Update: Influenza Activity — United States, October 4–November 28, 2015
, MPH1; , MPH1; , MPH1; , MPH1; , MPH1; , DSc1; , MPH1; , PhD1; , MD1; , MD1; , MD1; , MS1; , PhD1; , MD1; 1; , PhD1; , PhD1; , PhD1; , MA1; , PhD1; , MD1; , MPH1
CDC collects, compiles, and analyzes data on influenza activity year-round in the United States. The influenza season generally begins in the fall and continues through the winter and spring months; however, the timing and severity of circulating influenza viruses can vary by geographic location and season. Influenza activity in the United States remained low through October and November in 2015. Influenza A viruses have been most frequently identified, with influenza A (H3) viruses predominating. This report summarizes U.S. influenza activity* for the period October 4–November 28, 2015.†
Viral Surveillance
World Health Organization (WHO) collaborating laboratories and National Respiratory and Enteric Virus Surveillance System (NREVSS) laboratories, which include both public health and clinical laboratories located throughout the United States, participate in virologic surveillance for influenza. Beginning with the 2015–16 influenza season, data for public health and clinical laboratories are presented separately because influenza testing practices differ. Clinical laboratories test respiratory specimens for diagnostic purposes, and data from these laboratories provide useful information regarding the timing and intensity of influenza activity. Public health laboratories primarily test specimens for surveillance purposes to understand which influenza viruses are circulating throughout their jurisdictions and which population groups are being affected. The age group distribution of influenza positive tests reported from public health laboratories is summarized.
Clinical laboratories in the United States tested 102,675 respiratory specimens collected during October 4–November 28, 2015, for influenza viruses. Among these, 1,268 (1.2%) tested positive for influenza (Figure 1); 772 (60.9%) were influenza A viruses, and 496 (39.1%) were influenza B viruses.
Public health laboratories in the United States tested 8,488 respiratory specimens collected during October 4–November 28, 2015, for influenza viruses. Among these, 404 tested positive for influenza (Figure 2); 333 (82.4%) were influenza A viruses, and 71 (17.6%) were influenza B viruses. Of the 333 influenza A viruses, 317 (95.2%) were subtyped; 55 (17.4%) were influenza A(H1N1)pdm09 (pH1N1), and 262 (82.6%) were influenza A (H3) viruses. Of the 71 influenza B viruses, 21 (29.6%) had lineage determined; 13 (61.9%) belonged to the B/Yamagata lineage, and eight (38.1%) belonged to the B/Victoria lineage. Since October 4, influenza-positive test results have been reported from all 50 states, the District of Columbia, Guam, and Puerto Rico, representing all 10 U.S. Department of Health and Human Services (HHS) regions.§ Influenza A viruses have predominated nationally and in all 10 HHS regions.
During October 4–November 28, 2015, age data were available for 370 positive influenza test results, including 31 (8.4%) in children aged 0–4 years, 96 (26.0%) in persons aged 5–24 years, 130 (35.1%) in persons aged 25–64 years, and 113 (30.5%) in persons aged ≥65 years. Influenza A (H3) viruses were predominant in all age groups, accounting for a proportion of influenza positives ranging from 41.9% (ages 0–4 years) to 84.1% (ages ≥65 years). The largest number of influenza A pH1N1 viruses were reported in persons aged 25–64 years. The largest number of influenza B viruses were reported in persons aged 5–24 years and 25–64 years.
Influenza Virus Characterization
WHO collaborating laboratories in the United States are requested to submit a subset of influenza-positive respiratory specimens to CDC for further virus characterization. CDC characterizes influenza viruses through one or more laboratory tests including genome sequencing, or hemagglutination inhibition (HI), or neutralization assays. These data are used to compare how similar currently circulating influenza viruses are to the influenza vaccine reference viruses, and to monitor for changes in circulating influenza viruses. Most viruses tested are propagated in mammalian cell cultures because isolation rates of human influenza viruses are higher in mammalian cell cultures than in eggs. However, egg-propagated vaccine viruses are used widely for production of influenza vaccines because most influenza vaccines are egg-based. Propagation of influenza viruses in eggs can lead to isolation of viruses that differ genetically and antigenically from corresponding clinical specimens isolated in mammalian cell cultures. In addition, mammalian cell-propagated viruses are genetically more representative of viruses present in original clinical specimens (1,2). Antigenic and genetic characterization of circulating viruses is performed using both mammalian cell- and egg-propagated reference viruses.
