FIGURE 1. Critical actions needed to improve chances of survival of an out-of-hospital cardiac arrest
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Out-of-Hospital Cardiac Arrest Surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010
Corresponding author: Amy L. Valderrama, PhD, National Center for Chronic Disease Prevention and Health Promotion, CDC, 4770 Buford Highway N.E., MS K-47, Atlanta, GA 30341. Telephone: 770-488-8218; Fax: 770-488-8334; E-mail: fgj0@cdc.gov.
Abstract
Problem/Condition: Each year, approximately 300,000 persons in the United States experience an out-of-hospital cardiac arrest (OHCA); approximately 92% of persons who experience an OHCA event die. An OHCA is defined as cessation of cardiac mechanical activity that occurs outside of the hospital setting and is confirmed by the absence of signs of circulation. Whereas an OHCA can occur from noncardiac causes (i.e., trauma, drowning, overdose, asphyxia, electrocution, primary respiratory arrests, and other noncardiac etiologies), the majority (70%--85%) of such events have a cardiac cause.
The majority of persons who experience an OHCA event, irrespective of etiology, do not receive bystander-assisted cardiopulmonary resuscitation (CPR) or other timely interventions that are known to improve the likelihood of survival to hospital discharge (e.g., defibrillation). Because nearly half of cardiac arrest events are witnessed, efforts to increase survival rates should focus on timely and effective delivery of interventions by bystanders and emergency medical services (EMS) personnel. This is the first report to provide summary data from an OHCA surveillance registry in the United States.
Reporting Period: This report summarizes surveillance data collected during October 1, 2005-- December 31, 2010.
Description of the System: In 2004, CDC established the Cardiac Arrest Registry to Enhance Survival (CARES) in collaboration with the Department of Emergency Medicine at the Emory University School of Medicine. This registry evaluates only OHCA events of presumed cardiac etiology that involve persons who received resuscitative efforts, including CPR or defibrillation. Participating sites collect data from three sources that define the continuum of emergency cardiac care: 911 dispatch centers, EMS providers, and receiving hospitals. OHCA is defined in CARES as a cardiac arrest that occurred in the prehospital setting, had a presumed cardiac etiology, and involved a person who received resuscitative efforts, including CPR or defibrillation.
Results: During October 1, 2005--December 31, 2010, a total of 40,274 OHCA records were submitted to the CARES registry. After noncardiac etiology arrests and missing hospital outcomes were excluded from the analysis (n = 8,585), 31,689 OHCA events of presumed cardiac etiology (e.g., myocardial infarction or arrhythmia) that received resuscitation efforts in the prehospital setting were analyzed. The mean age at cardiac arrest was 64.0 years (standard deviation [SD]: 18.2); 61.1% of persons who experienced OHCA were male (n = 19,360). According to local EMS agency protocols, 21.6% of patients were pronounced dead after resuscitation efforts were terminated in the prehospital setting. The survival rate to hospital admission was 26.3%, and the overall survival rate to hospital discharge was 9.6%. Approximately 36.7% of OHCA events were witnessed by a bystander. Only 33.3% of all patients received bystander CPR, and only 3.7% were treated by bystanders with an automated external defibrillator (AED) before the arrival of EMS providers. The group most likely to survive an OHCA are persons who are witnessed to collapse by a bystander and found in a shockable rhythm (e.g., ventricular fibrillation or pulseless ventricular tachycardia). Among this group, survival to discharge was 30.1%.
A subgroup analysis was performed among persons who experienced OHCA events that were not witnessed by EMS personnel to evaluate rates of bystander CPR for these persons. After exclusion of 3,400 OHCA events that occurred after the arrival of EMS providers, bystander CPR information was analyzed for 28,289 events. In this group, whites were significantly more likely to receive CPR than blacks, Hispanics, or members of other racial/ethnic populations (p<0.001). Overall survival to hospital discharge of patients whose events were not witnessed by EMS personnel was 8.5%. Of these, patients who received bystander CPR had a significantly higher rate of overall survival (11.2%) than those who did not (7.0%) (p<0.001).
Interpretation: CARES data have helped identify opportunities for improvement in OHCA care. The registry is being used continually to monitor prehospital performance and selected aspects of hospital care to improve quality of care and increase rates of survival following OHCA. CARES data confirm that patients who receive CPR from bystanders have a greater chance of surviving OHCA than those who do not.
Public Health Actions: Medical directors and public health professionals in participating communities use CARES data to measure and improve the quality of prehospital care for persons experiencing OHCA. Tracking performance longitudinally allows communities to better understand which elements of their care are working well and which elements need improvement. Education of public officials and community members about the importance of increasing rates of bystander CPR and promoting the use of early defibrillation by lay and professional rescuers is critical to increasing survival rates. Reporting at the state and local levels can enable state and local public health and EMS agencies to coordinate their efforts to target improving emergency response for OHCA events, regardless of etiology, which can lead to improvement in OHCA survival rates.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a leading cause of death among adults in the United States. Approximately 300,000 OHCA events occur each year in the United States; approximately 92% of persons who experience an OHCA die (1). An OHCA is defined as cessation of cardiac mechanical activity that is confirmed by the absence of signs of circulation and that occurs outside of a hospital setting (1,2). While an OHCA can occur from multiple causes (i.e., trauma, drowning, overdose, asphyxia, electrocution, primary respiratory arrests and other noncardiac etiologies), the majority (70%--85%) of such events have a cardiac etiology (3--6).
In the first few minutes following OHCA, swift implementation of five critical actions by bystanders or emergency medical services (EMS) providers comprising a framework known as the "chain of survival" (Figure 1) can substantially increase the chances of survival from OHCA. These actions should be undertaken regardless of the cause of the OHCA and include 1) rapid activation of EMS by calling 911, 2) rapid initiation of cardiopulmonary resuscitation (CPR), 3) prompt application and use of an automated external defibrillator (AED), 4) rapid delivery of advanced life support by EMS providers, and 5) early postresuscitative care (7,8). Despite decades of research, median reported rates of survival to hospital discharge are poor (7.9%) and have remained virtually unchanged for 3 decades (9,10). Moreover, survival rates vary widely across the United States. The likelihood of surviving an OHCA caused by ventricular fibrillation varies widely (range: 2%--35%), depending on the location of the OHCA event (11). Without a reliable method to collect data in a uniform fashion, the effectiveness of different EMS systems and interventions cannot be compared. Participation in an OHCA registry enables medical providers and EMS systems to compare patient populations, interventions, and outcomes and identifies opportunities to improve quality of care and ascertain whether resuscitation is provided according to evidence-based guidelines (2).
Since the mid-1990s, the need for widespread, uniform EMS data reporting has been well understood; both the National Highway Traffic Safety Administration (NHTSA) and the Health Resources and Services Administration (HRSA) have highlighted the need for EMS data as a necessary foundation for evaluating the effectiveness of EMS care and called for the adoption of standardized data collection strategies and linking prehospital patient care information with outcomes (12,13). The American Heart Association (AHA) and other international organizations have called for integrated methods of data collection from EMS agencies, hospitals, and communities to improve care and compare performance across systems (7). In 2006, the Institute of Medicine (IOM) noted that the majority of EMS agencies cannot document their impact on the communities they serve and recommended that the EMS community collect, analyze, and use performance improvement data (14). In 2008, AHA renewed its call for widespread data surveillance and for making OHCA a reportable condition (3). Healthy People 2020 (objective no. HDS-18) called for increasing the proportion of OHCA events that receive appropriate bystander and EMS care (15). In 2004, to develop a model national registry that could measure outcomes and progress in the treatment of OHCA, CDC collaborated with the Emory University School of Medicine to establish the Cardiac Arrest Registry to Enhance Survival (CARES), which collects data to improve the quality of care and outcomes of patients who experience an OHCA.
