At a glance
Current best practices for environmental cleaning procedures in patient care areas, as well as cleaning for specific situations (e.g., blood spills) and for noncritical patient care equipment.
Overview
For use in global healthcare facilities
This chapter provides the current best practices for environmental cleaning procedures in patient care areas, as well as cleaning for specific situations (e.g., blood spills) and for noncritical patient care equipment; see summary in Appendix B1 – Cleaning procedure summaries for general patient areas and Appendix B2 – Cleaning procedure summaries for specialized patient areas.
The determination of environmental cleaning procedures for individual patient care areas, including frequency, method, and process, should be based on the risk of pathogen transmission.
This risk is a function of the:
- Probability of contamination.
- Vulnerability of the patients to infection.
- Potential for exposure (i.e., high-touch vs low-touch surfaces).
These three elements combine to determine low, moderate, and high risk—more frequent and rigorous (with a different method or process) environmental cleaning is required in areas with high risk. Risk determines cleaning frequency, method, and process in routine and contingency cleaning schedules for all patient care areas. This risk-based approach is outlined in Appendix A – Risk-assessment for determining environmental cleaning method and frequency.
Risk-based environmental cleaning frequency principles
Probability of contamination: Heavily contaminated surfaces and items require more frequent and thorough environmental cleaning than moderately contaminated surfaces, which in turn require more frequent and rigorous environmental cleaning than lightly or non-contaminated surfaces and items.
Vulnerability of patients to infection: Surfaces and items in care areas containing vulnerable patients (e.g., immunosuppressed) require more frequent and rigorous environmental cleaning than surfaces and items in areas with less vulnerable patients.
Potential for exposure to pathogens: High-touch surfaces (e.g., bed rails) require more frequent and rigorous environmental cleaning than low-touch surfaces (e.g., walls).
Every facility should develop cleaning schedules, including:
- Identifying the person responsible.
- The frequency.
- The method (product, process).
- Detailed SOPs for environmental cleaning of surfaces and noncritical equipment in every type of patient care area.
Checklists and other job aids are also required to ensure that cleaning is thorough and effective.
These aspects are covered in more detail in 2.4.3 Cleaning checklists, logs, and job aids.
4.1 General environmental cleaning techniques
For all environmental cleaning procedures, always use the following general strategies:
Conduct visual preliminary site assessment
Proceed only after a visual preliminary site assessment to determine if:
- Patient status could pose a challenge to safe cleaning.
- There is any need for additional PPE or supplies (e.g., if there are any spills of blood/body fluids or if the patient is on transmission-based precautions).
- There are any obstacles (e.g., clutter) or issues that could pose a challenge to safe cleaning.
- There is any damaged or broken furniture or surfaces to be reported to supervisor/management.
Proceed from cleaner to dirtier
Proceed from cleaner to dirtier areas to avoid spreading dirt and microorganisms. Examples include:
- During terminal cleaning, clean low-touch surfaces before high-touch surfaces.
- Clean patient areas (e.g., patient zones) before patient toilets.
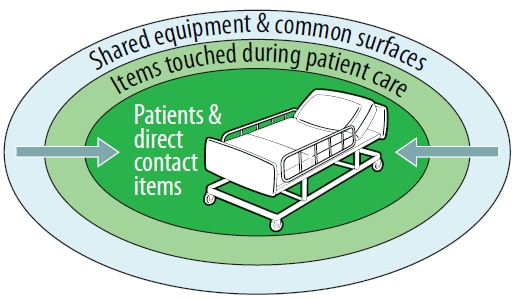
- Within a specified patient room, terminal cleaning should start with shared equipment and common surfaces, then proceed to surfaces and items touched during patient care that are outside of the patient zone, and finally to surfaces and items directly touched by the patient inside the patient zone (Figure 9). In other words, high-touch surfaces outside the patient zone should be cleaned before the high-touch surfaces inside the patient zone.
- Clean general patient areas not under transmission-based precautions before those areas under transmission-based precautions.
Proceed from high to low (top to bottom)
Proceed from high to low to prevent dirt and microorganisms from dripping or falling and contaminating already cleaned areas. Examples include:
- Cleaning bed rails before bed legs.
- Cleaning environmental surfaces before cleaning floors.
- Cleaning floors last to allow collection of dirt and microorganisms that may have fallen.
Proceed in a methodical, systematic manner
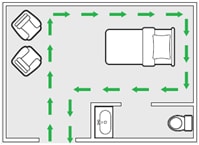
Proceed in a systematic manner to avoid missing areas—for example, left to right or clockwise (Figure 10).
In a multi-bed area, clean each patient zone in the same manner—for example, starting at the foot of the bed and moving clockwise.
Immediately attend to body fluid spills
Clean spills of blood or body fluids immediately, using the techniques in 4.5 Spills of blood or body fluids.
This is the general surface cleaning process:
- Thoroughly wet (soak) a fresh cleaning cloth in the environmental cleaning solution.
- Fold the cleaning cloth in half until it is about the size of your hand. This will ensure that you can use all of the surface area efficiently (generally, fold them in half, then in half again, and this will create 8 sides).
- Wipe surfaces using the general strategies as above (e.g., clean to dirty, high to low, systematic manner), making sure to use mechanical action (for cleaning steps) and making sure to that the surface is thoroughly wetted to allow required contact time (for disinfection steps).
- Regularly rotate and unfold the cleaning cloth to use all of the sides.
- When all of the sides of the cloth have been used or when it is no longer saturated with solution, dispose of the cleaning cloth or store it for reprocessing.
- Repeat process from step 1.