Historically HI data have been used most commonly to assess the similarity between reference viruses and circulating viruses. Although vaccine effectiveness field studies must be conducted to actually determine how well the vaccine is working, these laboratory data are used to determine whether changes in the virus have occurred that could affect vaccine effectiveness. Beginning with the 2014–15 season and to date, however, a proportion of influenza A (H3N2) viruses have not yielded sufficient hemagglutination titers for antigenic characterization by HI. For all viruses characterized at CDC laboratories, whole genome sequencing is performed to determine the genetic group identity of these circulating viruses. For the subset of viruses that do not yield sufficient hemagglutination titers, antigenic properties of those viruses are inferred using results from viruses within the same genetic group that have been characterized antigenically.
Since October 1, 2015, CDC has antigenically or genetically characterized 62 specimens (18 influenza A (H1N1)pdm09, 43 influenza A (H3N2), and one influenza B/Yamagata lineage). A total of 43 H3N2 viruses have been genetically sequenced and all 43 viruses belonged to genetic groups for which a majority of antigenically characterized viruses were similar to the cell-propagated reference virus A/Switzerland/9715293/2013 representing the influenza A (H3N2) component of the 2015–16 Northern Hemisphere vaccine. A total of 35 viruses (18 influenza A (H1N1)pdm09, 16 influenza A (H3N2), and one B/Yamagata lineage) collected since October 1, 2015, have been antigenically characterized. All A(H1N1)pdm09, all B viruses, and 15 of the 16 A(H3N2) viruses were similar to the reference viruses representing the 2015–16 Northern Hemisphere influenza vaccine components.
Antiviral Resistance of Influenza Viruses
The WHO Collaborating Center for Surveillance, Epidemiology, and Control of Influenza at CDC tested 56 influenza virus specimens (11 influenza A (H1N1)pdm09, 33 influenza A (H3N2) and 12 influenza B) collected since October 1, 2015, in the United States for resistance to the influenza neuraminidase inhibitor antiviral medications oseltamivir, zanamivir, and peramivir, which are the drugs currently approved for use against seasonal influenza. All 56 influenza viruses tested were sensitive to all three antiviral medications. High levels of resistance to the adamantanes (amantadine and rimantadine) persist among influenza A (H1N1)pdm09 and (H3N2) viruses. Adamantane drugs are not recommended for use against influenza at this time.
Outpatient Illness Surveillance
Since October 4, the weekly percentage of outpatient visits for influenza-like illness (ILI)¶ reported by approximately 1,800 U.S. Outpatient ILI Surveillance Network (ILINet) providers in 50 states, New York City, Chicago, the U.S. Virgin Islands, Puerto Rico, and the District of Columbia, has ranged from 1.3% to 1.9% and has remained below the national baseline** of 2.1% (Figure 3). Peak weekly percentages of outpatient visits for ILI ranged from 2.4% to 7.6% from the 1997–98 through 2014–15 influenza seasons, excluding the 2009 pandemic. Data collected in ILINet are used to produce a measure of ILI activity†† by jurisdiction. During surveillance week 47, Puerto Rico and two states (Oklahoma and South Carolina) experienced moderate ILI activity, and four states (Arizona, Mississippi, New Jersey, and Virginia) experienced low ILI activity. Minimal ILI activity was experienced in New York City and 44 states (Alabama, Alaska, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Mexico, New York, North Carolina, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, South Dakota, Tennessee, Texas, Utah, Vermont, Washington, West Virginia, Wisconsin, and Wyoming). Data were insufficient to calculate an ILI activity level for the District of Columbia.