CARES utilizes Utstein-style definitions and reporting templates. The Utstein guidelines were first published in 1991 and later updated in 2004 by the International Liaison Committee on Resuscitation (ILCOR) to provide a uniform reporting template to describe OHCA events (2,16). The Utstein style was adopted by researchers and clinicians as a standard to use for research and registry databases for the purposes of tracking cardiac arrest in both in-hospital and out-of-hospital settings. This template has been used in many published studies of cardiac arrest and has contributed to a greater understanding of resuscitation science and resuscitation guidelines (2). The Utstein template can be used within hospitals, EMS systems, or communities and enables identification of areas that need improvement and comparisons across systems. It consists of 29 core data elements that allow for standardized resuscitation terminology. The Utstein template stratifies arrests by witness status (i.e., unwitnessed, witnessed by a bystander, or witnessed by 911 responders) and then further stratifies arrests by initial cardiac arrest rhythm. Utstein survival refers to survival to hospital discharge of those cardiac patients whose arrest events were witnessed by a bystander and that involved persons who had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia. These patients are the most likely to respond to CPR or defibrillation and are thus more likely to survive an OHCA event.
CARES is a simple but robust registry of cardiac arrest events that allows participating sites to enter OHCA-related data, generate summary reports, and compare local data with similar EMS systems elsewhere. The ultimate goal of CARES is to help local EMS administrators and medical directors identify when and where OHCA events occur, who is affected, which elements of the response system are functioning properly and which are not, and what changes can be made to improve cardiac arrest outcomes (17).
Methods
CARES is funded by CDC through a cooperative agreement with the Association of American Medical Colleges (AAMC), which supports the academic medical community's participation in CDC's efforts to promote the prevention and control of disease, injury, and disability. Since 2004, AAMC has provided funding for the Department of Emergency Medicine at the Emory University School of Medicine to implement CARES. This report, the first to present OHCA surveillance data, summarizes CARES data for October 1, 2005--December 31, 2010 from 46 EMS agencies in 36 communities in 20 states (Table 1; Figure 2).
Recruitment and Selection of 911 Call Centers, EMS Agencies, and Hospitals
CARES was first implemented in October of 2005 in Atlanta, Georgia, a city in Fulton County served by a single advanced life-support EMS, one first-responding fire department, a single 911 computer-aided dispatch center, and 13 hospitals. Approximately 600 cases were entered during an initial 12-month period of pilot testing and refinement before the program was expanded to the rest of Fulton County and the surrounding seven counties in the metropolitan Atlanta area, an area encompassing 2,000 square miles with a population of approximately 3 million persons. This phase helped in understanding how to work in a complicated and multijurisdictional environment.
CARES began expansion to other communities in 2006. Initially, several communities were invited to participate on the basis of their ability or history of collecting data regarding OHCA. After these agencies joined the registry, interest in CARES began to grow. Other medical directors learned about the registry through word-of-mouth at conferences and meetings and contacted program staff to request participation. Currently, CARES has a waiting list of sites interested in participating. At present the program has grown to encompass more than 40 communities in 23 states, representing 73 EMS agencies and more than 340 hospitals. Approximately 22 million persons reside in communities that are participating in CARES.
Participation in CARES is contingent on having complete EMS coverage of a catchment area. In communities for which multiple EMS providers service one catchment area, all providers must participate to ensure capture of all OHCA events within the respective service area. Communities need to establish contacts at their local hospitals to provide emergency room and hospital data. Participating agencies also must ensure through routine audits of paper or electronic records that all of their OHCA events are being reported.
Case Definition
CARES includes data on persons of any age who have an OHCA event and who receive resuscitative efforts (e.g., CPR or defibrillation). Patients with obvious signs of death (e.g. rigor mortis or dependent lividity) or for whom a "do not resuscitate" (DNR) order is respected are not included. The event must have occurred as the result of a presumed cardiac etiology on the basis of the clinical judgment of the care providers. Noncardiac etiologies (e.g., trauma, drowning, overdose, asphyxia, electrocution, primary respiratory arrest, or other noncardiac etiologies) are excluded from analyses.
Case Ascertainment
EMS providers initiate the reporting process. The catchment area of an EMS agency is defined as the regular area of response that is determined locally and might be consistent with a county, township, or municipal border. Regardless of how an EMS agency's area of response is defined geographically, it must allow for capture of all OHCA resuscitation events in its area.
Data Collection
Three sources of data are linked to describe each OHCA adequately: 1) 911 call center data (to provide incident address and dispatch and arrival times), 2) EMS data (to describe initially recorded cardiac rhythm and treatment methods), and 3) hospital data. Hospital data (emergency department and hospital outcome, hypothermia treatment, and neurologic status at discharge) are requested only when the data are not available already in the EMS record. If the resuscitation ends in the emergency department before EMS providers leave the hospital, this is documented in the CARES EMS report, and no additional data are needed from the hospital. This helps to decrease the data-reporting burden required of hospitals and promotes and sustains participation in the program because the majority of patients transported to the hospital die in the emergency department.
If a community uses a unique identifier number, CARES uses that number to link 911 call center, EMS, and hospital datasets to form a complete record for each event. When a unique number does not exist, the files are linked by matching the patient name and age with the event time, date, and location. To preserve patient confidentiality, individual identifiers are stripped from each record after a CARES analyst confirms the completeness and accuracy of each event.
The number of mandatory data elements is limited to the minimum required to characterize an OHCA event and document its outcome. Candidate variables were drawn from three existing datasets that focus on OHCAs rather than in-hospital cardiac arrests: 1) the Utstein template (2); 2) the National EMS Information System (NEMSIS), created by a panel of experts in 2001(18); and 3) the Resuscitation Outcomes Consortium, created by a network of National Institutes of Health--funded research institutions in 2006 (19). Each variable was vetted by CARES staff, with input from an ad hoc panel assembled at the National Association of EMS Physicians Annual Meeting in 2004 (17). Four criteria were used to determine which data elements to include in CARES: 1) whether the variable is necessary to characterize an OHCA event, 2) whether it can be defined clearly, 3) whether it can be measured objectively and reported reliably, and 4) whether it can affect or measure the outcome. For the variable to be included in CARES, all four criteria have to be met. This iterative process produced a core dataset of 31 elements (Figure 3). For consistency, NEMSIS data definitions were used wherever possible. The CARES data dictionary is available at https://mycares.net.
CARES data are compiled by using a Health Insurance Portability and Accountability Act (HIPAA)--compliant, web-based system developed by Sansio, Inc (Duluth, Minnesota) and managed by CARES staff. The web-based system is used for data collection, management, and reporting. Sites can readily access their data and compare it with aggregate output of the entire registry. Access to the site is restricted to authorized users, who are prohibited from viewing data from another agency or hospital.