For all environmental cleaning procedures, these are the best practices for environmental cleaning of surfaces:
- Use fresh cleaning cloths at the start of each cleaning session (e.g., routine daily cleaning in a general inpatient ward).
- Change cleaning cloths when they are no longer saturated with solution, for a new, wetted cloth. Soiled cloths should be stored for reprocessing.
- For higher-risk areas, change cleaning cloths between each patient zone (i.e., use a new cleaning cloth for each patient bed). For example, in a multi-bed intensive unit, use a fresh cloth for every bed/incubator—see 4.6 Specialized patient areas for more guidance.
- Ensure that there are enough cleaning cloths to complete the required cleaning session.
- Never double-dip cleaning cloths into portable containers (e.g., bottles, small buckets) used for storing environmental cleaning products (or solutions).
- Never shake mop heads and cleaning cloths—it disperses dust or droplets that could contain microorganisms.
- Never leave soiled mop heads and cleaning cloths soaking in buckets.
High-touch surfaces
The identification of high-touch surfaces and items in each patient care area is a necessary prerequisite to the development of cleaning procedures, as these will often differ by room, ward and facility. See Appendix C – Example of high-touch surfaces in a specialized patient area. Perform assessments and observations of workflow in consultation with clinical staff in each patient care area to determine key high-touch surfaces.
Include identified high-touch surfaces and items in checklists and other job aids to facilitate completing cleaning procedures. See 2.4.3 Cleaning checklists, logs, and job aids.
Common high-touch surfaces include:
- Bedrails
- IV poles
- Sink handles
- Bedside tables
- Counters where medications and supplies are prepared
- Edges of privacy curtains
- Patient monitoring equipment (e.g., keyboards, control panels)
- Transport equipment (e.g., wheelchair handles)
- Call bells
- Doorknobs
- Light switches
4.2 General patient areas
General patient areas include:
- Outpatient or ambulatory care wards.
- General inpatient wards with patients admitted for medical procedures, who are not receiving acute care (i.e., sudden, urgent or emergent episodes of injury and illness that require rapid intervention).
Three types of cleaning are required for these areas:
- Routine cleaning.
- Terminal cleaning.
- Scheduled cleaning.
Generally, the probability of contamination or the vulnerability of the patients to infection is low, so these areas may require less frequent and rigorous (e.g., method, process) cleaning than specialized patient areas.
4.2.1 Outpatient wards
General outpatient or ambulatory care wards include waiting areas, consultation areas, and minor procedural areas.
Table 6. Recommended Frequency, Method and Process for Outpatient Wards
| Area | Frequency | Method | Process |
|---|---|---|---|
| Waiting / Admission | At least once daily (e.g., per 24-hour period) | Clean | High-touch surfaces and floors |
| Consultation / Examination | At least twice daily | Clean | High-touch surfaces and floors |
| Procedural (minor operative procedures; e.g., suturing wounds, draining abscesses) | Before and after (i.e., between [Footnote e]) each procedure
Footnote e: |
Clean and disinfect | High-touch surfaces and floors, with an emphasis on the patient zone, procedure table |
| Procedural (minor operative procedures; e.g., suturing wounds, draining abscesses) | End of the day (terminal clean) | Clean and disinfect | All surfaces and the entire floor
Handwashing sinks, thoroughly clean (scrub) and disinfect Sluice areas/sinks or scrub areas |
| All | Scheduled basis (e.g., weekly, monthly) and when visibly soiled | Clean | Low-touch surfaces; see 4.2.4 Scheduled cleaning |
4.2.2 Routine cleaning of inpatient wards
Routine cleaning of inpatient areas occurs while the patient is admitted, focuses on the patient zones and aims to remove organic material and reduce microbial contamination to provide a visually clean environment.
Note: This occurs when the room is occupied, and systems should be established to ensure that cleaning staff have reasonable access to perform routine cleaning.
Table 7. Recommended Frequency, Method and Process for Routine Cleaning of Inpatient Wards
| Frequency | Method | Process |
|---|---|---|
| At least once daily (e.g., per 24-hour period) | Clean | High-touch surfaces and floors
Handwashing sinks |
| Scheduled basis (e.g., weekly) and when visibly soiled | Clean | Low-touch surfaces; see 4.2.4 Scheduled cleaning |
4.2.3 Terminal or discharge cleaning of inpatient wards
Terminal cleaning of inpatient areas, which occurs after the patient is discharged/transferred, includes the patient zone and the wider patient care area and aims to remove organic material and significantly reduce and eliminate microbial contamination to ensure that there is no transfer of microorganisms to the next patient.
Terminal cleaning requires collaboration between cleaning, IPC, and clinical staff to delineate responsibility for every surface and item, including ensuring that:
- Disposable personal care items are discarded.
- Patient care equipment is removed for reprocessing.
It is important that the staff responsible for these tasks are identified in checklists and SOPs to ensure that items are not overlooked because of confusion in responsibility.
Table 8. Recommended Frequency, Method and Process for Terminal Cleaning of Inpatient Wards
| Frequency | Method | Process |
|---|---|---|
| Patient transfer or discharge | Clean and disinfect | See general terminal cleaning process below |
This is the general terminal cleaning process:
- Remove soiled/used personal care items (e.g., cups, dishes) for reprocessing or disposal.
- Remove facility-provided linens for reprocessing or disposal. See Appendix D – Linen and laundry management.
- Inspect window treatments. If soiled, clean blinds on-site, and remove curtains for laundering.
- Reprocess all reusable (noncritical) patient care equipment; see 4.7 Noncritical patient care equipment.
- Clean and disinfect all low- and high-touch surfaces, including those that may not be accessible when the room/area was occupied (e.g., patient mattress, bedframe, tops of shelves, vents), and floors.