Geographic Spread of Influenza Activity
For the week ending November 28 (week 47), Guam reported widespread geographic spread of influenza,§§ Puerto Rico reported regional spread, and seven states (Iowa, Maryland, Massachusetts, New Hampshire, North Carolina, Oregon, and Utah) reported local spread. The District of Columbia, the U.S. Virgin Islands, and 38 states (Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Kansas, Kentucky, Louisiana, Maine, Michigan, Minnesota, Missouri, Montana, Nebraska, Nevada, New Jersey, New Mexico, New York, North Dakota, Ohio, Oklahoma, Pennsylvania, South Carolina, South Dakota, Texas, Vermont, Washington, West Virginia, Wisconsin, and Wyoming) reported sporadic spread. Five states (Alabama, Mississippi, Rhode Island, Tennessee, and Virginia) reported no influenza activity.
Pneumonia- and Influenza-Associated Mortality
CDC tracks pneumonia and influenza (P&I)–associated deaths through two systems, the National Center for Health Statistics (NCHS) Mortality Surveillance System and the 122 Cities Mortality Reporting System. Beginning during the 2015–16 season, data from the newer NCHS system will be the principal component of the U.S. mortality surveillance system. NCHS mortality data are presented by the week that the death occurred, whereas the 122 Cities Mortality Reporting System data are reported the week that the death certificate was registered. The length of time from the occurrence of a death until registration of the death certificate in the vital statistics office can vary considerably; therefore, these two data sources produce different percentages. Presenting data by the week of the death, rather than the date of filing of the death certificate more accurately reflects the timing of P&I mortality. The percentage of P&I deaths from each system should be compared with the corresponding system-specific baselines and thresholds.
Through the NCHS Mortality Surveillance System, the percentages of deaths associated with P&I are released 2 weeks after the week of death to allow for collection of sufficient data to produce a stable P&I mortality percentage. Based on NCHS data available December 3, 5.9% (1,370 of 23,191) of all U.S. deaths occurring during the week ending November 14, 2015 (week 45) were classified as resulting from P&I. This percentage is below the epidemic threshold¶¶ of 6.8% for week 45. Since October 4, the weekly percentage of deaths attributed to P&I ranged from 5.9% to 6.2% and has not exceeded the epidemic threshold this season. Peak weekly percentages of deaths attributable to P&I during the previous five influenza seasons ranged from 8.7% during the 2011–12 season to 11.1% during the 2012–13 season.
During the week ending November 28 (week 47), P&I was reported as an underlying or contributing cause of 6.1% (524 of 8,634) of all deaths reported to the 122 Cities Mortality Reporting System. This percentage is below the epidemic threshold of 6.5% for the week. Since October 4, the weekly percentage of deaths attributed to P&I ranged from 5.2% to 6.1% and has not exceeded the epidemic threshold so far this season. Peak weekly percentages of deaths attributable to P&I in the previous five seasons ranged from 7.8% during the 2011–12 season to 9.9% during the 2012–13 season.
Influenza-Associated Pediatric Mortality
As of November 28 (week 47), two influenza-associated pediatric deaths have been reported to CDC during the 2015–16 influenza season, both of which occurred during week 44 (the week ending November 7, 2015). One death was associated with an influenza A virus for which no subtyping was performed, and one death was associated with an influenza B virus. The number of influenza-associated pediatric deaths reported to CDC in the previous three seasons ranged from 111 during the 2013–14 season to 171 during the 2012–13 season. During the 2009 pandemic, 358 pediatric deaths were reported from April 15, 2009, through October 2, 2010 (historically, influenza seasons include data from October [week 40] through September [week 39] of the following year).
