REACH

Every person deserves the chance to be healthy, but some chronic diseases and their risk factors are more common or severe for certain racial and ethnic minority groups in the United States. Many complex factors influence health disparities. Often called social determinants of health, these factors may include economic stability, education access and quality, social and community context, health care access and quality, food and nutrition security, neighborhoods and the built environment.
The Racial and Ethnic Approaches to Community Health (REACH) program is at the forefront of CDC’s efforts to reduce health disparities and achieve health equity. Since 1999, REACH has worked to reduce health disparities among specific racial and ethnic groups in communities with the highest risk or rates of chronic disease.
REACH strives to promote healthy behaviors and reduce chronic disease risk factors among people who are Black or African American, Hispanic or Latino, Asian or Asian American, American Indian or Alaska Native, and Natives of Hawaii or other Pacific Islands.
In rural, urban, and tribal communities across the United States, REACH recipients use the following strategies as part of culturally tailored interventions designed to improve social and environmental conditions:
- Increase options for good nutrition across the lifespan.
- Promote community planning and transportation plans that create places for safe and accessible physical activity.
- Prevent and reduce commercial* tobacco use.
- Connect clinical services to community programs that help people prevent and manage chronic diseases such as heart disease and diabetes.
* When CDC references tobacco on this web page, we are referring to the use of commercial tobacco and not the sacred and traditional use of tobacco by some American Indian communities.
Fast Stats
Because of REACH program activities during 2014-2018:
Over 2.9 million people
have better access to healthy foods and drinks.
Over 322,000 people
have benefited from
smoke-free and
tobacco-free
interventions.
About 1.4 million people
have more opportunities
to be physically active.
About 830,000 people
have access to local chronic disease programs that are linked to health care systems.
CDC’s Approach
Reaching the Racial and Ethnic Groups Most Affected by Chronic Diseases

Heart disease, cancer, diabetes, and stroke are among the most common causes of illness, disability, and death in the United States. These chronic conditions—and the factors that lead to them—are more common or severe for some racial and ethnic groups. For example:
- From 2017 to 2020, the percentage of people with diabetes (diagnosed and undiagnosed) was higher among Hispanic (15.5%) and non-Hispanic Black (17.4%) adults compared to non-Hispanic White (13.6%) adults, after accounting for age differences in the populations.
- From 2018 to 2019, the percentage of American Indian and Alaska Native adults with diagnosed diabetes for both men (14.4%) and women (14.7%) was higher than for people of other race/ethnicities, after accounting for age differences in the populations.
Using Locally Based and Culturally Tailored Solutions That Work