911 Call Centers
Data elements collected from the 911 call centers include incident location, the time that each 911call was received, the time of dispatch for both first responder and EMS providers, and arrival time at the scene. The data can be entered directly online or uploaded in batched files from a computer-aided dispatch center (CAD). Wide variation in how response time elements are defined in each community prevents aggregation of response time data on a national level. Instead, these data are used routinely for local benchmarking purposes with historic data used for purposes of comparison.
EMS Agencies
Data elements collected from EMS providers include demographic information (i.e., name, age, date of birth, address of event, sex, and race/ethnicity), arrest-specific information (i.e., location of arrest, witnessed versus unwitnessed arrests, and presumed etiology), and resuscitation-specific information (i.e., whether resuscitation was attempted, bystander initiated CPR information, who initiated defibrillation, initial cardiac rhythm, return of spontaneous circulation [ROSC], and prehospital survival status).
The initial cardiac telemetry that is documented can identify a shockable rhythm (one that is responsive to defibrillation, including ventricular fibrillation and pulseless ventricular tachycardia). Such patients are more likely to survive than those patients whose rhythm is not shockable. Because a shockable rhythm can deteriorate over time into a nonshockable rhythm, the time of the initially documented rhythm also can be considered as a surrogate marker for the time from collapse in those patients who are believed to have had a cardiac etiology event, emphasizing the importance of minimizing delay until defibrillation.
The data can be submitted in two ways: 1) online by using a data-entry template on the CARES website, and 2) a daily upload of records from EMS services that use an electronic patient-care record system. Data entry checks have been embedded in the software to help minimize errors and enhance the accuracy of the data collection process. Each EMS agency also has a method to make sure that all of its resuscitation efforts are reported, which involves either an electronic query of its e-PCR or a manual review of its paper charts.
Hospitals
Five data elements are requested from hospitals: 1) emergency department outcomes (i.e., admitted, died, or transferred), 2) hospital outcome (i.e., discharged alive, died, or transferred), 3) patient disposition (i.e., discharged home or transferred to a second hospital, a rehabilitation facility, or a skilled nursing facility), 4) neurologic outcome at discharge (i.e., the Cerebral Performance Categories [CPC] Scale), and 5) whether therapeutic hypothermia treatment was provided.
Neurologic status at discharge is determined by using the CPC Scale (Box). This scale is provided to hospital users who indicate the cerebral performance of the patient as good (CPC 1), moderate (CPC 2), severe (CPC 3), or in a coma or vegetative state (CPC 4). Obtaining neurologic outcome is required to measure the overall clinical outcome of each OHCA patient. Because anoxic brain injury can occur within 4--6 minutes of collapse, communities with more favorable outcomes (CPC 1 or CPC 2) would likely be more effective might their bystander CPR rates and have shorter 911 response times given the time-sensitive nature of this condition.
If EMS providers document ongoing resuscitation in the emergency department, the CARES software automatically sends the respective hospital contact a reminder via e-mail that prompts the contact to log in to the CARES website and provide the needed outcomes to expedite the data-collection process. A hospital contact who logs in to the secure CARES website is able to determine the patient's name, date of birth, and date of admission as entered by the EMS provider. The hospital contact is then able to review a discharge summary or hospital emergency room log and determine quickly the survival status and neurologic outcomes requested.
Often, the primary obstacle to obtaining hospital participation in CARES has been concerns about federal patient privacy laws (14,20). In an effort to alleviate this concern, CARES provides documentation to hospitals about rules related to sharing information for public health purposes (17) and emphasizes the security of the HIPAA-compliant process used to collect and store the data.
Completeness of Case Ascertainment and Data Validation
For agencies that utilize an electronic patient-care record system, an electronic query algorithm is used to identify a cardiac arrest by searching patient records for data fields most likely to identify the event. The software algorithm searches for records in which the provider impression is documented as cardiac arrest or defibrillation, CPR, or intravenous administration of epinephrine (cardiac dosages) on the EMS report to ensure a sensitive method of capturing all CARES events. Records that are identified are matched against the CARES database to ensure that all events were captured in CARES.
All participating EMS agencies ensure that all OHCA events are reported to CARES by responding to a routine data audit from CARES that requests confirmation that the number of cases reported represents all of the cases in the agency's medical records. Within CARES, the volume of OHCA events per month is compared with historic monthly volumes. Whenever a substantial decrease (i.e., >50%) occurs in the number of events compared with the prior month's total, the local EMS agency contact is notified to determine if the variation was real or the result of a lag in the data-entry process. Tracking regular volumes by EMS and hospital providers also has encouraged compliance with the monthly schedule of data entry.
A CARES data analyst provides data validation and reviews every record for completeness and accuracy. Logic is incorporated into the software for direct online data entry to minimize the number of incomplete fields and implausible data entries. When a missing case is identified or incomplete data are discovered during the ongoing data audit process, the EMS providers who cared for the patient are asked to complete the record or clarify the missing data elements. The proportion of missing data ranges from a low of 1% for patient name to a high of 25% for patient race/ethnicity. Missing records for race/ethnicity are a result of certain communities deciding not to provide these data rather than a result of incomplete data entry by field providers.
Data Security
After a record has been audited and is considered complete, the patient-specific unique identifiers are permanently stripped from the record. The record is stored on the Sansio Inc. server (Duluth, Minnesota) and is accessible only to CARES staff, EMS agency providers, and hospitals that have been granted permission with a secure login and password. CARES uses a restricted-access Internet database that uses secure socket layer encryption technology in transmitting protected health information to its servers to ensure the integrity and privacy of the data.
Quality Improvement
CARES data are used to help communities benchmark and improve their performance for OHCA care. CARES allows participating communities to view their own statistics online confidentially and compare their performance to anonymous aggregated data at the local, regional, or national level. CARES automatically calculates local 911 response intervals, delivery rates for critical interventions (e.g., bystander CPR and public access defibrillation [PAD]), and community rates of survival and functional status at discharge, on the basis of each patient's CPC Scale. An annual report is provided to all participating communities that summarizes local results in comparison to regional and national benchmarks.
EMS agencies have continuous access to their data and can generate survival reports by date ranges. Aggregate de-identified survival reports are shared with all participating sites every 2 months in advance of a regular conference call with EMS medical directors and quality-improvement providers. A confidential report that compares 1) overall survival rates, 2) survival rates of witnessed arrests with an initial shockable rhythm, and 3) bystander CPR rates by community is provided to each site in a bar chart format (Figures 4--6). Starting in 2009, cumulative (beginning October 1, 2005) and annual (calendar year) reports have been generated. These detailed reports include patient demographics, arrest information, and hospital outcomes. In addition, EMS agencies and hospitals are able to query the database for any combination of local outcomes.
CARES convenes a regular users-group conference call to discuss data and quality improvement efforts. Topics have included measurement of response time, public access AED programs, dispatcher-assisted CPR training, and geomapping efforts to facilitate targeted community CPR training. An in-person meeting with site medical directors and registry staff takes place annually and corresponds with a national EMS medical directors conference.
Analytic Methods
Analysis of all OHCA events submitted to the registry during October 1, 2005--December 31, 2010 was conducted using SAS version 9.2 (SAS Institute Inc., Cary, North Carolina). The overall survival rate was calculated for all patients meeting the case definition.In addition, the Utstein survival rate was calculated for a subgroup of patients whose OHCAs were witnessed by a bystander and who had an intial cardiac arrest rhythm of ventricular fibrillation or pulseless ventricular tachycardia. The chi-square statistic was used to obtain differences between categorical variables. All p values <0.05 were deemed statistically significant.