- Clean (scrub) and disinfect handwashing sinks.
4.2.4 Scheduled cleaning
Scheduled cleaning occurs concurrently with routine or terminal cleaning and aims to reduce dust and soiling on low touch items or surfaces. Perform scheduled cleaning on items or surfaces that are not at risk for soiling under normal circumstances, using neutral detergent and water. But if they are visibly soiled with blood or body fluids, clean and disinfect these items as soon as possible.
Table 9. Recommended Frequency, Method and Process for Scheduled Cleaning of Inpatient Wards
| Frequency | Method | Process |
|---|---|---|
| Weekly | Clean | High surfaces (above shoulder height) such as tops of cupboards, vents
Walls, baseboards and corners |
| Monthly | See Appendix D – Linen and laundry management | Window blinds, bed curtains |
| Annually | See Appendix D – Linen and laundry management | Window curtains |
4.3 Patient area toilets
Toilets in patient care areas can be private (within a private patient room) or shared (among patients and visitors). They have high patient exposure (i.e., high-touch surfaces) and are frequently contaminated. Therefore, they pose a higher risk of pathogen transmission than in general patient areas.
Cultural considerations
Toileting practices vary, in terms of both the types of toilets in use (e.g., squat or sit, wet or dry) and the adherence to correct use. Therefore, needs for cleaning and disinfection vary. In some cases, more than twice daily cleaning and disinfection may be warranted.
Depending on resource and staffing levels, dedicated cleaning staff posted at shared toilets in healthcare facilities could reduce risk associated with these areas.
Table 10. Recommended Frequency, Method and Process for Patient Area Toilets
| Area | Frequency | Method | Process |
|---|---|---|---|
| Private toilets | At least once daily (e.g., per 24-hour period), after routine cleaning of patient care area | Clean and disinfect | High-touch and frequently contaminated surfaces in toilet areas (e.g., handwashing sinks, faucets, handles, toilet seat, door handles) and floors |
| Public or shared toilets (e.g., patients, visitors, family members) | At least twice daily | Clean and disinfect | High-touch and frequently contaminated surfaces in toilet areas (e.g., handwashing sinks, faucets, handles, toilet seat, door handles) and floors |
| Both (private and shared) | Scheduled basis (e.g., weekly) and when visibly soiled | Clean | Low-touch surfaces; see 4.2.4 Scheduled cleaning |
4.4 Patient area floors
Floors generally have low patient exposure (i.e., are low-touch surfaces) and pose a low risk for pathogen transmission. Therefore, under normal circumstances they should be cleaned daily, but the use of a disinfectant is not necessary.
There are situations where there is higher risk associated with floors (e.g., high probability of contamination), so review the specific procedures in 4.2 General patient areas and 4.6 Specialized patient areas for guidance on frequency of environmental cleaning of floors and when they should also be disinfected.
Table 11. Recommended Frequency, Method and Process for Patient Area Floors
| Area | Frequency | Method | Process |
|---|---|---|---|
| Floors in general inpatient and outpatient areas, always cleaned last after other environmental surfaces | At least once daily (e.g., per 24-hour period) or as often as specified in the specific patient care area | Clean (unless otherwise specified within specific patient care area) | See general mopping process below |
This is the general mopping process:
- Immerse the mop or floor cloth in the bucket with environmental cleaning solution and wring out.
- Mop in a figure-8 pattern with overlapping strokes, turning the mop head regularly (e.g., every 5-6 strokes).
- After cleaning a small area (e.g., 3m x 3m), immerse the mop or floor cloth in the bucket with rinse water and wring out.
- Repeat process from step 1.
These are the best practices for environmental cleaning of general patient area floors:
- Use wet floor or caution signs to prevent injuries.
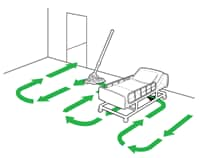
- Mop from cleaner to dirtier areas.
- Mop in a systematic manner, proceeding from area farthest from the exit and working towards the exit (Figure 11).
- Change mop heads/floor cloths and buckets of cleaning and disinfectant solutions as often as needed (e.g., when visibly soiled, after every isolation room, every 1-2 hours) and at the end of each cleaning session.
4.5 Spills of blood or body fluids
Regardless of the risk-level of an area, spills or contamination from blood or body fluid (e.g., vomitus), must be cleaned and disinfected immediately using a two-step process.
Table 12. Recommended Frequency, Method and Process for Spills of Blood or Body Fluids
| Area | Frequency | Method | Process |
|---|---|---|---|
| Any spill in any patient or non-patient area | Immediately, as soon as possible | Clean and disinfect:
|
See general process for cleaning of spills of blood or body fluids below |
This is the general process for cleaning of spills of blood or body fluids:
- Wear appropriate PPE. See Table 5 in 3.4 Cleaning Supplies and Equipment.
- Confine the spill and wipe it up immediately with absorbent (paper) towels, cloths, or absorbent granules (if available) that are spread over the spill to solidify the blood or body fluid (all should then be disposed as infectious waste).
- Clean thoroughly, using neutral detergent and warm water solution.
- Disinfect by using a facility-approved intermediate-level disinfectant.
- Typically, chlorine-based disinfectants at 500-5000ppm free chlorine (1:100 or 1:10 dilution of 5% chlorine-bleach; depending on the size of the spill) are adequate for disinfecting spills (however, do not use chlorine-based disinfectants on urine spills). See Appendix E – Chlorine disinfectant solution preparation.
- Take care to allow the disinfectant to remain wet on the surface for the required contact time (e.g., 10 minutes), and then rinse the area with clean water to remove the disinfectant residue (if required).
