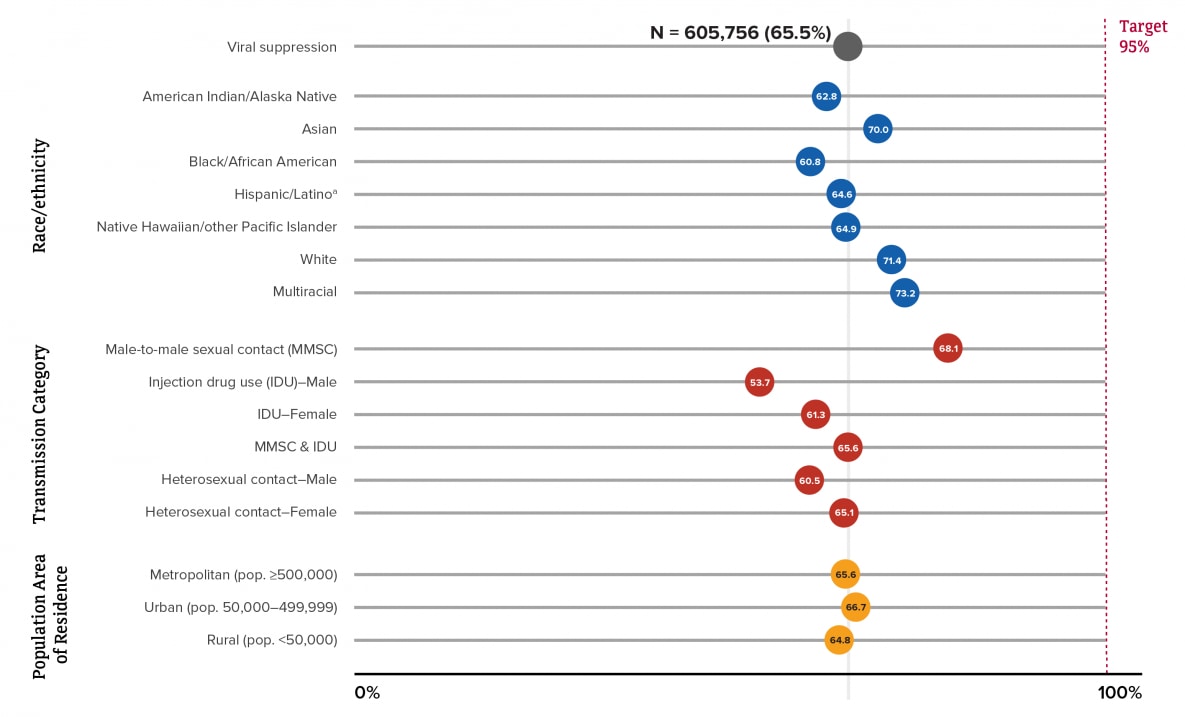
aHispanic/Latino persons can be of any race.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
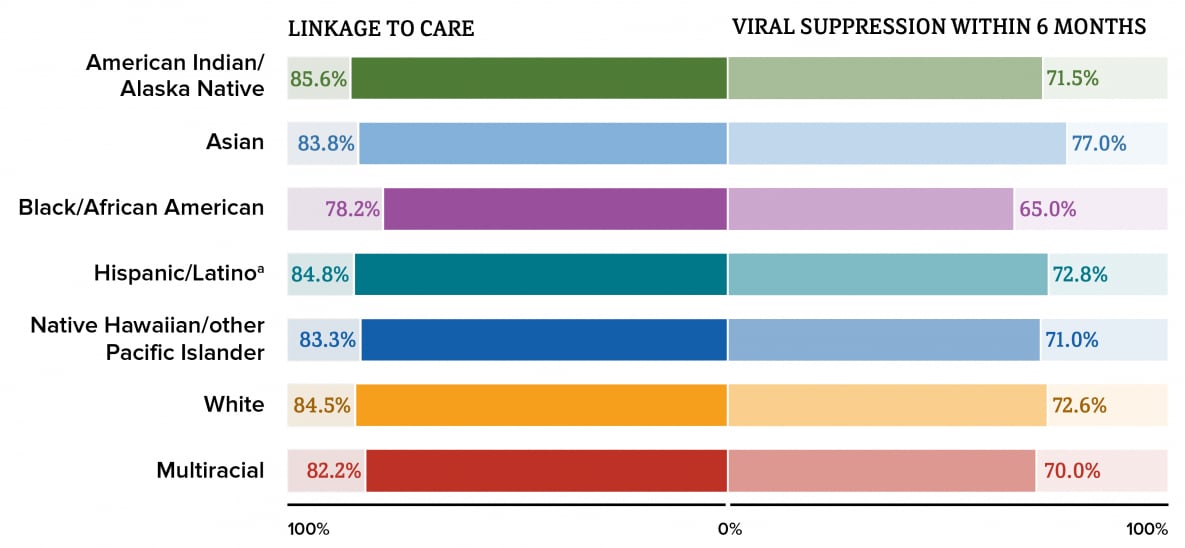
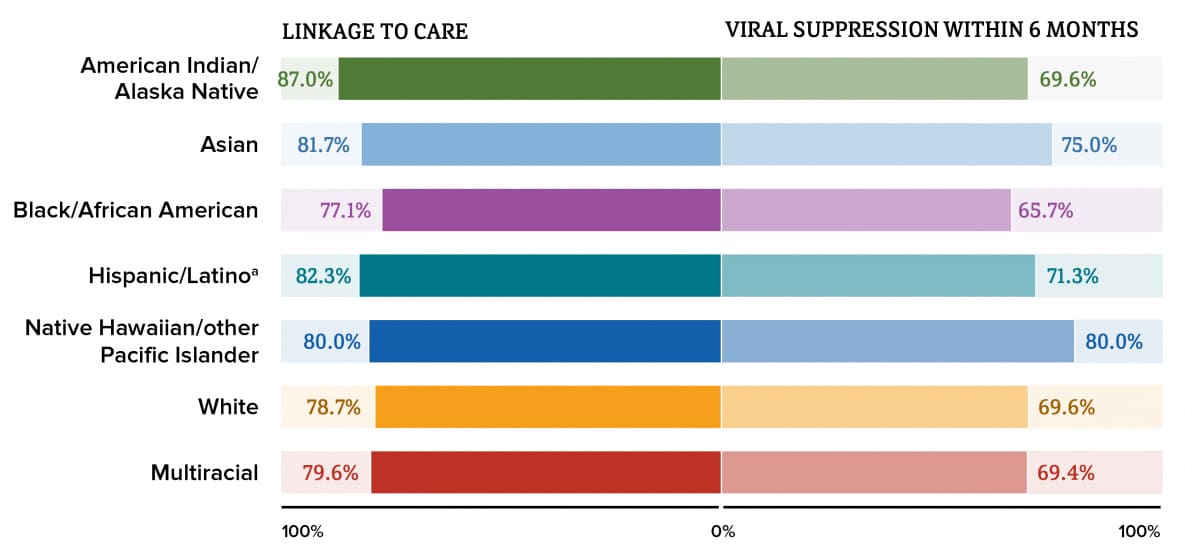
aHispanic/Latino persons can be of any race.