Results
Characteristics of Participating Communities
For 31,689 OHCA events, patient demographics (e.g., age, sex, and race/ethnicity) and aspects of the event (e.g., witnessed, unwitnessed, or bystander intervention) are reported (Tables 2 and 3). The mean age at cardiac arrest was 64.0 years (standard deviation: 18.2), and 61.1% of cases occurred in males (n = 19,360). The proportion of persons with an initially shockable rhythm (i.e., ventricular fibrillation or pulseless ventricular tachycardia) was 23.7%, and 47.3% of arrests were witnessed by a bystander, a first responder, or EMS personnel.
Characteristics of event location (e.g., home, street, and airport) are reported (Table 2). Approximately 66.4% of arrests occurred at a home or residence, and 13.5% occurred at a nursing home or assisted living facility. The remainder of arrests took place in public locations. Retention of incident location allows geographic information systems (GIS) to be used to map events, so local EMS services can examine neighborhood characteristics as well as individual factors and system issues that might influence the likelihood of survival following an OHCA event. Initial cardiac arrest rhythm and neurologic status among survivors are stratified by age group (Figures 7 and 8). An initial shockable rhythm occurred most frequently among persons aged 35--49 years old and those aged 50--64 years. The proportion of survivors who achieved a good CPC scale (CPC = 1) declined progressively by age group, beginning with those aged 18--34 years through those aged ≥80 years.
An Utstein survival report divides arrests into three categories: unwitnessed, witnessed by bystander, and witnessed by EMS personnel (Figure 9). The report then stratifies the arrest by the type of initial cardiac arrest rhythm. This allows for interpretation of Utstein survival rate (witnessed by a bystander with ventricular fibrillation or pulseless ventricular tachycardia as the initial cardiac rhythm), which was 30.1% in this dataset (Table 3).
On the basis of local EMS agency protocols, 21.6% of patients were pronounced dead after resuscitation efforts were terminated in the prehospital setting. The survival rate to hospital admission was 26.3%, and the overall survival rate to hospital discharge was 9.6%. Although 36.7% of OHCA events were witnessed by a bystander, only 43.8% of these arrests involved persons who received bystander CPR, and only 3.7% of those persons were treated with an AED before the arrival of 911.
A subgroup analysis was performed among patients with OHCA events that were not witnessed by EMS providers to evaluate rates of bystander CPR. After exclusion of 3,400 OHCA events that occurred after the arrival of EMS, bystander CPR information was analyzed for 28,289 events (Table 4). Whites were more likely to receive bystander CPR than blacks, Hispanics, or persons of other races/ethnicities (p<0.001). Among whites, 40.2% received bystander CPR, compared with 32.8% of blacks and 33.7% of Hispanics. No significant difference was noted in receiving bystander CPR between male and female patients (p = 0.821). Persons who had a witnessed event were more likely than persons whose event was not witnessed to receive bystander CPR (43.8% versus 32.1%; p<0.001), and an event that occurred in a public location had a higher percentage of bystander CPR than one that occurred in a private setting (48.3% versus 34.0%; p<0.001). Overall survival to hospital discharge of patients whose event was not witnessed by EMS was 8.5%. Of these, patients who received bystander CPR had a higher rate of overall survival (11.2%) than those who did not receive CPR (7.0%).
Discussion
CARES data are used for quality improvement and surveillance efforts. The overall survival to hospital discharge rate was 9.6%. This is higher than in certain previous reports (6.7%--8.4%) (10). CARES is a voluntary registry, and agencies that choose to participate might have more resources to dedicate to quality improvement initiatives and thus might have greater survival rates than other agencies. However, these low survival rates for an OHCA event are of public health concern because, despite advances in technology and resuscitation science, these rates have remained virtually unchanged for >3 decades (10). The Utstein survival rate in this dataset was 30.1%. Utstein survival is defined as the rate of survival among persons whose arrests were witnessed by a bystander and who had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia. These patients have the greatest survival potential and are the most likely to respond to CPR or defibrillation. Utstein suvival provides a better measurement tool for determining the effectiveness of an intervention, such as increased CPR training within a community. Since Utstein survival is determined for a subset of the overall dataset and represents patients who are most likely to survive, Utstein survival rates are consistently higher than overall survival rates. For example, a recent study examining the effectiveness of active compression-decompression CPR showed an overall survival to hospital discharge rate of 10% in patients who received standard CPR and an Utstein survival rate of 27% in this same group (21). Patients who received bystander CPR had a higher rate of overall survival (11.2%) than those who did not receive bystander CPR (7.0%; p<0.01). Improving community bystander CPR rates is an important step towards improving OHCA survival.
CARES data suggest that disparities exist in the provision of bystander CPR by race/ethnicity. Whites were more likely to receive bystander CPR than blacks, Hispanics, or persons of other races/ethnicities. CARES data are used to analyze neighborhood disparities regarding incidence of cardiac arrest and low rates of bystander CPR. An analysis of CARES data from Fulton County, Georgia, identified 14 census tracts with a high incidence of OHCA and low rate of bystander CPR that had more black residents, lower household income, and lower education levels than other census tracts in the rest of Fulton County (22). Interventions (e.g., increased CPR training and AED placement) targeted at neighborhoods with these disparities are critical to the reduction of socioeconomic disparities in OHCA events. CARES data reinforce previous research indicating increased survival benefit when bystander CPR occurred. A systematic review and meta-analysis of predictors of survival determined that, for bystander CPR, the number of persons needed to receive treatment to save one life was 24 patients in communities with high baseline survival rates and 36 in communities with low rates of survival; this study suggested that efforts to increase survival rates from OHCA include targeted CPR training (10,22).
Two communities (Columbus, Ohio and San Diego, California) are using CARES data to identify local health disparities in both the provision of bystander CPR and AED use. Using GIS mapping techniques, neighborhoods have been identified that have high rates of cardiac arrest and low rates of bystander CPR. These neighborhoods are now being targeted using culturally sensitive CPR interventions developed with the help of citizens from within these communities (David Keseg, MD, Jim Dunford, MD, personal communications, 2011).
Data collected during the initial phase of the CARES program (2005--2010) have helped participating communities identify opportunities to improve care for persons who experience an OHCA event. The registry can be used to monitor EMS performance and selected aspects of pre-hospital care to improve treatment and increase rates of survival following an OHCA event. CARES data confirm that patients who are helped by bystanders and who are treated promptly by EMS providers in the field are most likely to survive.
Tracking performance longitudinally will help communities better understand which elements of the response system are working well and which elements need improvement. The 2010 American Heart Association Guidelines for CPR and Emergency Cardiovascular Care describe the quality improvement elements of a resuscitation system as 1) systematic evaluation of resuscitation care and outcome, 2) benchmarking with stakeholder feedback, and 3) strategic efforts to address identified deficiencies (8).
CARES data can be used to evaluate new interventions and treatments in OHCA care and can guide targeted training efforts within communities. In 2010, CARES included therapeutic hypothermia as a required data field for both EMS and hospital providers to determine the frequency of this post resuscitation treatment. A pilot AED registry to track device usage and map existing locations of devices at public sites is in the planning stage. CARES records the address of a cardiac arrest event, enabling the use of GIS technology to identify community-level disparities related to bystander CPR and AED usage. As communities work to increase training in bystander CPR, improve awareness of AED availability, and use more effective CPR techniques, CARES data can be analyzed to evaluate the success of these interventions and contribute to improved survival on a local, regional, statewide, or national level.