- Typically, chlorine-based disinfectants at 500-5000ppm free chlorine (1:100 or 1:10 dilution of 5% chlorine-bleach; depending on the size of the spill) are adequate for disinfecting spills (however, do not use chlorine-based disinfectants on urine spills). See Appendix E – Chlorine disinfectant solution preparation.
- Immediately send all reusable supplies and equipment (e.g., cleaning cloths, mops) for reprocessing (i.e., cleaning and disinfection) after the spill is cleaned up.
4.6 Specialized patient areas
Specialized patient areas include those wards or units that provide service to:
- High-dependency patients, (e.g., ICUs).
- Immunosuppressed patients (e.g., bone marrow transplant, chemotherapy).
- Patients undergoing invasive procedures (e.g., operating theater rooms).
- Patients who are regularly exposed to blood or body fluids (e.g., labor and delivery ward, burn units).
Roles and responsibilities
This vulnerable population is more prone to infection and the probability of contamination is high, making these areas higher risk than general patient areas.
Unless otherwise indicated, environmental surfaces and floors in the following sections require cleaning and disinfection with a facility-approved disinfectant for all cleaning procedures described.
4.6.1 Operating rooms
Operating rooms are highly specialized areas with a mechanically controlled atmosphere where surgical procedures are performed. These require environmental cleaning at three distinct intervals throughout the day:
- Before the first procedure.
- Between procedures.
- After the last procedure (i.e., terminal cleaning).
Responsible staff
Because operating rooms are highly specialized areas, the surgery department clinical staff usually manages environmental cleaning. Operating room nurses and their assistants sometimes perform cleaning duties along with, or sometimes instead of, general cleaning staff.
Critical and semi-critical equipment in the operating rooms require specialized reprocessing procedures and are never the responsibility of environmental cleaning staff. The processes described below pertain only to the cleaning and disinfection of environmental surfaces and the surfaces of noncritical equipment.
Where multiple staff are involved, clearly defined and delineated cleaning responsibilities must be in place for cleaning of all environmental surfaces and noncritical patient care equipment (stationary and portable). The use of checklists and SOPs is highly recommended.
Table 13. Recommended Frequency and Process for Operating Rooms
| Frequency | Process |
|---|---|
| Before the first procedure | Carefully inspect records and assess the operating space to ensure that the terminal clean was completed the previous evening.
Wipe all horizontal surfaces in the room (e.g., furniture, surgical lights, operating bed, stationary equipment) with a disinfectant to remove any dust accumulated overnight.
If there was no written confirmation or terminal cleaning on the previous day, do a full terminal clean (see Terminal Clean on this table). Thoroughly clean and disinfect portable patient-care equipment that is not stored within the operating room, such as suction regulators, anesthesia trolley, compressed gas tanks, x-ray machines, and lead gowns, before introduction into the operating room. |
| Before and after each procedure | Remove all used linen and surgical drapes, waste (including used suction canisters, ¾ filled sharps containers), and kick buckets, for reprocessing or disposal.
Clean and disinfect:
|
| After the final procedure (i.e., terminal clean) | Clean and disinfect:
Thoroughly clean and disinfect portable patient-care equipment that is not stored within the operating room before removal from the operating room. Examples include:
|
| Scheduled basis (e.g., weekly, monthly) | At the same time as daily terminal cleaning, clean and disinfect:
|
Environmental cleaning supplies and equipment for the operating room (OR)
Have dedicated supplies and equipment for the OR (e.g., mops, buckets).
Use fresh mops/floor cloths and mopping solutions for every cleaning session, including between procedures.
Use fresh cleaning cloths for every cleaning session, regularly replacing them during cleaning and never double-dipping them into cleaning and disinfectant solutions.
4.6.2 Medication preparation areas
Departments or areas where medication is prepared (e.g., pharmacy or in clinical areas) often service vulnerable patients in high-risk and critical care areas, in addition to other patient populations.
Responsible staff
The staff who work in the medication preparation area might be responsible for cleaning and disinfecting it, instead of the environmental cleaning staff.
Develop detailed SOPs and checklists for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Table 14. Recommended Frequency and Process for Medication Preparation Areas
| Frequency | Process |
|---|---|
| Before and after every use | Countertops and portable carts used to prepare or transport medications |
| At least once every 24 hours | All high-touch surfaces (e.g., light switches, countertops, handwashing sinks, cupboard doors) and floors |
| Scheduled basis (e.g., weekly, monthly) | Low-touch surfaces, such as the tops of shelves, walls, vents |
4.6.3 Sterile service departments (SSD)
Departments or areas where semi-critical and critical equipment is sterilized and stored (i.e., sterile services) often service vulnerable patients in high-risk and critical care areas, in addition to other patient populations.
Responsible staff
Staff who work in the SSD might be responsible for cleaning and disinfecting it instead of environmental cleaning staff. Alternatively, it is possible to train and assign a dedicated cleaning staff member to this area.
Develop detailed SOPs and checklists for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Table 15. Recommended Frequency and Process for Sterile Service Departments (SSD)
| Frequency | Process |
|---|---|
| Before and after every use | Utility sinks used for washing medical devices (e.g., endoscopes) |
| At least twice daily | All high-touch surfaces (e.g., countertops, surfaces of washing equipment, handwashing sinks) and floors |
| Scheduled (e.g., weekly, monthly) | Low-touch surfaces, such as the tops of shelves, walls, vents |
Additional best practices for sterile service departments (SSD)
SSDs have two distinct areas, the soiled area (also called dirty area or decontamination area) and the clean area.
- Start daily environmental cleaning with the clean area and finish with the dirty area.