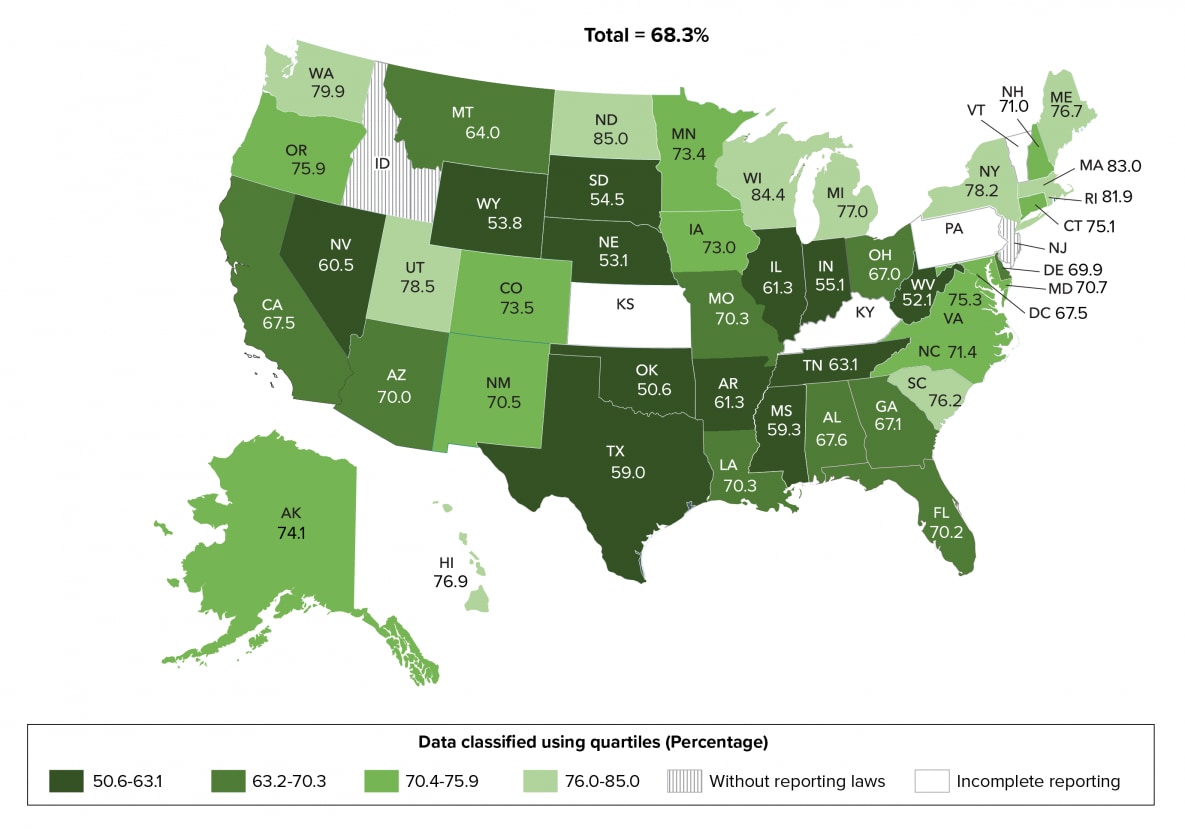
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
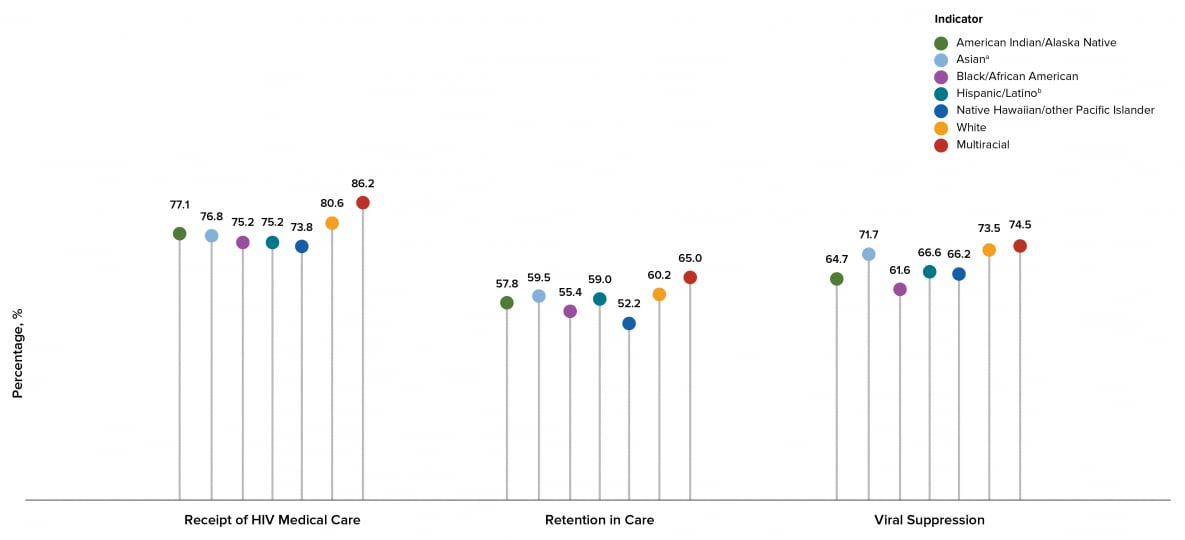
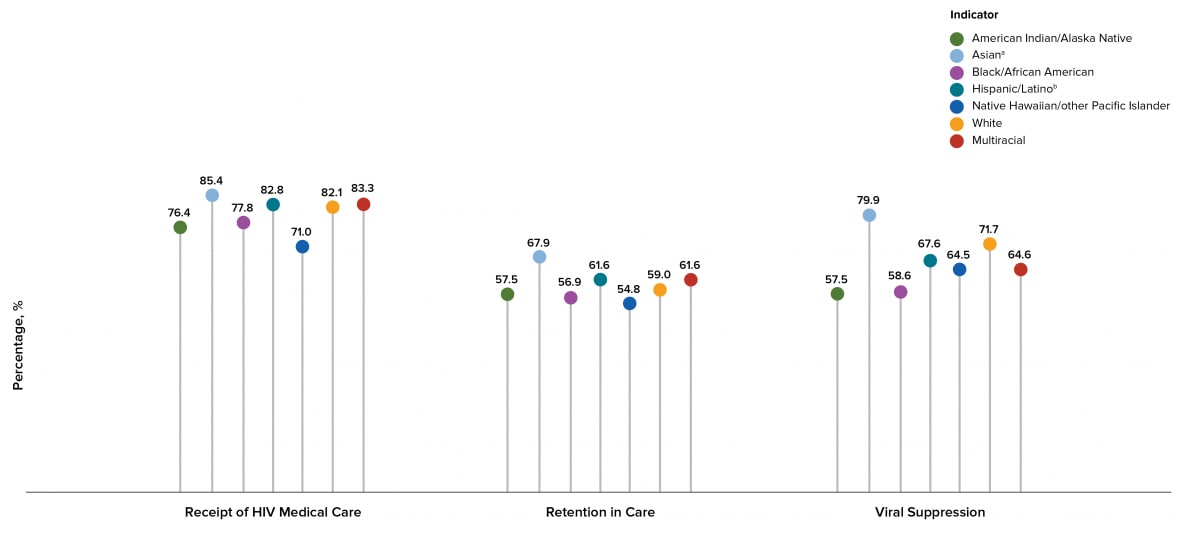
aHispanic/Latino persons can be of any race.