Starting in 2011, CARES is expanding to statewide participation in Arizona, Hawaii, Minnesota, North Carolina, Pennsylvania, and Washington. Statewide participation allows enrollment of additional communities of different sizes and population densities to be included in the registry. In addition, state-level participation allows better communication and collaboration between state and local EMS providers.
Limitations
The data presented in this report are subject to at least six limitations. First, although as part of the audit process, participating agencies are asked to confirm that all cardiac arrest cases are included in the CARES registry, some cardiac arrests in a community might be missed, resulting in selection or reporting bias. EMS field providers might fail to return patient care documentation, and records with incorrect or missing name and date of birth information make it difficult for hospitals to locate the patient and provide a hospital outcome. CARES cannot capture OHCA events when 911 or EMS are not notified, resulting in lack of detection of some OHCA events. Second, EMS providers work in high-stress environments and are commonly collecting information after the event. Recall bias among EMS providers, as well as bystanders, might affect the quality of the data. Third, CARES primarily represents larger, urban areas. The majority of communities in CARES have a population of >200,000 persons. This could potentially create a selection bias for denser populations, more infrastructure, greater resources, and more established EMS systems, limiting generalizability of CARES results. Expansion at the state level allows CARES to be more inclusive and include communities of varied size and population densities. Fourth, EMS providers might vary on their interpretation of an event. Participants are asked to classify an arrest as having a cardiac etiology, unless it is known or likely to have been caused by a noncardiac cause. This is a process of exclusion and is based on clinical opinion. The presumption of cardiac etiology could potentially cause misclassification of the event. Fifth, since CARES is designed as a registry system rather than a research database, it does not capture highly detailed information on episodes of OHCA or detailed treatment information. CARES does not measure the rate, depth, or influence of interruptions in chest compressions, which would help to understand better the effectiveness and quality of CPR. Response time by EMS providers and first responders is measured, but aggregate reports are not generated for benchmarking purposes because of concerns regarding variation in how these times are measured. Finally, the data- collection process protects the confidentiality of subjects by de-identifying records once they have been deemed accurate and complete. This prevents researchers from identifying and contacting survivors or the next-of-kin of those who died, which can limit understanding of patient outcomes after hospitalization or the influence of community members' efforts during an OHCA event before the arrival of 911 responders.
Despite these limitations, which reflect the fact that public health surveillance serves different goals than clinical research, participation in CARES is provided at no cost to participants, and the registry is easy to adopt and maintain. Personnel costs related to data entry must be absorbed by participating agencies; however, data-collection activity is limited to a small number of high-impact parameters, which decreases the data-entry burden. In addition, the data CARES collects focuses attention on the performance metrics that matter most to EMS medical directors, agency directors, and quality-assurance personnel.
Conclusion
The data provided in this report indicate the need for prompt and effective resuscitation efforts. Provision of optimal care at the scene is essential to survival. If a pulse is not restored before EMS transport, additional efforts at the receiving hospital almost invariably fail (23).
Education of public officials and community members about the importance of increasing rates of bystander CPR far beyond the current 33.3% and promoting use of early defibrillation by lay and professional rescuers are critical to improving survival of OHCA events. CARES data can be used at the community level to target interventions (e.g., bystander CPR training and AED placement) and assess their effectiveness. CDC uses CARES data for cardiovascular surveillance efforts and makes data available to the public at http://apps.nccd.cdc.gov/NCVDSS_DTM. As statewide CARES registries become available, the data will be used for state-specific OHCA surveillance efforts.
With expansion to state-level surveillance, CARES will enable local and state public health departments and EMS agencies to better coordinate their efforts. Such coordination can improve the quality of EMS care and thus increase the proportion of persons who survive an OHCA event.
Acknowledgments
This report is based in part on data provided by members of the CARES Surveillance Group: Mike Levy, MD, Anchorage, Alaska; Joseph Barger, MD, Contra Costa County, California; James V. Dunford, MD, San Diego County, California; Karl Sporer, MD, San Francisco County, California; Angelo Salvucci, MD, Ventura County, California; David Ross, MD, Colorado Springs, Colorado; Christopher Colwell, MD, Denver, Colorado; Dorothy Turnbull, MD, Stamford, Connecticut; Rob Rosenbaum, MD, New Castle County, Delaware; Mark Waterman, MD, Atlanta, Georgia; Richard Dukes, MD, Clayton County, Georgia; Raymond Fowler, MD, Douglas County, Georgia; John Lloyd, MD, Forest Park, Georgia; Art Yancey, MD, Atlanta, Georgia; Earl Grubbs, MD, Gwinnett County, Georgia; John Lloyd, MD, Hapeville, Georgia; Jonathan Morris, MD, Metro Atlanta, Georgia; Stephen Boyle, MD, Metro Atlanta, Georgia; Troy Johnson, MD, Newton County, Georgia; Christopher Wizner, MD, Puckett County, Georgia; Melissa White, MD, Metro Atlanta, Georgia; Sabina Braithwaite, MD, Sedgwick County, Kansas; Sophia Dyer, MD, Boston, Massachusetts; Gary Setnik, MD, Cambridge, Massachusetts; Bob Hassett, MD, Springfield, Massachusetts; John Santor, MD, Springfield, Massachusetts; Bob Swor, MD, Oakland County, Michigan; Todd Chassee, MD, Kent County, Michigan; Charlie Lick, MD, Hennepin County, Minnesota; Mike Parrish, Hennepin County, Minnesota; Darel Radde, Hennepin County, Minnesota; Brian Mahoney, MD, Hennepin County, Minnesota; Darell Todd, Hennepin County, Minnesota; Joseph Salomone, MD, Kansas City, Missouri; Eric Ossman, MD, Durham, North Carolina; Brent Myers, MD, Wake County, North Carolina; Lee Garvey, MD, Charlotte, North Carolina; James Camerson, MD, New Jersey; David Slattery, MD, Las Vegas, Nevada; Joseph Ryan, MD, Reno, Nevada; Jason McMullan, MD, Cincinnati, Ohio; David Keseg, MD, Columbus, Ohio; James Leaming, MD, Hershey, Pennsylvania; BK Sherwood, MD, Hilton Head, South Carolina; Jeff Luther, MD, Sioux Falls, South Dakota; Corey Slovis, MD, Nashville, Tennessee; Paul Hinchey, MD, Austin-Travis County, Texas; Michael Harrington, MD, Baytown, Texas; John Griswell, MD, Jeff Beeson, MD, Fort Worth, Texas; David Persse, MD, Houston, Texas; Mark Gamber, MD, Plano, Texas; Joe Ornato, MD, Richmond, Virginia.
References
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation 2011;123:e18--209.
- Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. Circulation 2004;110:3385--97.
- Nichol G, Rumsfeld J, Eigel B, et al. Essential features of designating out-of-hospital cardiac arrest as a reportable event. Circulation 2008; 117:2299--308.
- Rea TD, Fahrenbruch C, Culley L, et al. CPR with chest compression alone or with rescue breathing. N Engl J Med. 2010;363:423--33.