- Provide separate environmental cleaning supplies and equipment, including PPE for cleaning staff (e.g., reusable rubber gloves, gowns), to prevent cross-contamination between these areas.
- If resources permit, assign separate cleaning staff/teams to each area. If not, clean at different times of the day depending on the workflow.
Find further guidance on environmental cleaning in SSDs here: Decontamination and Reprocessing of Medical Devices for Health-care Facilities.
4.6.4 Intensive care units
Intensive care units (ICUs) are high-risk areas due to the severity of disease and vulnerability of the patients to develop infections.
Frequency and process is the same for adult, pediatric, and neonatal units, but there are specific considerations for neonatal areas. See Process / Additional guidance in Table 16 below.
Table 16. Recommended Frequency and Process for Intensive Care Units
| Frequency | Process / Additional guidance |
|---|---|
| Twice daily and as needed | Clean and disinfect high-touch surfaces
Clean floors with neutral detergent and water If a neonatal incubator is occupied, clean and disinfect only the outside; only clean (neutral detergent) on inside Ensure that cleaning schedules details responsible staff (e.g., nursing or cleaning staff) for environmental cleaning of surfaces of noncritical patient care equipment Last clean of the day: also clean low-touch surfaces; see 4.2.4 Scheduled cleaning |
| Scheduled basis (e.g., weekly) and when visibly soiled | Scheduled basis (e.g., weekly) and when visibly soiled
Change filters in incubators according to manufacturer’s instructions, when wet or if neonate was on contact precautions (during terminal clean) |
| After patient transfer or discharge (i.e., terminal cleaning) | See 4.2.3 Terminal or discharge cleaning of inpatient wards
Pay special attention to terminal cleaning of incubators Pay special attention to ensure reprocessing of noncritical patient care equipment |
Environmental cleaning supplies and equipment for the ICU
Provide dedicated supplies and equipment for the ICU (e.g., mops, buckets) that are not used anywhere else.
Use fresh mops/floor cloths and mopping solutions for every cleaning session.
Use fresh cleaning cloths for surfaces for every cleaning session (at least two per day), regularly replacing them during cleaning and never double-dipping into cleaning and disinfectant solutions.
4.6.5 Emergency departments
Emergency departments are moderate to high-risk areas because of the wide variability in the condition of patients and admissions, which can:
- Increase the probability of contamination of the environment from infectious agents or blood and body fluids.
- Make them more susceptible to infection (e.g., trauma patients).
Responsible staff
Because emergency departments are specialized and high-throughput areas, clinical staff (e.g., nurses) might play an active role in performing environmental cleaning, particularly in examination and procedural areas.
Develop detailed SOPs, including checklists for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Table 17. Recommended Frequency and Process for Emergency Departments
| Area | Frequency | Process |
|---|---|---|
| Waiting / Admission | At least once daily (e.g., per 24-hour period) | High-touch and low-touch surfaces and floors |
| Consultation / Examination (low acuity) | After each event/case and at least twice daily, and as needed | High-touch surfaces
End of the day: entire floor and low-touch surfaces |
| Procedural (trauma, critical care) |
Before and after (i.e., between*) each procedure
*If there is prolonged time between procedures or local conditions that create risk for dust generation/dispersal, re-wipe surfaces with disinfectant solution immediately before the subsequent procedure. |
High-touch surfaces, procedure table and floor, inside the patient zone |
| Procedural (trauma, critical care) | End of the day (terminal clean) |
All surfaces and the entire floor
Handwashing sinks (thoroughly clean (scrub) and disinfect) Sluice areas/sinks or scrub areas |
| All | Scheduled basis (e.g., weekly, monthly) and when visibly soiled | See 4.2.4 Scheduled cleaning |
4.6.6 Labor and delivery wards
Labor and delivery wards are routinely contaminated and patients are vulnerable to infection.
Responsible staff
Because labor and delivery wards are often high-throughput areas, clinical staff (e.g., nurses) might play an active role in performing environmental cleaning, particularly between procedures.
Develop detailed SOPs, including checklists, for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Table 18. Recommended Frequency and Process for Labor and Delivery Wards
| Frequency | Process |
|---|---|
| Before and after (i.e., between) every procedure and at least daily |
Remove soiled linens and waste containers for disposal/reprocessing; see Appendix D – Linen and laundry management
Clean and disinfect:
|
| After the last delivery (terminal clean) |
As above
Clean and disinfect other high-touch surfaces (e.g., light switches, door handles) outside of the patient zone Clean (scrub) and disinfect handwashing sinks Clean and disinfect entire floor (move patient bed and other portable equipment) |
| Scheduled basis (e.g., weekly, monthly) | See 4.2.4 Scheduled cleaning |
4.6.7 Other specialized areas
The areas in this section are higher risk because of:
- High probability of contamination.
- High patient vulnerability to infection.
Responsible staff
Nursing and cleaning staff might be responsible for cleaning certain areas/items in these areas, so there must be clearly defined cleaning responsibilities for all surfaces and equipment (stationary and portable).
Develop detailed SOPs, including checklists, for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Cleaning for specialized areas
- Hemodialysis units
- Hemodialysis units include the dialysis stations (chair or bed, table and dialysis machine) for dialysis treatment.
- Hemodialysis units include the dialysis stations (chair or bed, table and dialysis machine) for dialysis treatment.
- Burn units
- Burn units house patients with significant burn wounds.
- Burn units house patients with significant burn wounds.
- Special isolation units
- Special isolation units house highly immunocompromised patients with specific conditions where white blood cells are depleted (e.g., bone marrow transplant, leukemia).
- Special isolation units house highly immunocompromised patients with specific conditions where white blood cells are depleted (e.g., bone marrow transplant, leukemia).