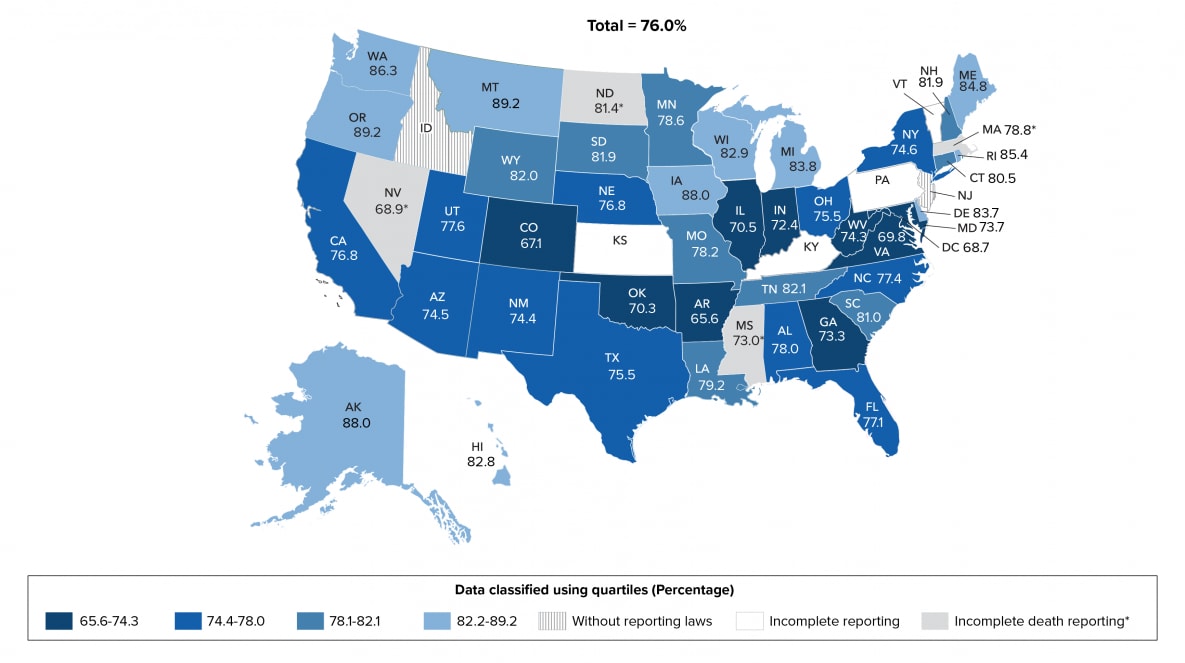
Note. Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020.
See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
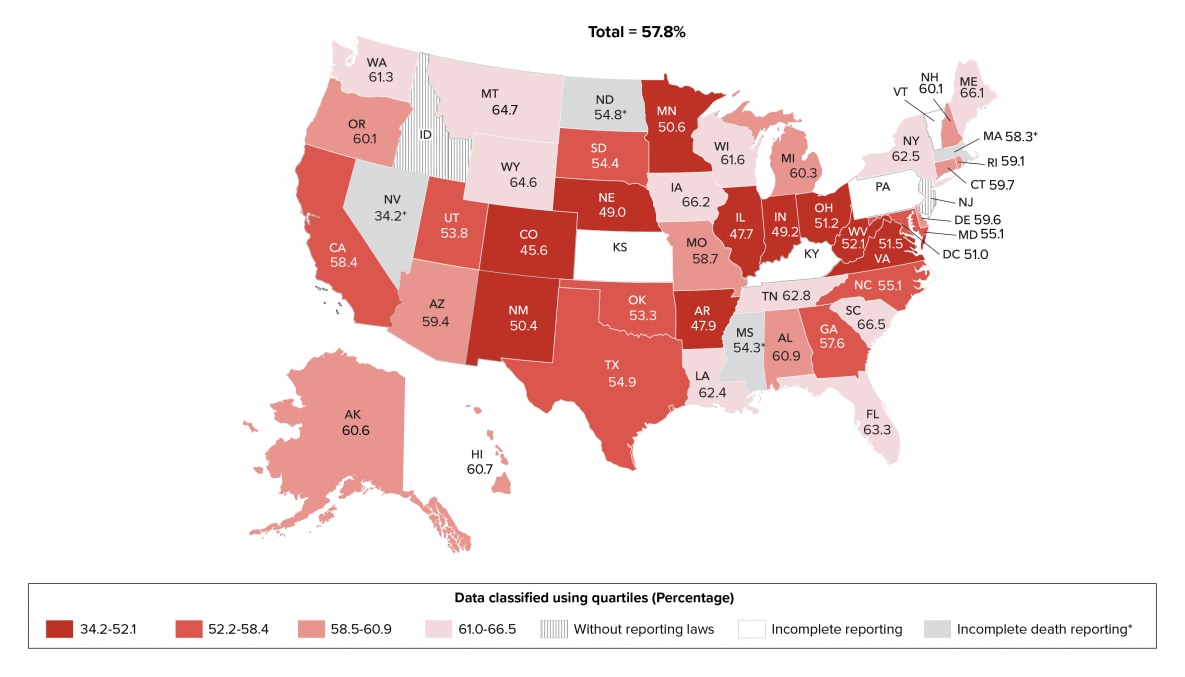
Note. Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020.
See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
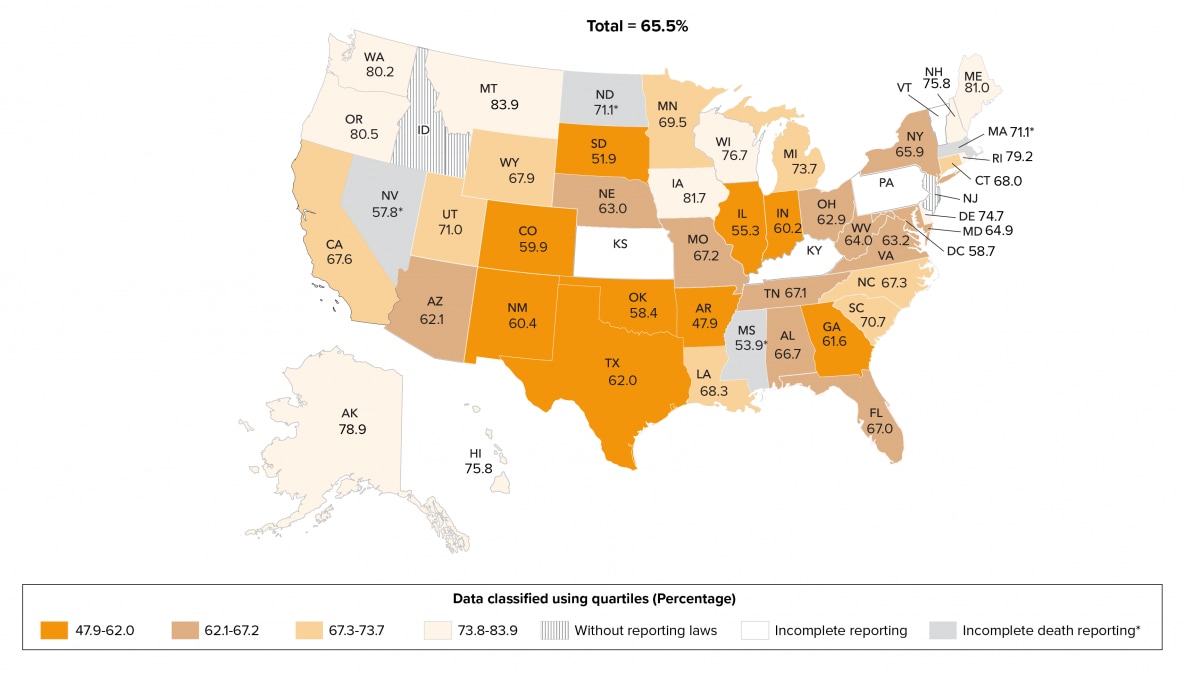
Note. Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020.