- Bobrow BJ, Spaite DW, Berg RA, et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 2010;304:1447--54.
- Bobrow BJ. Survival from out-of-hospital cardiac arrest after chest compression-only CPR. JAMA 2011;305:147; author reply 148.
- Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the "chain of survival" concept. Circulation 1991;83:1832--47.
- Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPR overview. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122(Suppl 3):S676--84.
- Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008;300:1423--31.
- Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63--81.
- Rea TD, Eisenberg MS, Sinibaldi G, White RD. Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation 2004;63:17--24.
- National Highway Traffic Safety Administration. Emergency medical services agenda for the future. Washington, DC: US Department of Transportation, National Highway Traffic Safety Administration; 1996.
- Sayre MR, White LJ, Brown LH, McHenry SD. National EMS research agenda. Prehosp Emerg Care 2002;6(3 Suppl):S1--43.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Emergency medical services: at the crossroads. Washington, DC: The National Academies Press; 2007.
- US Department of Health and Human Services. Healthy people 2020: heart disease and stroke. Washington, DC: US Department of Health and Human Services; 2011. Available at http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=21. Accessed July 20, 2011.
- Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. Circulation 1991;84:960--75.
- McNally B, Stokes A, Crouch A, Kellermann AL. CARES: Cardiac Arrest Registry to Enhance Survival. Anns Emerg Med 2009;54:674--83.
- Intermountain Injury Control Research Center. The NEMSIS Technical Assistance Center. Available at http://www.nemsis.org. Accessed July 20, 2011.
- University of Washington Cardiac Clinical Trials Center. Resuscitation outcomes consortium. Available at https://roc.uwctc.org. Accessed July 20, 2011.
- CDC. HIPAA privacy rule and public health: guidance from CDC and the U.S. Department of Health and Human Services. MMWR 2003;52(Suppl).
- Aufderheide TP, Frascone RJ, Wayne MA, et al. Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitation with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: a randomised trial. Lancet 2011;377:301--11.
- Sasson C, Keirns CC, Smith D, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter? Ann Intern Med 2010;153:19--22.
- Sasson C, Hegg AJ, Macy M, Park A, Kellermann A, McNally B. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA 2008;300:1432--8.
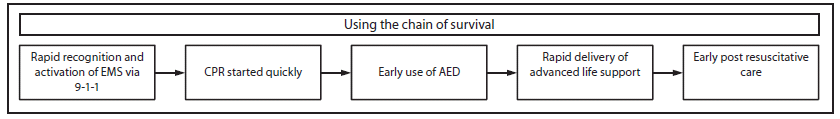
Abbreviations: EMS = emergency medical services; CPR = cardiopulmonary resuscitation; AED = automated external defibrillator.
Source: Adapted from Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPR overview. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122:S676--84.
Alternate Text: The figure above shows the five critical actions needed to improve chances of survival of an out-of-hospital cardiac arrest: 1) active recognition and activation of Emergency Medical Services by calling 9-1-1, 2) starting cardiopulmonary resuscitation quickly, 3) early use of automated external defibrillator, 4) rapid delivery of advanced live support, and 5) early post resuscitative care.
FIGURE 2. Cardiac arrest surveillance participant sites --- Cardiac Arrest Registry to Enhance Survival, United States, October 1, 2005--December 31, 2010
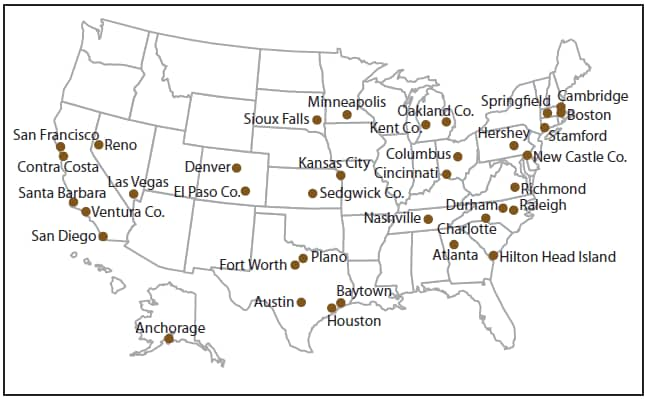
Alternate Text: The figure above shows a map of the United States indicating the cities in which emergency medical services agencies participate in the Cardiac Arrest Registry to Enhance Survival. These cities are located in 20 states: Alaska, California, Colorado, Connecticut, Delaware, Georgia, Kansas, Massachusetts, Michigan, Minnesota, Missouri, Nevada, North Carolina, Ohio, Pennsylvania, South Carolina, South Dakota, Tennessee, Texas, and Virginia.
FIGURE 3. Cardiac Arrest Registry to Enhance Survival data entry form --- United States, October 1, 2005--December 31, 2010
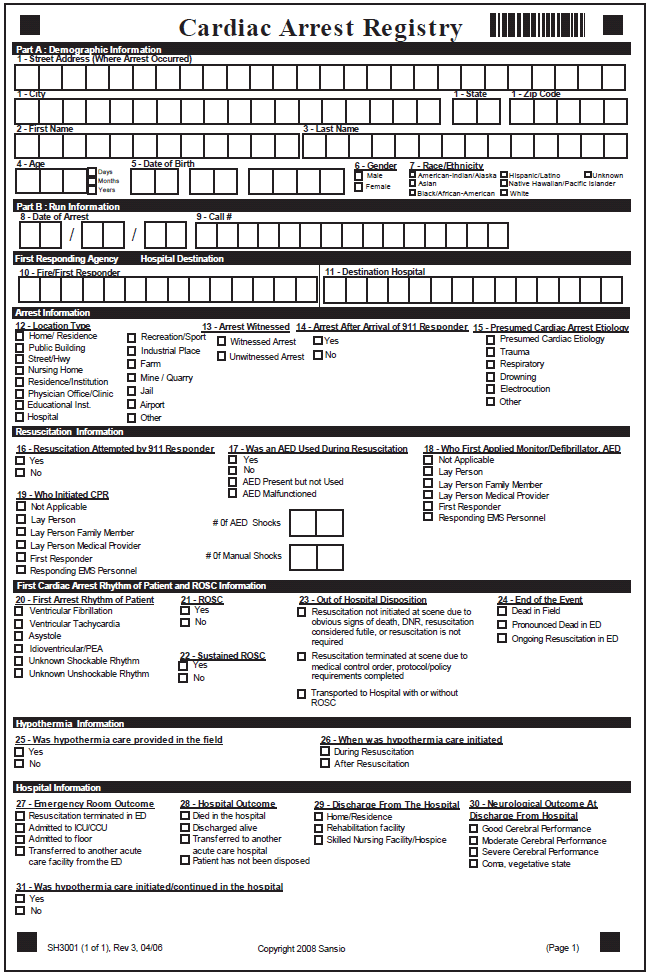
Alternate Text: The figure above shows a data entry form used to collect information on out-of-hospital cardiac arrests for the Cardiac Arrest Registry to Enhance Survival.
|
CPC 1. Good cerebral performance. Conscious, alert, able to work; might have mild neurologic or psychologic deficit. CPC 2. Moderate cerebral disability. Conscious, sufficient cerebral function for independent activities of daily life. Able to work in sheltered environment. CPC 3. Severe cerebral disability. Conscious, dependent on others for daily support because of impaired brain function. Ranges from ambulatory state to severe dementia or paralysis. CPC 4. Coma or vegetative state. Any degree of coma without the presence of all brain death criteria. Unawareness, even if appears awake (vegetative state) without interaction with environment; might have spontaneous eye opening and sleep/awake cycles. Cerebral unresponsiveness. ____________________________ Source: Safar P. Resuscitation after brain ischemia. In: Grenvik A, Safar P, eds. Brain failure and resuscitation. New York, NY: Churchill Livingston; 1981;155--84. |
FIGURE 4. Cumulative overall survival rates, by participating emergency medical services agency --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010*
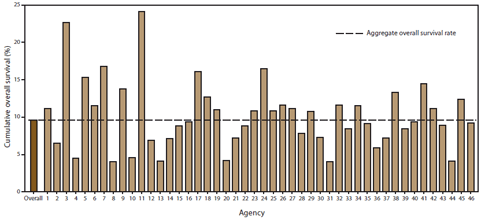
* Agencies sorted by total number of out-of-hospital cardiac arrest events in CARES (from low to high; range: 18--5,434).