A cornerstone of the REACH program is making sure that community members are involved in shaping the strategies that will be used in their communities. Recipients often hire or partner with people who represent the needs of the community and work with them to adapt programs that reflect local cultural norms, language, and practices.
REACH recipients also form coalitions to promote health. Partners include groups that represent the focus populations, state and local health agencies, universities, community organizations, housing and transportation authorities, health care organizations, employers, and faith-based organizations.
Local evaluations show that REACH recipients have changed local environments to support healthier behaviors among racial and ethnic minority populations. From 2014 to 2018, REACH communities reported the following successes:
- Working with rural communities in the Navajo Nation, an organization called Partners in Health helped increase access to healthier foods in small stores and at community venues for about 18,500 residents. It also trained community health workers to help increase access to health services for about 90,000 community members.
- In DeKalb County, Georgia, farmers’ markets participating in a REACH program helped increase access to healthy food for about 242,000 African American residents. As a result, county officials reported a 34% increase in fruit and vegetable consumption among customers.
- In Omaha, Nebraska, the REACH program at Creighton University partnered with the Omaha Housing Authority to create safer places for physical activity for more than 330 African American residents of three low-income housing towers.
- In Orange County, California, a REACH program improved access to smokefree environments for an estimated 100,000 Asian or Asian American residents by increasing the number of commercial shopping plazas with voluntary smokefree policies.
- In Cuyahoga County, Ohio, the Produce Prescription Program for Hypertension helped connect about 600 Asian or Asian American and Pacific Islander people with low income and high blood pressure to information about healthy eating and affordable produce.
- The Toiyabe Indian Health Project increased the availability of healthy foods for an estimated 3,000 American Indian people in seven tribes and two tribal communities along the eastern Sierra Nevadas by increasing healthy food production in community gardens.
Expanding the Legacy of REACH
Since 1999, REACH has evolved from focusing on specific diseases—like heart disease and vaccine-preventable diseases—to supporting broader environmental improvements designed to reduce chronic disease risk factors.
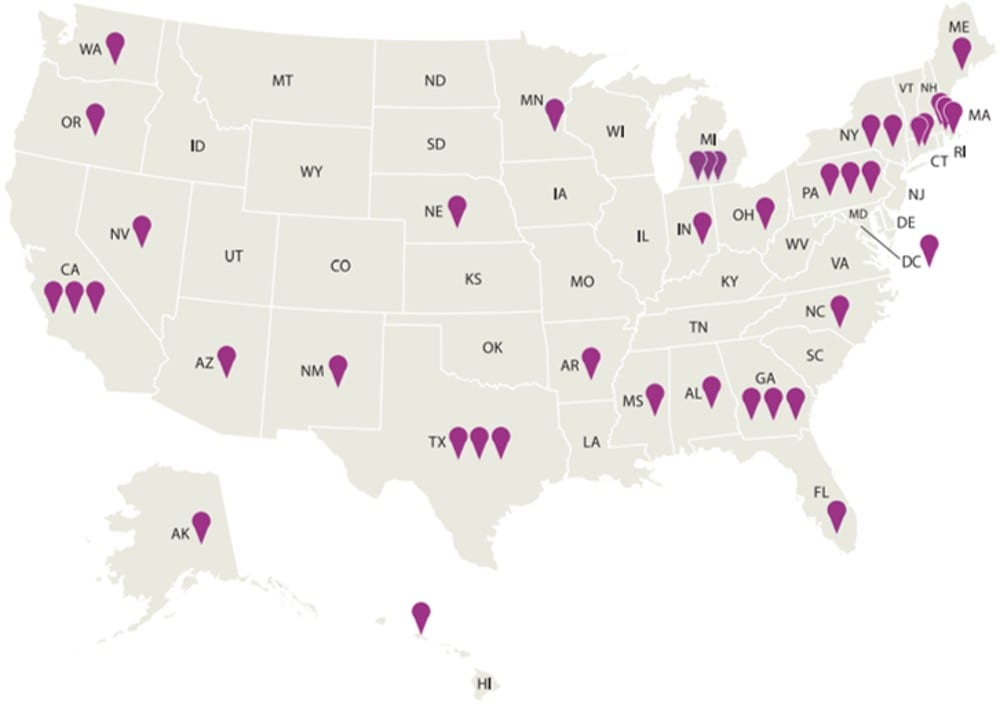
The REACH program currently funds 40 recipients, including community organizations, universities, local health departments, tribal organizations, and states. Each recipient uses at least three of the following strategies:

Increase Options for Good Nutrition Across the Lifespan
- Work with food vendors, distributors, and producers to increase the number of healthy foods they buy and sell.
- Help hospitals, early care and education centers, and worksites use nutrition standards that increase the availability of healthy foods.
- Improve local nutrition programs and food systems. Examples include using voucher incentive programs, accepting electronic benefit transfer cards where food is purchased, improving public transportation routes to food stores, and improving access to healthy foods at community venues.
- Support breastfeeding by making it easier to breastfeed in more places and by training health workers to give mothers the help and support they need to breastfeed.
Promote Community and Transportation Planning to Increase Physical Activity
- Work with partners to connect activity-friendly routes to everyday destinations by using land use and environmental design interventions.
Support Tobacco-Free Living
- Implement tobacco-free policies in workplaces and multi-unit housing.
- Work with health care providers to ensure that patients are screened for tobacco use, advised to quit, and given resources.
- Communicate culturally tailored messages on the effects of tobacco and secondhand smoke exposure. Encourage quitting and calling tobacco quitlines.
Connect Clinics to Community Programs for Chronic Disease Management
- Increase referrals and access to community health programs—for example, by expanding the use of community health workers, patient navigators, and pharmacists.
As REACH continues to strengthen efforts to prevent disease and reduce racial and ethnic health disparities, REACH communities will create sustainable solutions that break down barriers to health.
The REACH budget line provides (1) core REACH program funding to 40 urban, rural, and tribal areas to address health disparities in chronic diseases and related risk factors among five racial and ethnic minority groups and (2) direct funding to tribes, Alaska Native villages, tribal organizations, Tribal Epidemiology Centers, and Urban Indian Organizations to improve the health of American Indians and Alaska Natives as part of CDC’s Healthy Tribes program.