Discussion
Influenza activity in the United States for the 2015–16 season remained low during October 4–November 28, 2015. Although the timing of influenza activity can vary, peak activity in the United States most commonly occurs during December–March; however, substantial influenza activity can be observed in November and activity can last as late as May. During the 2014–15 influenza season, activity increased in November and peaked in December; however during the current 2015–16 season, activity remains low. During October 4–November 28, 2015, influenza A (H3N2) viruses were identified most frequently in the United States, but pH1N1 and influenza B viruses also were reported.
Antigenic and genetic characterization of influenza-positive respiratory specimens submitted to CDC indicate that the majority of influenza virus isolates recently examined in the United States are similar to the 2015–16 influenza vaccine reference viruses. Although antigenic and genetic characterization of circulating influenza viruses can indicate whether antigenically different (i.e., "drifted") viruses have emerged, vaccine effectiveness studies are needed to determine how much protection has been provided to the community by vaccination. Last season, laboratory data indicated that most influenza A (H3N2) viruses had drifted from the 2014–15 influenza A (H3N2) vaccine reference virus. During that season, reduced vaccine effectiveness against the predominant influenza A (H3N2) viruses was noted (3). During other seasons, however, antigenic differences between circulating and reference vaccine viruses that suggested reduced vaccine effectiveness were not shown to have resulted in reduced protection in community studies undertaken during the season (3–5). Predicting which influenza viruses will predominate during a season is challenging. Although no significant drift has been identified in influenza viruses circulating recently, it is possible that drift may still occur.
Vaccination remains the most effective method of preventing influenza and its complications. Even during seasons when vaccine effectiveness is reduced, substantial public health impact can still be observed (6). CDC previously developed a model to estimate the illnesses and hospitalizations averted by influenza vaccination in the United States. During 2010–2014, annual vaccination prevented an estimated 1.7–7.8 million cases and 34,000–114,000 hospitalizations per season, or 9.4%–22.3% of hospitalizations associated with influenza (6). For the 2014–15 influenza season, updated estimates of vaccination coverage, vaccine effectiveness, and rates of influenza were used in the same model to estimate that influenza vaccination resulted in an estimated 1.9 million (95% confidence interval [CI] = 707,000–4.4 million) fewer illnesses, 966,000 (CI = 344,000–2.2 million) fewer medically attended illnesses, and 67,000 (CI = 15,000–208,000) fewer hospitalizations associated with influenza (6).
As of December 4, 2015, vaccine manufacturers have reported that approximately 140 million doses of influenza vaccine have been distributed. Health care providers should offer vaccine to all unvaccinated persons aged ≥6 months now and throughout the influenza season as long as influenza viruses are circulating. Vaccination coverage typically declines markedly after November, prompting CDC to annually observe a National Influenza Vaccination Week (December 6–12 this year) to promote influenza vaccination beyond November. Although the timing of influenza activity can vary, little influenza activity has occurred to date this season; thus, vaccination at this time should still offer substantial public health benefit. Past and current vaccine coverage estimates highlight low influenza vaccination coverage in the United States, despite a universal vaccination recommendation that has been in place since 2010. For the 2015–16 season, the Advisory Committee on Immunization Practices (ACIP) recommends that healthy children aged 2 years through 8 years who have no vaccine contraindications or precautions receive either live attenuated influenza vaccine (LAIV) or inactivated influenza vaccine (IIV), with no preference expressed for either vaccine when one is otherwise appropriate and available (5). For the 2015–16 season, ACIP recommends that children aged 6 months through 8 years who have previously received ≥2 total doses of trivalent or quadrivalent influenza vaccine at any time before July 1, 2015, require only 1 dose of 2015–16 influenza vaccine (5). The 2 previous doses do not need to have been given during the same or consecutive seasons (5). Children in this age group who are being vaccinated for the first time or who have not previously received a total of ≥2 doses before July 1, 2015, require 2 doses of 2015–16 influenza vaccine, administered ≥4 weeks apart (7).
