Diagnosis and Treatment
Early diagnosis and treatment are very important for serious pneumococcal infections. Antibiotics can help treat severe illnesses caused by pneumococcal bacteria.
Diagnosis
If doctors suspect serious pneumococcal disease, like meningitis or bloodstream infections, they will collect samples of cerebrospinal fluid or blood. Cerebrospinal fluid is the fluid that surrounds the brain and spinal cord. View the lumbar puncture illustration to see how a doctor collects this fluid. Doctors then send the samples to a laboratory for testing.
Growing the bacteria in a laboratory helps identify the specific type of bacteria causing the infection. Knowing the cause helps doctors choose the right treatment, including which antibiotic will work best.
Doctors can use a urine test to help make a diagnosis of pneumococcal pneumonia in adults. Doctors usually diagnose ear and sinus infections based on a history and physical exam findings that support pneumococcal infection.
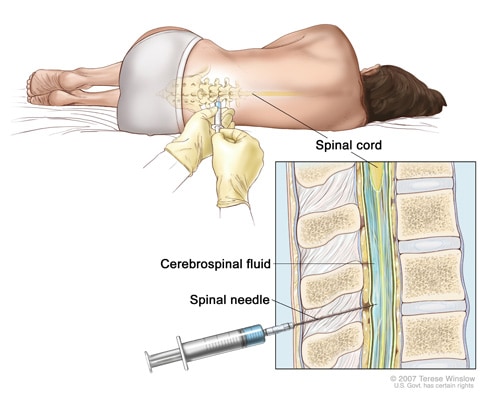
Doctors use a lumbar puncture to collect a sample of cerebrospinal fluid.
Treatment
Doctors use antibiotics to treat pneumococcal disease. However, some pneumococcal bacteria have become resistant to certain antibiotics used to treat these infections. Available data show that pneumococcal bacteria are resistant to one or more antibiotics in 3 out of every 10 cases.
Antibiotic treatment for serious pneumococcal infections typically includes ‘broad-spectrum’ antibiotics until results of antibiotic sensitivity testing are available. Antibiotic sensitivity testing shows which antibiotics will be most successful at treating a bacterial infection. Broad-spectrum antibiotics work against a wide range of bacteria. Once the sensitivity of the bacteria is known, doctors may choose a more targeted (or ‘narrow-spectrum’) antibiotic.
The number of antibiotic-resistant pneumococcal infections has decreased due to the success of pneumococcal conjugate vaccination. In addition to vaccination, appropriate use of antibiotics may also slow or reverse drug-resistant pneumococcal infections.

Available data show that pneumococcal bacteria are resistant to one or more antibiotics in 3 out of every 10 cases.