See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
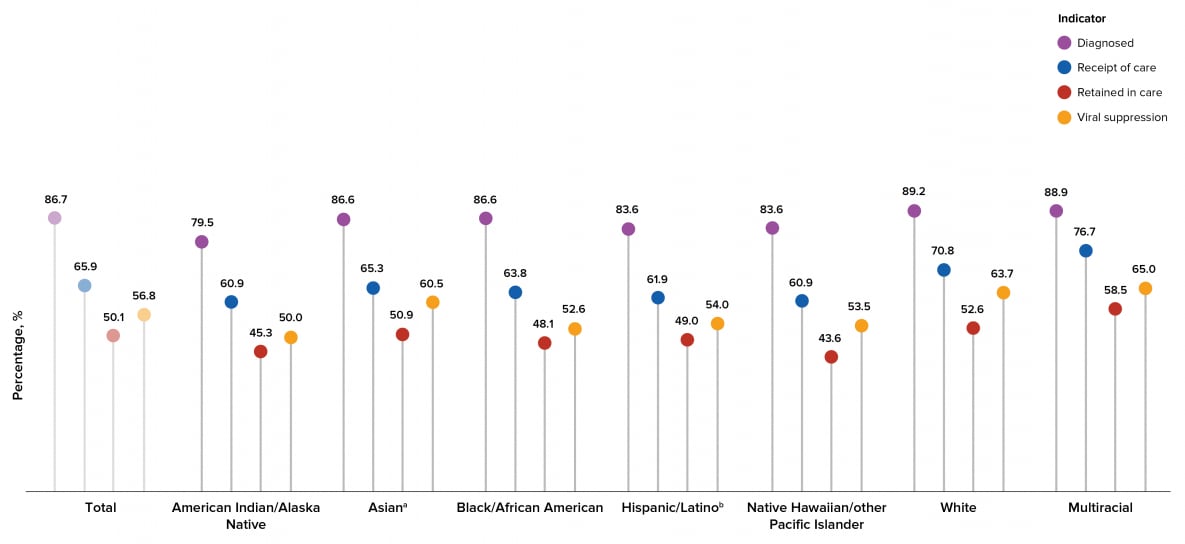
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
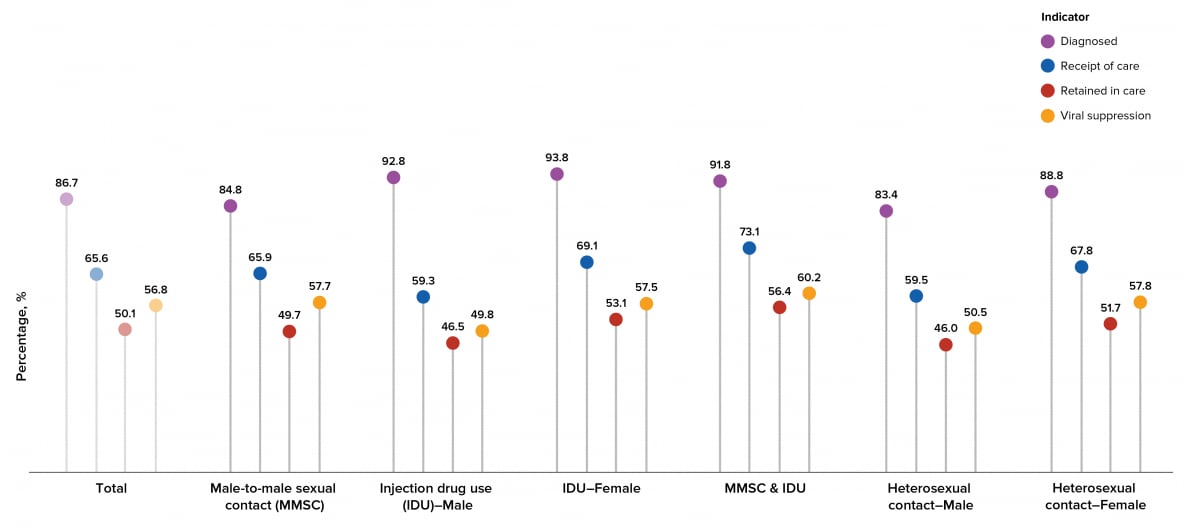
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
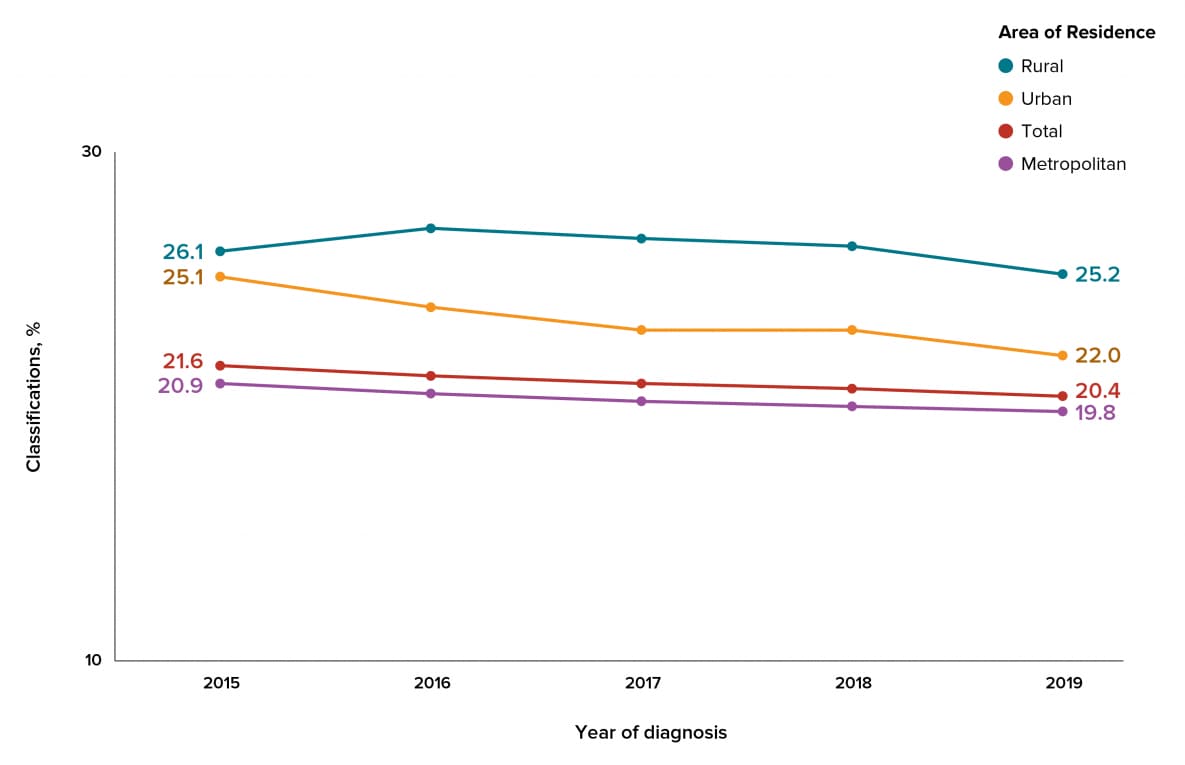