Although influenza vaccination is the first and best way to prevent influenza, antiviral medications continue to be an important adjunct to vaccination for reducing the health impact of influenza. Treatment is most effective when given early during illness, and providers should not delay treatment until test results become available or rely on insensitive assays such as rapid antigen detection influenza diagnostic tests to determine treatment decisions (8). Treatment with influenza antiviral medications as early as possible is recommended for patients with confirmed or suspected influenza (either seasonal influenza or novel influenza virus infection) who have severe, complicated, or progressive illness; who require hospitalization; or who are at high risk for serious influenza-related complications*** (8). Antiviral treatment should not be withheld from severely ill patients or those at high risk with suspected influenza infection pending confirmatory influenza test results or based on illness onset††† (8).
Influenza surveillance reports for the United States are posted online weekly and are available at http://www.cdc.gov/flu/weekly. Additional information regarding influenza viruses, influenza surveillance, influenza vaccine, influenza antiviral medications, and novel influenza A virus infections in humans is available at http://www.cdc.gov/flu.
Acknowledgments
State, county, city, and territorial health departments and public health laboratories; U.S. World Health Organization collaborating laboratories; National Respiratory and Enteric Virus Surveillance System laboratories; U.S. Outpatient Influenza-Like Illness Surveillance Network sites; National Center for Health Statistics, CDC; 122 Cities Mortality Reporting System; World Health Organization FluNet; Angie Foust, Wendy Sessions, Elisabeth Blanchard, Priya Budhathoki, Thomas Rowe, Lizheng Guo, Ewelina Lyszkowicz, Shoshona Le, Malania Wilson, Juliana DaSilva, Alma Trujillo, Michael Hillman, Thomas Stark, Samuel Shepard, Sujatha Seenu, Ha Nguyen, Vasiliy Mishin, Margaret Okomo-Adhiambo, Michelle Adamczyk, Juan De la Cruz, Influenza Division, National Center for Immunization and Respiratory Diseases, CDC.
1Influenza Division, National Center for Immunization and Respiratory Diseases, CDC.
Corresponding author: Sophie Smith, ssmith11@cdc.gov, 404-639-3747.
References
- Schild GC, Oxford JS, de Jong JC, Webster RG. Evidence for host-cell selection of influenza virus antigenic variants. Nature 1983;303:706–9.
- Katz JM, Wang M, Webster RG. Direct sequencing of the HA gene of influenza (H3N2) virus in original clinical samples reveals sequence identity with mammalian cell-grown virus. J Virol 1990;64:1808–11.
- Flannery B, Clippard J, Zimmerman RK, et al. Early estimates of seasonal influenza vaccine effectiveness—United States, January 2015. MMWR Morb Mortal Wkly Rep 2015;64:10–5.
- Ohmit SE, Victor JC, Rotthoff JR, et al. Prevention of antigenically drifted influenza by inactivated and live attenuated vaccines. N Engl J Med 2006;355:2513–22.
- Grohskopf LA, Sokolow LZ, Olsen SJ, Bresee JS, Broder KR, Karron RA. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States, 2015–16 influenza season. MMWR Morb Mortal Wkly Rep 2015;64:818–25.
- CDC. Estimated influenza illnesses and hospitalizations averted by vaccination—United States, 2015–16 influenza season. Atlanta, GA: US Department of Health and Human Services, CDC. Available at http://www.cdc.gov/flu/about/disease/2014-15.htm.
- Neuzil KM, Jackson LA, Nelson J, et al. Immunogenicity and reactogenicity of 1 versus 2 doses of trivalent inactivated influenza vaccine in vaccine-naive 5–8-year-old children. J Infect Dis 2006;194:1032–9.
- Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM. Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(No. RR-1).
* CDC collects five categories of surveillance data from nine data sources: 1) viral surveillance (World Health Organization collaborating laboratories, the National Respiratory and Enteric Virus Surveillance System, and novel influenza A virus case reporting); 2) outpatient illness surveillance (U.S. Outpatient Influenza-Like Illness Surveillance Network); 3) mortality (the National Center for Health Statistics Mortality Surveillance System, 122 Cities Mortality Reporting System, and influenza-associated pediatric mortality reports); 4) hospitalizations (Influenza Hospitalization Surveillance Network [FluSurv-NET], which includes the Emerging Infections Program and surveillance in three additional states); and 5) summary of the geographic spread of influenza (state and territorial epidemiologist reports). Additional information available at http://www.cdc.gov/flu/weekly/fluactivitysurv.htm.