- Pediatric wards
- Pediatric wards (excludes pediatric intensive care units).
- Pediatric wards (excludes pediatric intensive care units).
- General procedure rooms
- General procedure rooms (e.g., radiology, endoscopy).
- General procedure rooms (e.g., radiology, endoscopy).
- Areas with airborne precautions
- Areas with contact and droplet precautions
Table 19. Recommended Frequency and Process for Hemodialysis Units
| Frequency | Process |
|---|---|
| Before and after (i.e., between) every patient |
Remove disposable patient care items/waste and reprocess reusable noncritical patient care equipment; see Table 26. Recommended Selection and Care of Noncritical Patient Care Equipment
Clean and disinfect:
|
| After the last patient (terminal clean) | As above
|
| Scheduled basis (e.g., weekly, monthly) | Low-touch surfaces; see 4.2.4 Scheduled cleaning |
Table 20. Recommended Frequency and Process for Burn Units
| Frequency | Process |
|---|---|
| Before and after (i.e., between) every procedure and twice daily and as needed |
Remove soiled linens and waste containers for disposal/reprocessing; see Appendix D – Linen and laundry management
Clean and disinfect:
Last clean of the day: clean and disinfect entire floor and low-touch surfaces |
| Scheduled basis | See 4.2.4 Scheduled cleaning |
Table 21. Recommended Frequency and Process for Special Isolation Units
| Frequency | Process |
|---|---|
| Daily, before cleaning any other patient care area (i.e., first cleaning session of the day) | Clean and disinfect:
Clean floors with neutral detergent and water |
| Scheduled basis (e.g., weekly, monthly) | Low-touch surfaces; see 4.2.4 Scheduled cleaning |
| Terminal cleaning | See 4.2.3 Terminal or discharge cleaning of inpatient wards |
Table 22. Recommended Frequency and Process for Pediatric Wards
| Area | Frequency | Process |
|---|---|---|
| Pediatric outpatient wards (waiting/ admission area) | At least daily and as needed (e.g., visibly soiled, blood/body fluid spills) | Clean and disinfect:
|
| Pediatric outpatient wards (consultation/examination area) | After each event/case and at least twice per day and as needed | Clean and disinfect:
|
| Pediatric outpatient wards (minor operative/ procedure rooms) | Before and after (i.e., between) every procedure | Clean and disinfect:
|
| Pediatric inpatient wards | Same as adult inpatient wards | Same as adult inpatient wards; see |
| All pediatric wards | Scheduled basis | See 4.2.4 Scheduled cleaning |
| All pediatric wards | After each use and at least daily | Clean and disinfect:
|
Table 23. Recommended Frequency and Process for General Procedure Rooms
| Frequency | Process |
|---|---|
| Before and after (i.e., between) every patient |
Remove disposable equipment and reprocess reusable noncritical patient care equipment; see Table 26. Recommended Selection and Care of Noncritical Patient Care Equipment.
Clean and disinfect:
|
| After the last patient (terminal clean) |
As above
Clean and disinfect:
|
| Scheduled basis (e.g., weekly, monthly) | See 4.2.4 Scheduled cleaning |
4.6.8 Transmission-based precaution/isolation wards
Isolation or cohorted areas with suspected or confirmed cases of infections requiring transmission-based precautions are considered high-risk areas, particularly for:
- Environmentally hardy pathogens (e.g., resistant to disinfectants).
- Multidrug-resistant pathogens that are highly transmissible and/or are associated with high morbidity and mortality.
The three types of transmission-based precautions are:
- Airborne
- Contact
- Droplet
Transmission-specific PPE is required for all cleaning sessions in areas under transmission-based precautions, according to facility policy or Table 5 in 3.4 Cleaning Supplies and Equipment.
PPE should always be put on and removed following the indications posted/recommended by IPC.
A full list of pathogens/infections requiring these precautions are included in CDC's Guideline for Isolation Precautions.
These are the best practices for environmental cleaning in transmission-based precaution areas:
- Clean these areas after non-isolation areas.
- Change environmental cleaning supplies and equipment, including PPE, directly after cleaning these areas.
- If resources permit, dedicate supplies and equipment for these areas
- If resources permit, dedicate supplies and equipment for these areas
- Post the type of precaution and required procedures, including required PPE, on visible signage outside the isolation area, ensuring that these indications are understood by cleaning staff.
- Do not bring cleaning carts into the area—keep them at the door and only bring the equipment and supplies needed for the cleaning process.
Table 24. Recommended Frequency and Process for Airborne Precautions
| Frequency | Process |
|---|---|
| At least once daily (e.g., per 24-hour period) |
See 4.2.2 Routine cleaning of inpatient wards (only cleaning required)
Unit manager or shift leader should coordinate schedule Take care to keep the door closed during the cleaning process (ventilation requirement) |
| After patient transfer or discharge (terminal clean) | See 4.2.3 Terminal or discharge cleaning of inpatient wards
Unit manager or shift leader should coordinate schedule Take care to keep the door closed during the cleaning process (ventilation requirement) |
Table 25. Recommended Frequency and Process for Contact and Droplet Precautions
| Frequency | Process |
|---|---|
| At least twice daily and as needed |
High-touch surfaces and floors
Any surface (e.g., walls) that is visibly soiled with blood or body fluids See Cleaning for C. difficile (spore forming) Last clean of the day: clean and disinfect low-touch surfaces |
| After patient transfer or discharge (terminal clean) | See 4.2.3 Terminal or discharge cleaning of inpatient wards.
|
Cleaning for C. difficile (spore-forming)
Two-step process required:
- Rigorous mechanical cleaning process (e.g., using friction).