Alternate Text: The figure above shows site-specific and cumulative overall survival rates for out-of-hospital cardiac arrest events by participating emergency medical services agency for October 1, 2005- December 31, 2010. Results varied by agency; the overall survival rate was 10%.
FIGURE 5. Cumulative Utstein survival rates, by participating emergency medical services agency --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010*
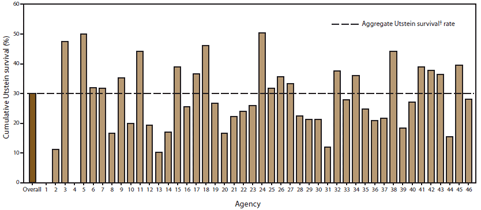
* Agencies sorted by total number of out-of-hospital cardiac arrest events in CARES (from low to high).
† Utstein survival refers to survival to hospital discharge of persons whose cardiac arrest events were witnessed by a bystander and had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia (range: 0--598).
Alternate Text: The figure above shows site-specific and aggregate Utstein survival rates for out-of-hospital cardiac arrest events by participating emergency medical services agency for October 1, 2005- December 31, 2010. Utstein survival refers to survival to hospital discharge of persons whose cardiac arrest events were witnessed by a bystander and had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia. Results varied by agency; the overall Utstein survival rate was 30%.
FIGURE 6. Cumulative bystander cardiopulmonary resuscitation (CPR), by participating emergency medical services agency --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010*
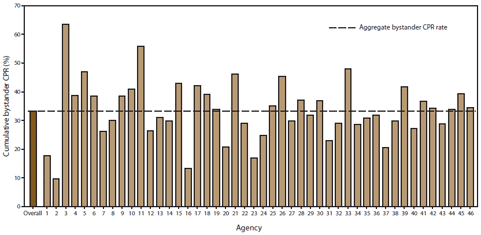
Abbreviation: CPR = cardiopulmonary resuscitation.
* Agencies sorted by total number of out-of-hospital cardiac arrest events in CARES (from low to high; range: 18--5,434).
Alternate Text: The figure above shows site-specific and aggregate bystander CPR rates for out-of-hospital cardiac arrest events by participating emergency medical services agency for October 1, 2005- December 31, 2010. Rates varied by agency; the overall bystander CPR rate was 30%.
FIGURE 7. Presenting arrest rhythm of persons who experienced an out-of-hospital cardiac arrest, by age group* --- Cardiac Arrest Registry to Enhance Survival, United States, October 1, 2005--December 31, 2010
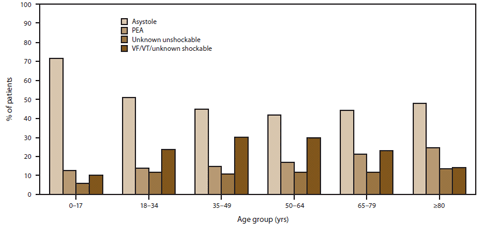
Abbreviations: PEA = pulseless electrical activitiy; VF = ventrical fibrillation; VT = pulseless ventricular tachycardia.
* N = 0--17 years: 590; 18--34 years: 1,162; 35--49 years: 4,145; 50--64 years: 9,538; 65--79 years: 9,082; and ≥80 years: 7,046. Initial rhythm missing for 126 patients.
Alternate Text: The figure above shows presenting arrest rhythm of persons who experienced an out-of-hospital cardiac arrest during October 1, 2005-December 31, 2010 by age group. Rates varied by age group and four factors: asystole, pulseless electrical activity, ventricular fibrillation, and pulseless ventricular tachycardia.
FIGURE 8. Neurologic status* among survivors of an out-of-hospital cardiac arrest, by age group† --- Cardiac Arrest Registry to Enhance Survival, United States, October 1, 2005--December 31, 2010
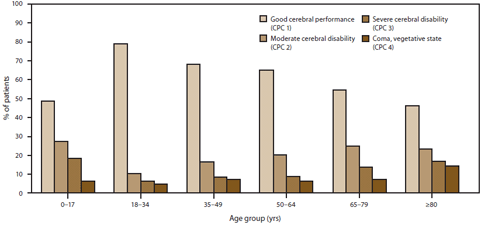
Abbreviation: CPC = cerebral performance category.
* Neurologic status missing for 353 patients.
† N = 0--17 years: 33; 18--34 years: 109; 35--49 years: 455; 50--64 years: 1,059; 65--79 years: 751; and ≥80 years: 282.
Alternate Text: The figure above shows the neurologic status among survivors of an out-of-hospital cardiac arrest during October 1, 2005- December 31, 2010 by age group and four cerebral performance categories: CPC 1 (good cerebral performance), CPC 2 (moderate cerebral disability), CPC 3 (severe cerebral disability), and CPC 4 (coma, vegetative state). Results varied by age group.
FIGURE 9. Utstein survival report showing survival for out-of-hospital cardiac arrest, stratified by witness category --- United States, October 1, 2005--December 31, 2010
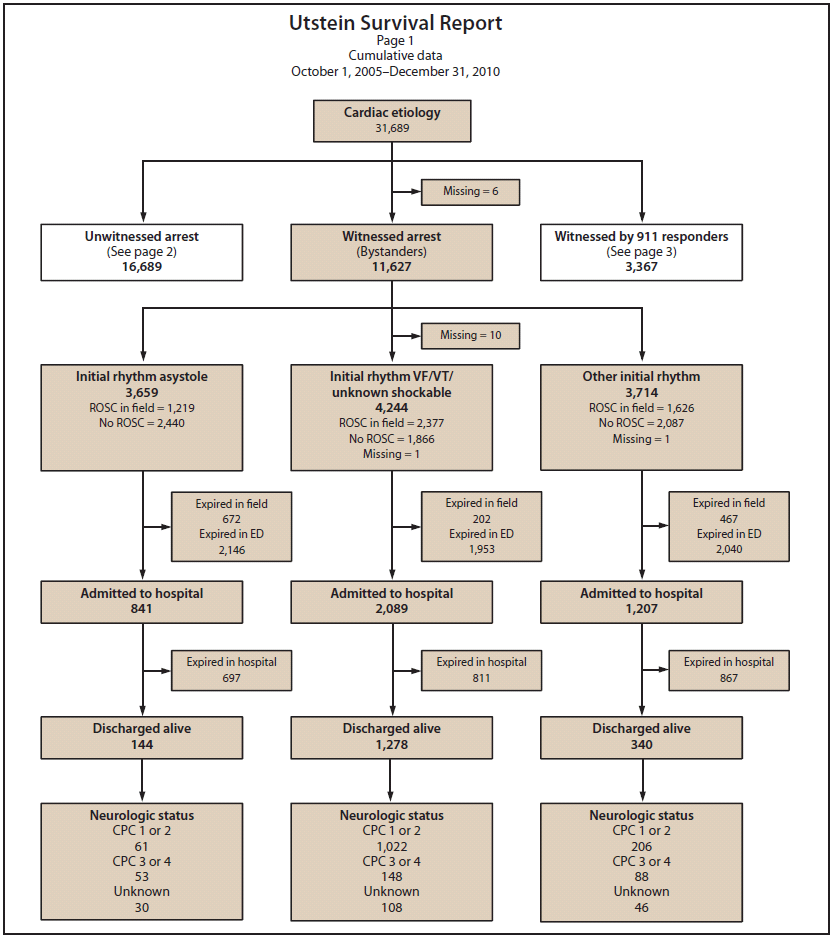
Abbreviations: ROSC = return of spontaneous circulation; VF = ventricular fibrillation; VT = pulseless ventricular tachycardia; CPC = cerebral performance category; ED = emergency department; expired = died.