† Data reported as of December 4, 2015.
§ Region 1: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont. Region 2: New Jersey, New York, Puerto Rico, and the U.S. Virgin Islands. Region 3: Delaware, District of Columbia, Maryland, Pennsylvania, Virginia, and West Virginia. Region 4: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee. Region 5: Illinois, Indiana, Michigan, Minnesota, Ohio, and Wisconsin. Region 6: Arkansas, Louisiana, New Mexico, Oklahoma, and Texas. Region 7: Iowa, Kansas, Missouri, and Nebraska. Region 8: Colorado, Montana, North Dakota, South Dakota, Utah, and Wyoming. Region 9: Arizona, California, Hawaii, Nevada, American Samoa, Commonwealth of the Northern Mariana Islands, Federated States of Micronesia, Guam, Marshall Islands, and Republic of Palau. Region 10: Alaska, Idaho, Oregon, and Washington.
¶ Defined as a temperature of ≥100°F (≥37.8°C), oral or equivalent, and cough or sore throat, without a known cause other than influenza.
** The national and regional baselines are the mean percentage of visits for ILI during noninfluenza weeks for the previous three seasons plus two standard deviations. A noninfluenza week is defined as periods of ≥2 consecutive weeks in which each week accounted for <2% of the season's total number of specimens that tested positive for influenza. National and regional percentages of patient visits for ILI are weighted on the basis of state population. Use of the national baseline for regional data is not appropriate.
†† Activity levels are based on the percentage of outpatient visits in a jurisdiction attributed to ILI and are compared with the average percentage of ILI visits that occur during weeks with little or no influenza virus circulation. Activity levels range from minimal, corresponding to ILI activity from outpatient clinics at or below the average, to high, corresponding to ILI activity from outpatient clinics much higher than the average. Because the clinical definition of ILI is very nonspecific, not all ILI is caused by influenza; however, when combined with laboratory data, the information on ILI activity provides a clearer picture of influenza activity in the United States.
§§ Levels of activity are 1) no activity; 2) sporadic: isolated laboratory-confirmed influenza case(s) or a laboratory-confirmed outbreak in one institution, with no increase in activity; 3) local: increased ILI, or at least two institutional outbreaks (ILI or laboratory-confirmed influenza) in one region of the state, with recent laboratory evidence of influenza in that region and virus activity no greater than sporadic in other regions; 4) regional: increased ILI activity or institutional outbreaks (ILI or laboratory-confirmed influenza) in at least two but less than half of the regions in the state with recent laboratory evidence of influenza in those regions; and 5) widespread: increased ILI activity or institutional outbreaks (ILI or laboratory-confirmed influenza) in at least half the regions in the state, with recent laboratory evidence of influenza in the state.
¶¶ The seasonal baseline proportion of P&I deaths is projected using a robust regression procedure, in which a periodic regression model is applied to the observed percentage of deaths from P&I that were reported by the National Center for Health Statistics Mortality Surveillance System and the 122 Cities Mortality Reporting System during the preceding 5 years. The epidemic threshold is set at 1.645 standard deviations above the seasonal baseline. Users of the data should not expect the NCHS mortality surveillance data and the 122 Cities Mortality Reporting System to produce the same percentages and the percent P&I deaths from each system should be compared to the corresponding system specific baselines and thresholds.