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
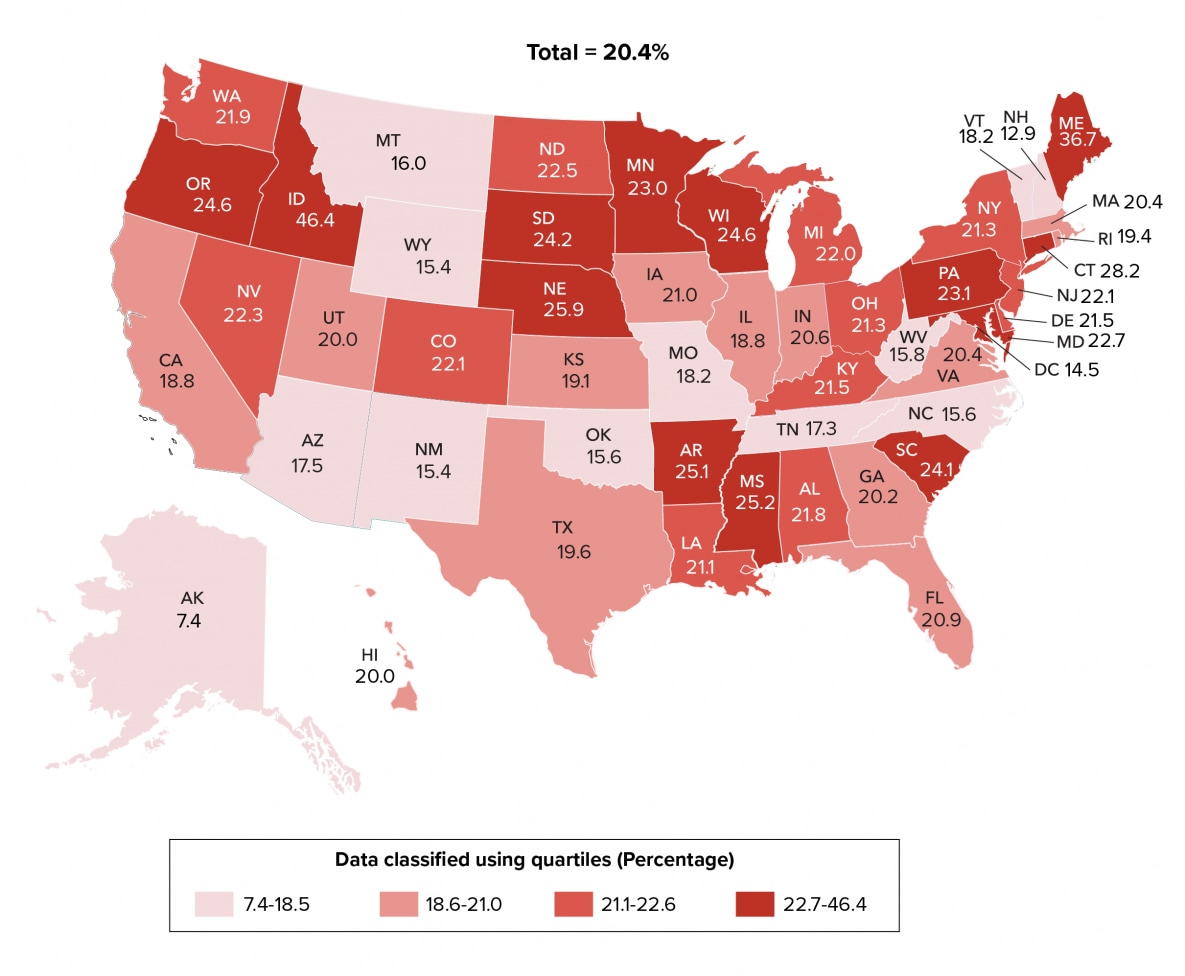
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.

Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
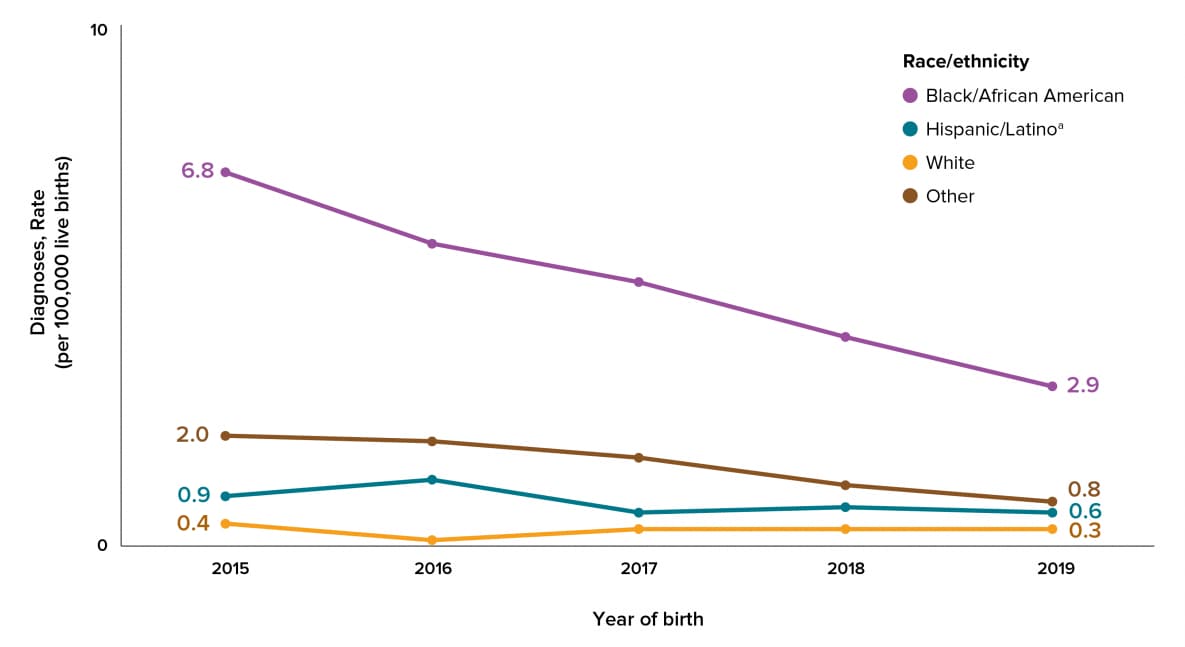
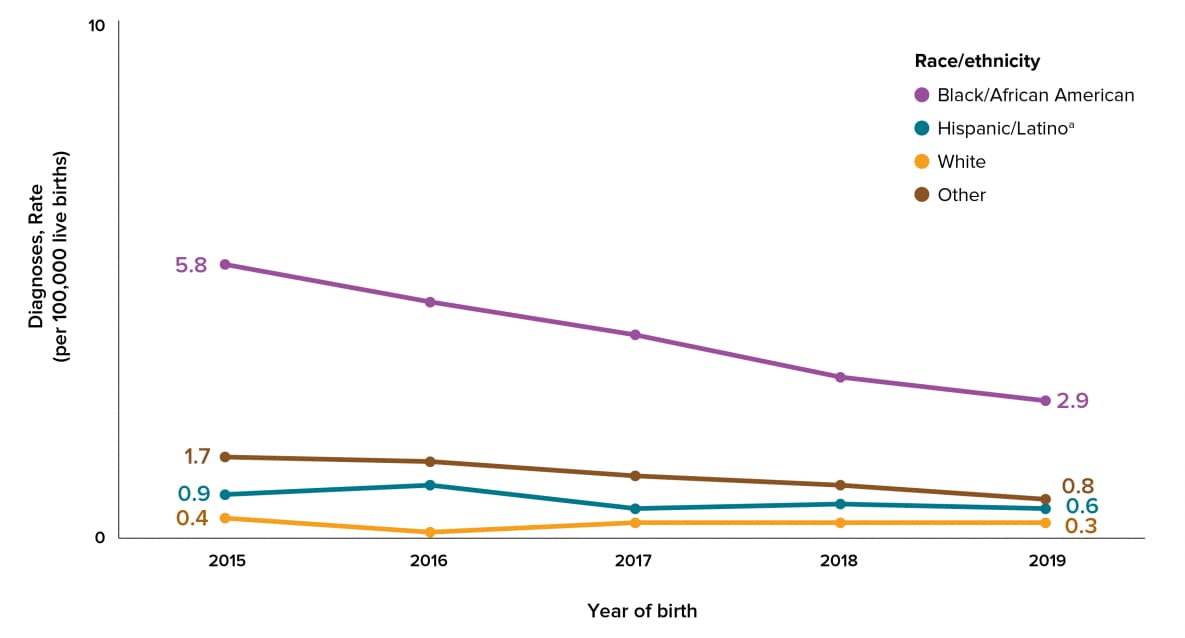
aHispanic/Latino persons can be of any race.