- Disinfectant with sporicidal properties, for example:
- Sodium hypochlorite solution (e.g., 1,000ppm or 5,000ppm). See Appendix E – Chlorine disinfectant solution preparation.
- Enhanced hydrogen peroxide at 4.5%.
- Sodium hypochlorite solution (e.g., 1,000ppm or 5,000ppm). See Appendix E – Chlorine disinfectant solution preparation.
Cleaning for carbapenem-resistant Enterobacterales, Acinetobacter baumannii and Pseudomonas aeruginosa (CRE-CRAB-CRPsA)
These organisms belong to a group of carbapenem-resistant, gram-negative bacteria of national and international concern because of their implication as an emerging cause of severe healthcare-associated infections. In 2017, the World Health Organization published the first global guidelines for the prevention and control of CRE-CRAB-CRPsA in healthcare facilities, which include environmental cleaning and disinfection as a key recommendation.
This implementation guide discusses the key elements of environmental cleaning needed for prevention and control of these organisms: WHO 2019: Implementation manual to prevent and control the spread of carbapenem-resistant organisms at the national and health care facility level [PDF – 98 pages].
Highly infectious pathogens of epidemic potential, such as those that cause viral hemorrhagic fevers (e.g., Ebola)
There might be specific cleaning procedures for isolation areas of highly infectious pathogens. Standalone training programs and strict adherence to required PPE is essential for conducting effective environmental cleaning in these situations.
Find more information on developing context-specific protocols:
4.7 Noncritical patient care equipment
Portable or stationary noncritical patient care equipment incudes IV poles, commode chairs, blood pressure cuffs, and stethoscopes. These high-touch items are:
- Used by healthcare workers to touch patients (i.e., stethoscopes).
- Frequently touched by healthcare workers and patients (i.e., IV poles).
- Often shared between patients.
Critical and semi-critical equipment
Responsible staff
The responsibility for cleaning noncritical patient care equipment might be divided between cleaning and clinical staff, so it is best practice to clearly define and delineate cleaning responsibilities for all equipment (stationary and portable).
Develop a cleaning chart or schedule outlining the method, frequency, and staff responsible for cleaning every piece of equipment in patient care areas and take care to ensure that both cleaning and clinical staff (e.g., nursing) are informed of these procedures so that items are not missed.
These are the best practices for selection and care of noncritical patient care equipment:
- Clean all equipment using the methods and products available at the facility.
- All equipment should include detailed written instructions for cleaning and disinfection from the manufacturer, including pictorial instructions if disassembly is required.
- Train the staff responsible for cleaning equipment on procedures before the equipment is placed into use.
- In patient care areas, do not purchase, install, or use equipment that cannot be cleaned and disinfected, unless they can be fitted with plastic (or other material) coverings.
- If plastic coverings are protecting difficult-to-clean equipment, clean these items with the same frequency, inspect coverings for damage on a regular basis, and repair or replace them as needed.
Table 26. Recommended Selection and Care of Noncritical Patient Care Equipment
| Type of Equipment | Frequency | Method | Additional Guidance |
|---|---|---|---|
| Shared (e.g., general inpatient wards) | Before and after each use | Clean and disinfect | Select a compatible disinfectant; see 4.7.1 Material compatibility considerations
Clean and disinfect heavily soiled items (e.g., bedpans) outside of the patient care area in dedicated 4.7.2 Sluice rooms Disinfect bedpans with a washer-disinfector or boiling water instead of a chemical disinfection process. |
| Dedicated (e.g., transmission-based precautions, isolation wards) | According to frequency of patient care area (at the same time as routine cleaning) | Method based on the risk level of the patient care area | Select a compatible disinfectant; ee 4.7.1 Material compatibility considerations
Clean and disinfect heavily soiled items (e.g., bedpans) outside of the patient care area in dedicated 4.7.2 Sluice rooms Disinfect bedpans with a washer-disinfector or boiling water instead of a chemical disinfection process |
| All | After patient transfer or discharge (i.e., terminal cleaning) | Clean and disinfect | Conduct terminal cleaning of all noncritical patient care equipment in 4.7.2 Sluice rooms |
4.7.1 Material compatibility considerations
A list of compatible cleaning and disinfectant products should be included in manufacturer's instructions or provided by the manufacturer upon request.
If manufacturer instructions are not available, here are the applicable material compatibility considerations and best practices for use of common healthcare disinfectants:
Table 27. Recommended Material Cleaning and Disinfectant Compatibility Considerations
| Disinfectant | Material compatibility considerations | Best practices for use on noncritical patient care equipment |
|---|---|---|
| Chlorine/ hypochlorite-based | Corrosive to metals |
|
| Alcohols (60-80%) | Could deteriorate glues and cause damage to plastic tubing, silicone, and rubber |
|
4.7.2 Sluice rooms
Each major patient care area should be equipped with a designated sluice room to reprocess soiled noncritical patient care equipment (e.g., commode chairs, bedpans). Alternatively, there may be central depots where these procedures are performed.
Sluice rooms should be as close as possible to the patient care areas that they serve and should have an organized workflow from soiled (dirty) to clean.
The soiled area (used for reprocessing equipment) should be adequately sized and have:
- A door that is kept closed at all times and ideally has hands-free operation.
- A work counter and sluice/utility sink with a hot and cold faucet.
- A dedicated handwashing sink.
- Space for washers/disinfectors (if resources allow).
- PPE available to protect staff during cleaning and disinfecting procedures.
The clean area (used for storing reprocessed equipment) should:
- Be distinctly separate from (by workflow) soiled areas to prevent confusion regarding reprocessing status.