*** Persons at higher risk include 1) children aged <2 years; 2) adults aged ≥65 years; 3) persons with chronic pulmonary conditions (including asthma); cardiovascular disease (except hypertension alone); renal, hepatic, hematologic (including sickle cell) disease; metabolic disorders (including diabetes mellitus); or neurologic and neurodevelopmental conditions (including disorders of the brain, spinal cord, peripheral nerves, and muscles, such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability [mental retardation], moderate to severe developmental delay, muscular dystrophy, or spinal cord injury); 4) persons with immunosuppression, including that caused by medications or by human immunodeficiency virus infection; 5) women who are pregnant or postpartum (within 2 weeks after delivery); 6) persons aged ≤18 years who are receiving long-term aspirin therapy; 7) American Indians/Alaska Natives; 8) persons who are morbidly obese (i.e., body mass index ≥40); and 9) residents of nursing homes and other chronic care facilities.
††† Additional information on antiviral use and treatment of influenza is available at: http://www.cdc.gov/flu/antivirals.
Summary
What is already known on this topic?
CDC collects, compiles, and analyzes data on influenza activity year-round in the United States. The influenza season generally begins in the fall and continues through the winter and spring months; however, the timing and severity of circulating influenza viruses can vary by geographic location and season.
What is added by this report?
During October 4–November 28, 2015, influenza activity overall in the United States remained low. Influenza A (H3N2) viruses were the most frequently identified viruses. All viruses characterized thus far this season have been similar to their respective components of the 2015–16 Northern Hemisphere trivalent and quadrivalent influenza vaccines. All influenza viruses tested to date have been sensitive to the antiviral drugs oseltamivir, zanamivir, and peramivir.
What are the implications for public health practice?
Vaccination remains the most effective method to prevent influenza and its complications. Health care providers should offer vaccine to all unvaccinated persons aged ≥6 months now and throughout the influenza season. As an adjunct to vaccine, treatment with influenza antiviral medications can lessen severity and duration of illness and can reduce severe outcomes of influenza. Antiviral medications work best when administered early in the course of influenza-like illness.
FIGURE 1. Number* and percentage of respiratory specimens testing positive for influenza reported by clinical laboratories, by influenza virus type and surveillance week — United States, September 28, 2014–November 28, 2015
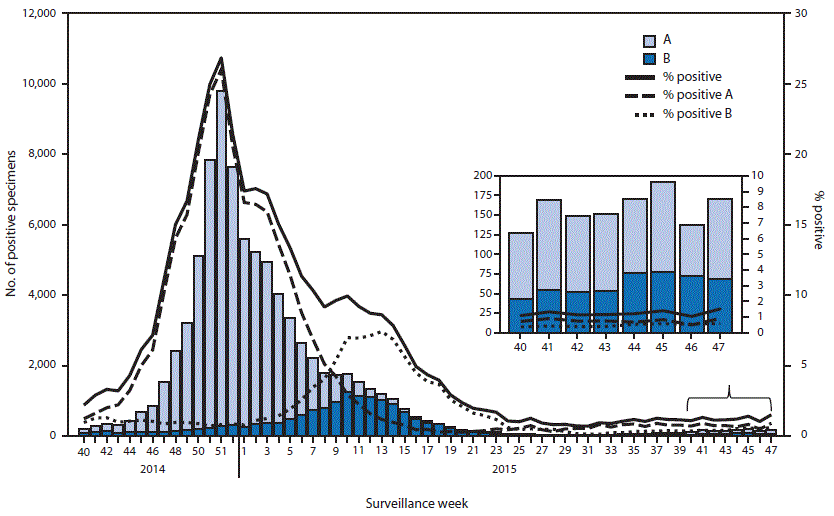
* 1,268 of 102,675 tested were positive during October 4–November 28, 2015.
Alternate Text: The figure above is a combination bar and line chart showing the number and percentage of respiratory specimens testing positive for influenza reported by clinical laboratories, by influenza virus type and surveillance week, in the United States during September 28, 2014-November 28, 2015.