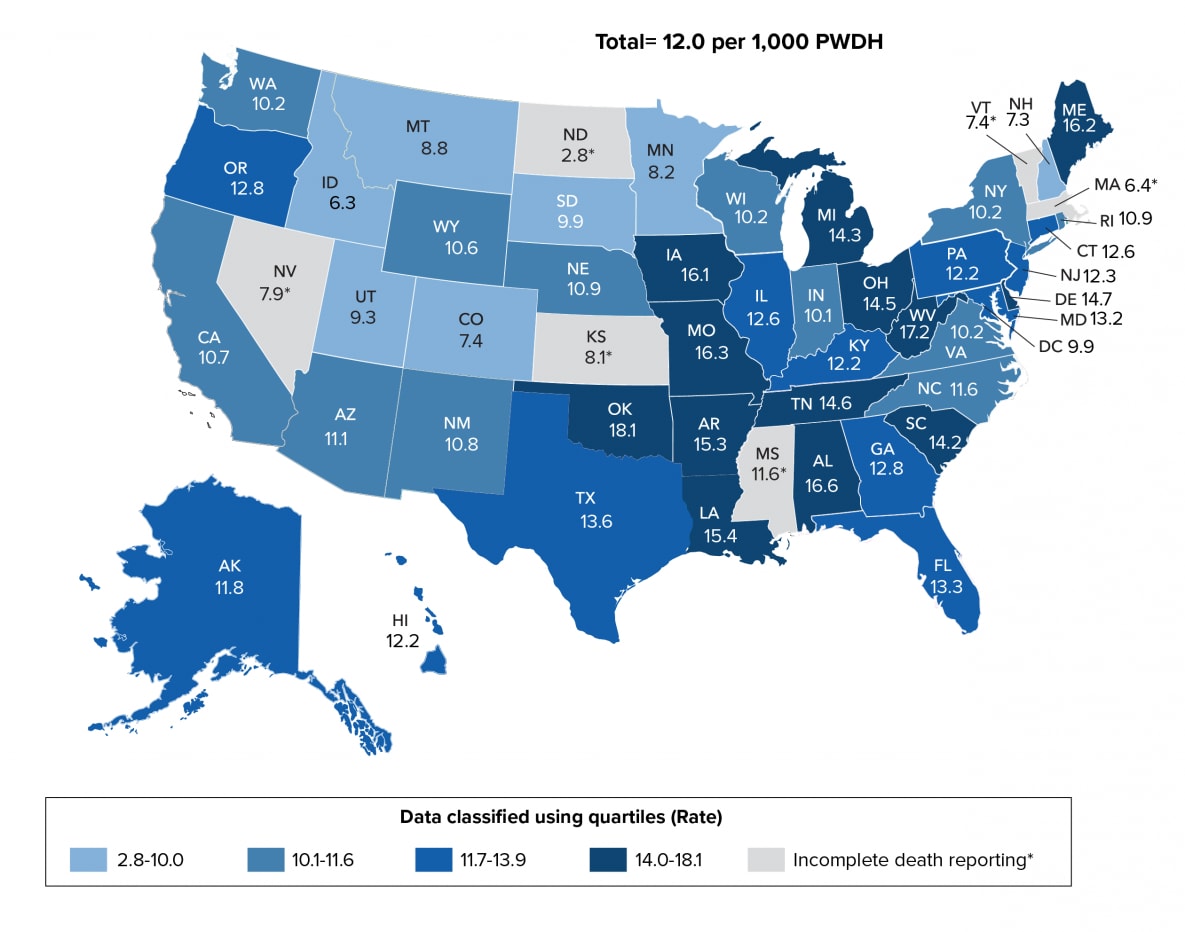
Note. Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020. Rates per 1,000 persons with diagnosed HIV infection. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
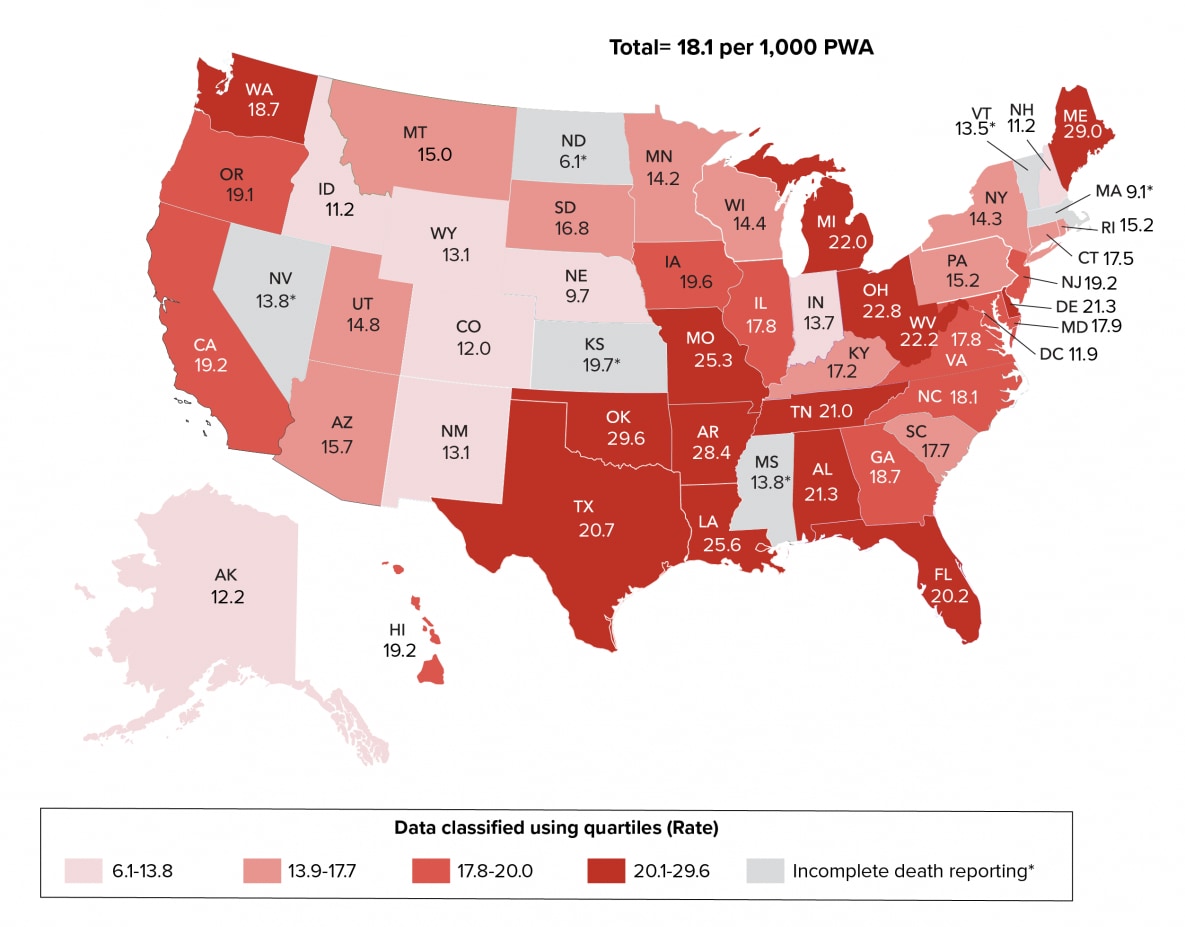
Note. Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020. Rates per 1,000 persons with diagnosed HIV infection ever classified as stage 3 (AIDS). See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
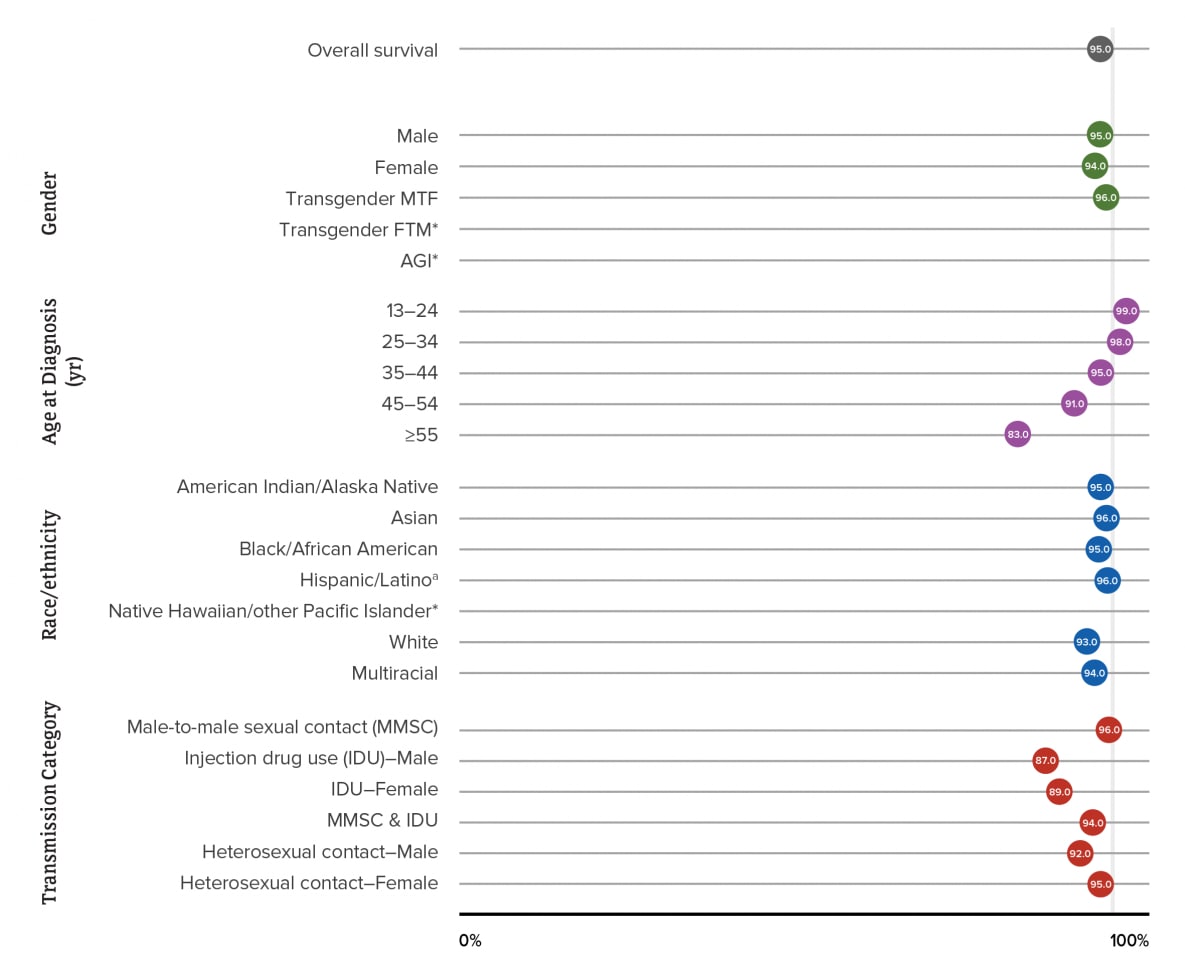
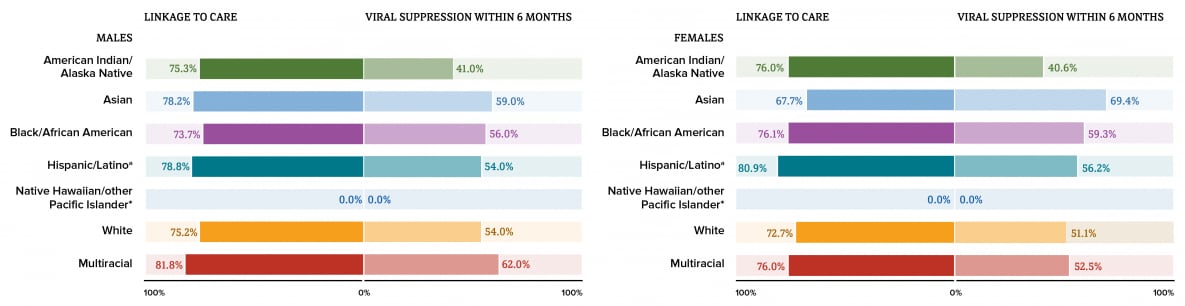