- Have shelves that are smooth, non-porous, and easy to clean.
- Be protected from water and soil, dirt, and dust.
- Be as close as possible to patient areas and easily available to staff.
Table 28. Recommended Frequency, Method and Process of Sluice Rooms
| Type of Equipment | Frequency | Method | Additional Guidance |
|---|---|---|---|
| Soiled areas | At least once daily (e.g., per 24-hours period) | Clean and disinfect | High-touch and frequently contaminated surfaces, including work counters and sinks, and floors (floors only require cleaning) |
| Clean area | At least once daily (e.g., per 24-hours period) | Clean | Horizontal surfaces and floors
Clean equipment should be covered or removed during cleaning process |
| Both | Scheduled basis (e.g., weekly) and when visibly soiled | Clean | Low-touch surfaces (e.g., vents, tops of cupboards) |
4.8 Methods for assessment of cleaning and cleanliness
It is best practice to perform routine, standardized assessments of environmental cleaning (i.e., practices, level of cleanliness) in order to:
- Ensure that environmental cleaning procedures are being performed according to best practices and facility policy.
- Use results to inform program improvement (e.g., training, resource allocation).
This section includes an overview of the available methods, as well as their advantages and disadvantages. The best practices for developing a system of routine monitoring, audit, and feedback within environmental cleaning program implementation are covered in 2.5 Monitoring, feedback, and audit elements.
Methods for assessing cleaning practice include (Table 29 below)
- Direct performance observations.
- Visual assessment.
- Fluorescent markers.
Methods for assessing the level of cleanliness include (Table 30 below)
- Measuring the residual bioburden (i.e., ATP).
- Taking a bacteriological culture of the surface itself using a swab or contact agar plate method.
Table 29. Advantages and Disadvantages of Monitoring Methods for Assessing Cleaning Practice: Adherence to Cleaning Procedures
| Method | Advantages | Disadvantages |
|---|---|---|
| Performance observations: observers (e.g., cleaning supervisors) use standardized perform structured observations using checklists that are specific to individual patient care areas. The goal is to rate the effectiveness of cleaning staff and adherence to the SOP (such as identifying the number of steps performed correctly). | Can be used for large areas (units, wards)
Easy to implement Benchmarking is possible Simple and inexpensive Allows immediate and direct feedback to individual staff Encourages cleaning staff engagement and input Identifies gaps for staff training/job aid improvements |
Subjective—difficulty in standardizing methodology and assessment across observers
Labor-intensive Results affected by Hawthorne bias (i.e., more of an assessment of knowledge than actual practice) Does not assess or correlate to bioburden |
| Visual assessment of cleanliness: after an area has been cleaned, observers check the cleanliness of items. For example, using a gloved hand, wipe surfaces to inspect for dust. | Can be applied to entire facility or specific units/wards
Easy to implement Benchmarking is possible Inexpensive Allows immediate and direct feedback to individual staff |
Could be delay in feedback dependent on method used to compile results
Subjective—based on individual determinations of dust/debris levels Does not assess or correlate to bioburden |
| Fluorescent markers (e.g., UV visible): a tracing agent (e.g., fluorescent material, chemical tracer) marks predetermined items and surfaces before cleaning. After cleaning, a trained observer uses a detecting agent (e.g., ultraviolet light, enzymatic detector) to determine if any tracing agent is left. The observer counts the items that still show tracing agent and gives a score based on how many were cleaned completely, partially, or not at all. |
Quick
Provides immediate feedback on performance Minimal training required to perform Objective Benchmarking is possible Relatively inexpensive |
Does not assess or correlate to bioburden
Labor-intensive as surfaces should be marked before cleaning and checked after cleaning has been completed Some difficulties documented in terms of removal of markers from porous or rough surfaces (e.g., canvas straps) Time-intensive Need to vary frequency and objects to prevent monitoring system from becoming known |
Table 30. Advantages and Disadvantages of Monitoring Methods for Assessing Cleanliness: Effectiveness of Cleaning Procedures
| Method | Advantages | Disadvantages |
|---|---|---|
| ATP bioluminescence: detection of ATP indicates that organic material (microbial or biologic) is present on an object or surface. Objects are tested before and after cleaning to determine the effectiveness of a cleaning procedure. A numeric score can be generated based on the proportion of marked surfaces/objects that were under the pre-determined threshold. |
Quick
Provides immediate feedback Minimal training required to perform Objective |
Expensive
Low sensitivity and specificity Lacks a standardized threshold or benchmark for determining the level or status of cleanliness (i.e., “safe” post-cleaning ATL levels) for specific surfaces or patient care areas Variable benchmarks Technology constantly changing Interference of cleaning products, supplies and in some cases surfaces, which can both reduce or enhanced ATP levels (e.g., bleach, microfiber, stainless steel) |
| Environmental cultures: the only direct measurement of levels of microbial contamination after cleaning. In this process, cultures are taken (by swabbing or use of RODAC or contact agar plates) after an item is cleaned. Swabbing can indicate the presence of a specific bacteria on a surface. Contact agar plates can show the level of bacterial contamination on an area of a large, flat surface. |
High sensitivity and specificity
Provides direct indication of presence of specific pathogens (direct swab cultures) May be useful for identifying source of outbreaks and/or environmental reservoirs Objective |
Not recommended for routine use
Expensive Prolonged time for results (>48hrs) Requires access to laboratory resources and trained personnel for interpreting results Lack of defined threshold or benchmark for determining the level or status of cleanliness (e.g., colony-forming units per surface area) |
- If there is prolonged time between procedures or local conditions that create risk for dust generation/dispersal, re-wipe surfaces with disinfectant solution immediately before the subsequent procedure.