FIGURE 2. Number* of respiratory specimens testing positive for influenza reported by public health laboratories, by influenza virus type, subtype and surveillance week — United States, September 28, 2014–November 28, 2015
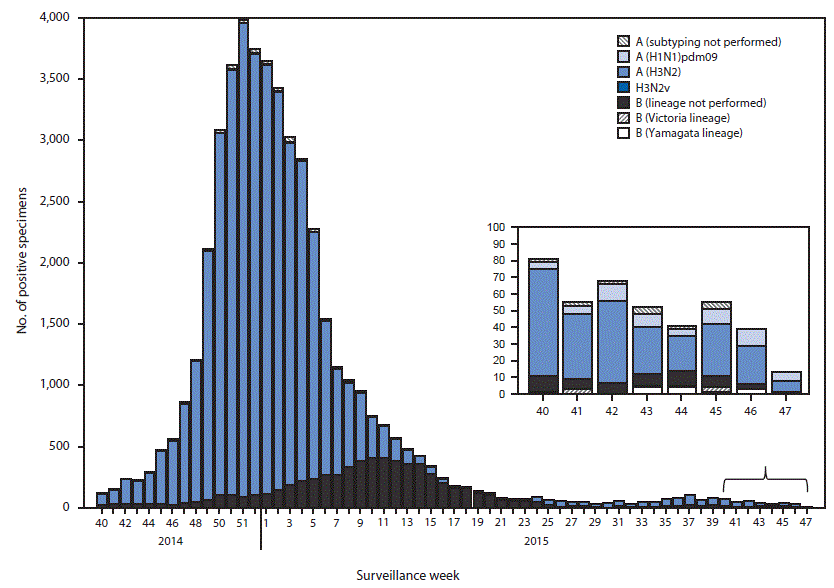
* 404 of 8,488 tested were positive during October 4–November 28, 2015.
Alternate Text: The figure above is a bar chart showing the number of respiratory specimens testing positive for influenza reported by public health laboratories, by influenza virus type, subtype and surveillance week, in the United States during September 28, 2014-November 28, 2015.
FIGURE 3. Percentage of all outpatient visits for influenza-like illness (ILI)* reported to CDC, by surveillance week — Outpatient Influenza-like Illness Surveillance Network, United States, October 4–November 28, 2015, and selected previous influenza seasons
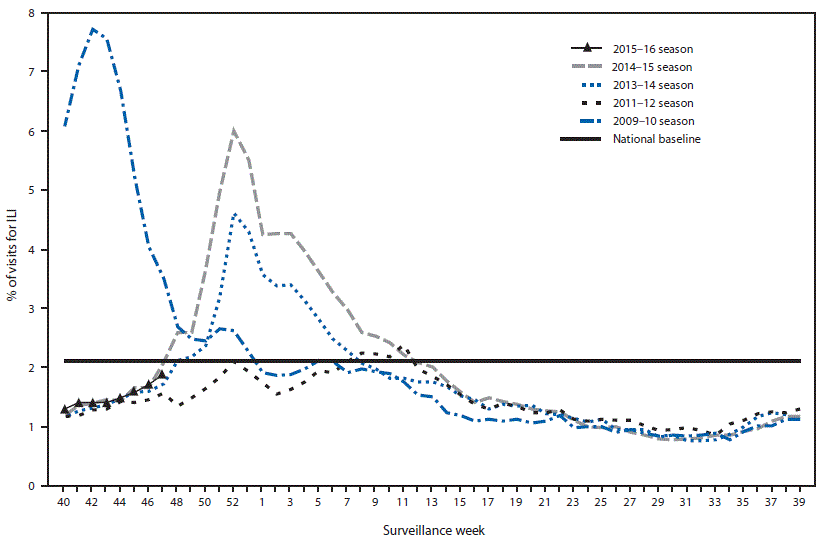
* Defined as a fever (≥100°F [≥37.8°C]), oral or equivalent, and cough or sore throat, without a known cause other than influenza.
Alternate Text: The figure above is a line chart showing the percentage of all outpatient visits for influenza-like illness reported to CDC, by surveillance week, in the United States during October 4-November 28, 2015, and selected previous influenza seasons.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