Alternate Text: The figure above shows an Utstein survival report showing survival for out-of-hospital cardiac arrest during October 1, 2005- December 31, 2010 stratified by witness category. Utstein survival refers to survival to hospital discharge of persons whose cardiac arrest events were witnessed by a bystander and had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia.
FIGURE 9. (Continued) Utstein survival report showing survival for out-of-hospital cardiac arrest, stratified by witness category --- United States, October 1, 2005--December 31, 2010
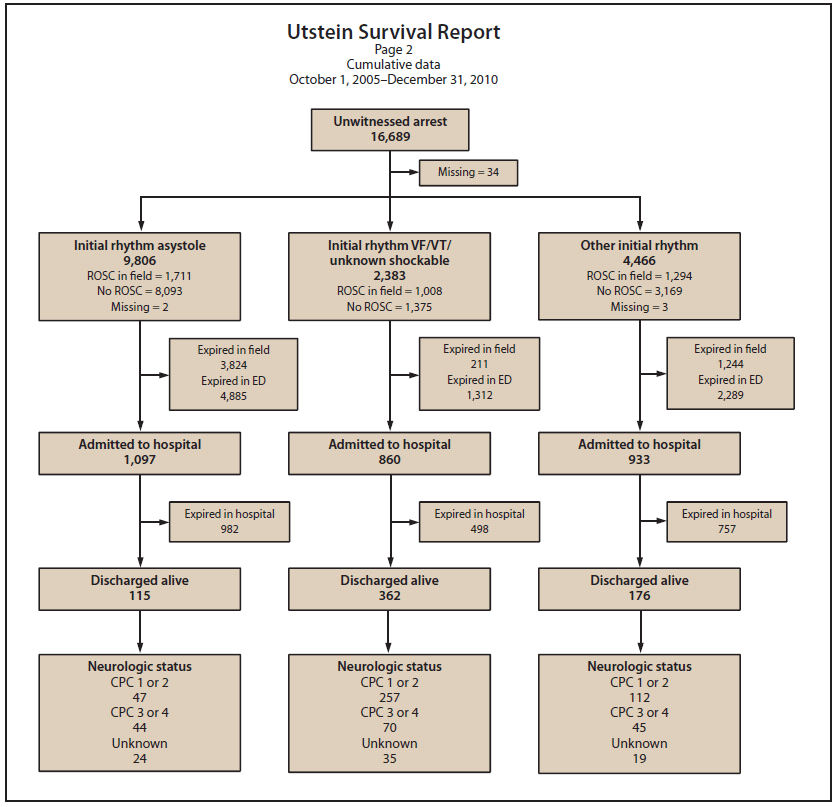
Abbreviations: ROSC = return of spontaneous circulation; VF = ventricular fibrillation; VT = pulseless ventricular tachycardia; CPC = cerebral performance category; ED = emergency department; expired = died.
Alternate Text: The figure above shows an Utstein survival report showing survival for out-of-hospital cardiac arrest during October 1, 2005- December 31, 2010 stratified by witness category. Utstein survival refers to survival to hospital discharge of persons whose cardiac arrest events were witnessed by a bystander and had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia.
FIGURE 9. (Continued) Utstein survival report showing survival for out-of-hospital cardiac arrest, stratified by witness category --- United States, October 1, 2005--December 31, 2010
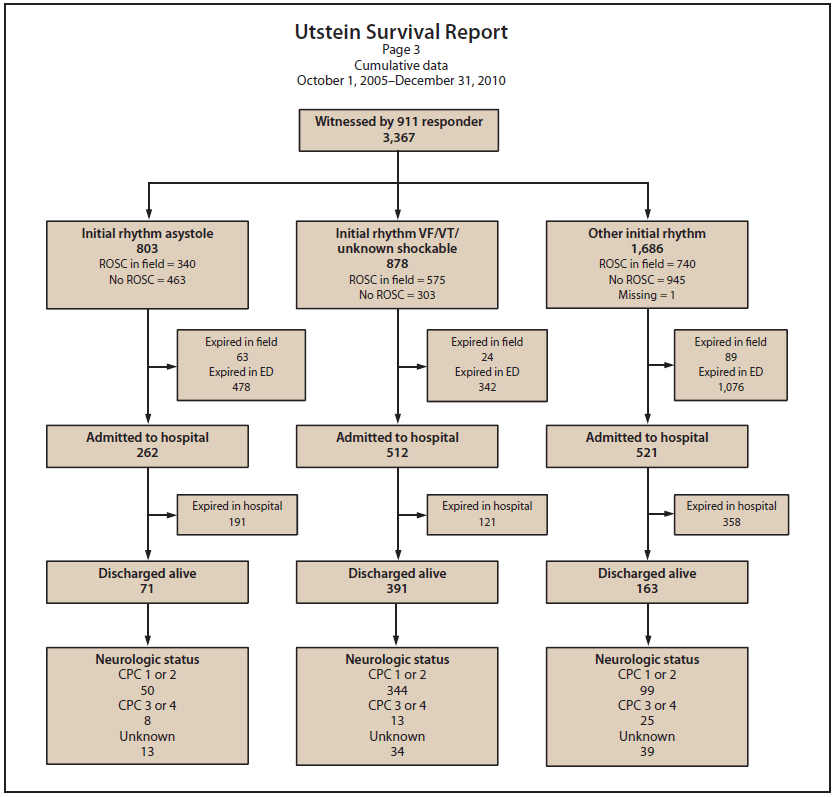
Abbreviations: ROSC = return of spontaneous circulation; VF = ventricular fibrillation; VT = pulseless ventricular tachycardia; CPC = cerebral performance category; ED = emergency department; expired = died.
Alternate Text: The figure above shows an Utstein survival report showing survival for out-of-hospital cardiac arrest during October 1, 2005- December 31, 2010 stratified by witness category. Utstein survival refers to survival to hospital discharge of persons whose cardiac arrest events were witnessed by a bystander and had an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.