Note. Asterisk (*) indicates sample too small (<600 diagnoses during the 6-year period) for the calculation of meaningful survival estimates. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
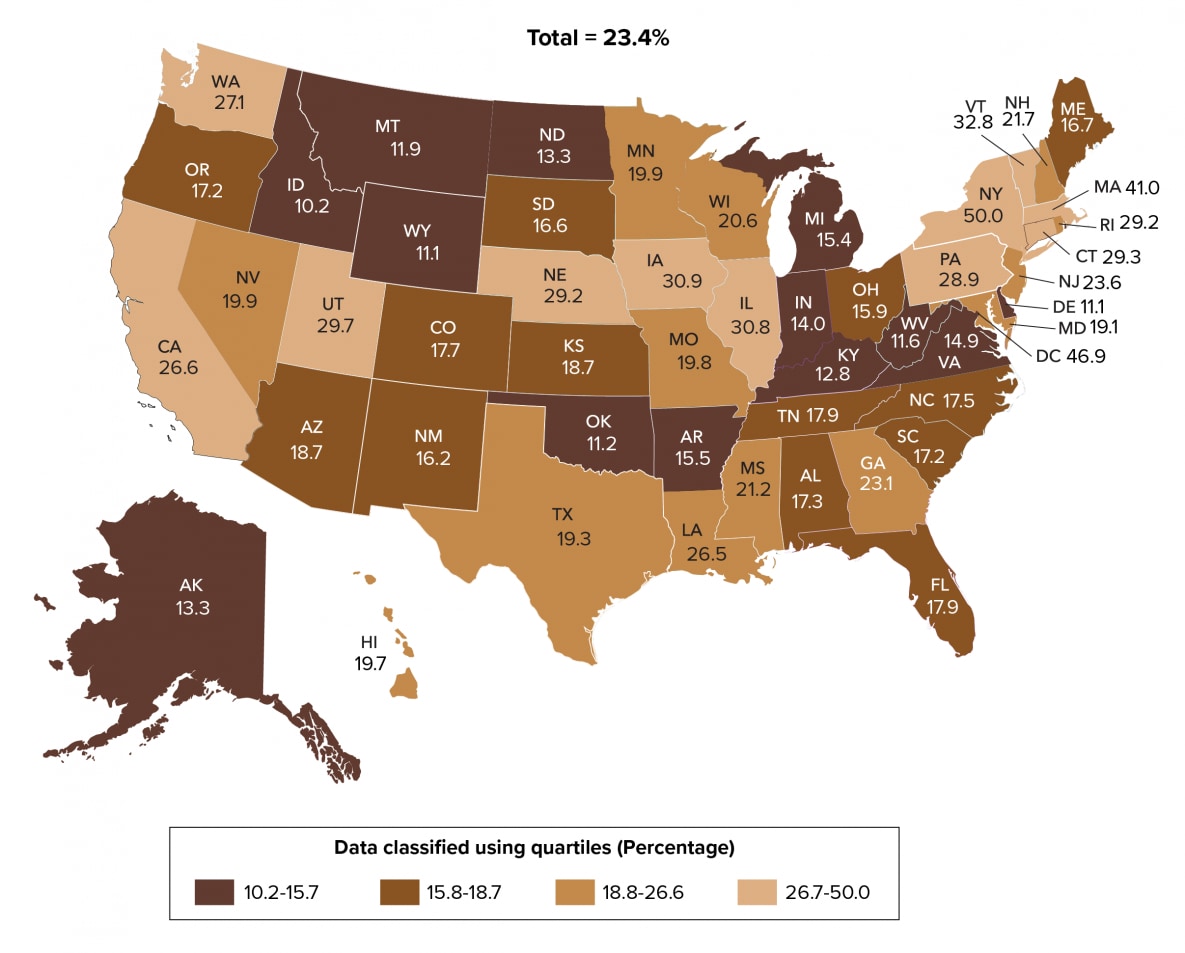
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
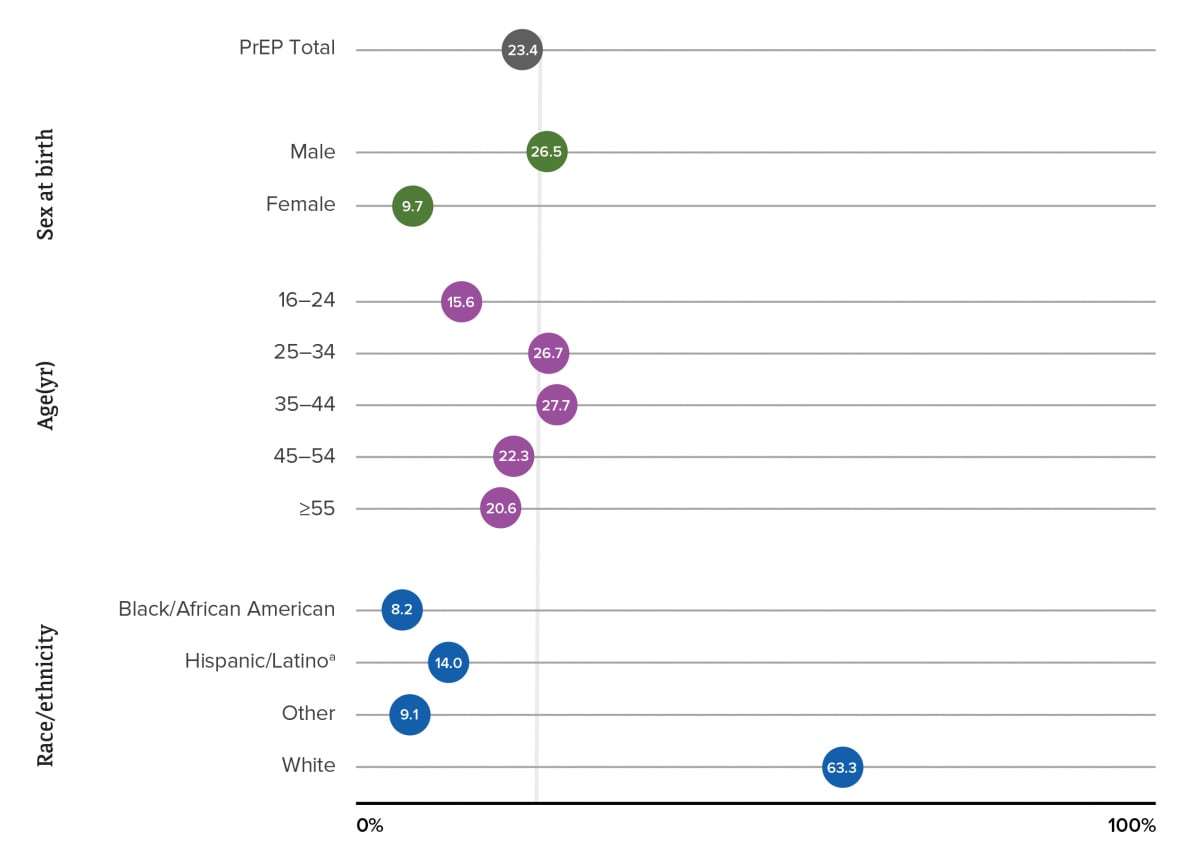
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications. Race/ethnicity data were only available for < 40% of persons prescribed PrEP in each year. Number prescribed PrEP and PrEP coverage for race/ethnicity reported in the table were adjusted applying the distribution of records with known race/ethnicity to records with missing race/ethnicity.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.

Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
*No cases diagnosed among this group.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
*No cases diagnosed among this group.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
Note. See Guide to Acronyms and Initialisms, Data Tables, and Technical Notes for more information on definitions and data specifications.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
Note. See Guide on Acronyms and Initialisms, Data Tables, and Technical Notes for more information on Definitions and Data Specifications.
aHispanic/Latino persons can be of any race.
