Notes from the Field: Outbreak of Escherichia coli O157:H7 Infections Associated with Dairy Education Event Attendance — Whatcom County, Washington, 2015
, PhD1,2; , MPH2; , PhD1,3; 4; 4; , MPH5; , MPH2; , PhD2; , DVM2
On April 27, 2015, the Whatcom County Health Department (WCHD) in Bellingham, Washington, was notified by a local laboratory regarding three children with presumptive Escherichia coli O157 infection. WCHD interviewed the parents, who indicated that all three children had attended a dairy education event held in a barn April 20–24, 2015, during a school field trip. WCHD, the Washington State Department of Health, and CDC investigated to determine the magnitude of the outbreak, identify risk factors and potential environmental sources of infection, and develop recommendations. A total of 60 cases (25 confirmed and 35 probable) were identified, and 11 patients were hospitalized.
Shiga-toxin producing E. coli infection is a notifiable condition in Washington. WCHD issued a health alert and notified local laboratories, school nurses, parents, and event organizers of the outbreak. WCHD and the state health department interviewed patients with confirmed E. coli infection and others who reported diarrheal illness about their attendance at the dairy education event. PulseNet, the national molecular subtyping laboratory network for foodborne disease surveillance, used pulsed-field gel electrophoresis (PFGE) to identify outbreak strains. A confirmed case of E. coli O157:H7 infection was defined as laboratory confirmation of infection with the outbreak strains or physician-diagnosed hemolytic uremic syndrome in a person with diarrheal illness onset during April 20–June 1, who had attended the dairy event or had close contact with someone who had attended the event. A probable case was defined as diarrheal illness in a person with onset during April 20–June 1, who had attended the event or had close contact with someone who attended the event. Confirmed and probable cases were classified as primary (patient attended the event) or secondary (patient was a contact of someone who attended the event). Environmental testing of the barn was conducted; bacterial isolates were compared with patient isolates using PFGE.
During April 20–June 1, 2015, 60 cases (25 confirmed and 35 probable) were identified (Figure). Eleven (18%) patients were hospitalized, and six (10%) developed hemolytic uremic syndrome. No deaths occurred. Forty primary cases were identified in 35 first-graders, three high school students, one parent, and one teacher who attended the event. Twenty secondary cases were identified in 14 siblings, four caretakers, and two cousins of attendees.
Food was served inside the barn to adolescents who set up and broke down the event on April 20 and April 24. During April 21–23 approximately 1,000 first-grade students attended the event, which included various activities related to farming. Crude attack rates were higher among those who assisted with setup on April 20 or breakdown on April 24 (three of 14 high school students; 21%) and among attendees on April 21 (22 of 254 students; 9%), than among attendees on April 22 (six of 377 students; 2%) and April 23 (seven of 436 students; 2%).
Animals, including cattle, had been exhibited in the barn during previous events. Before the dairy education event, tractors, scrapers, and leaf blowers were used to move manure to a bunker at the north end of the barn. Environmental samples collected in this area yielded E. coli O157:H7 PFGE patterns indistinguishable from the outbreak strains.
This investigation highlighted the importance of implementing infection prevention measures at events held in venues with animals or where animals had been present. Students attending the setup and breakdown might have had higher rates of illness because they consumed food in the barn and might not have washed their hands before eating. Facility cleaning procedures and location of the manure bunker (inside the barn) might have contributed to an increased risk for infection among the attendees.
Although it might not be possible to completely disinfect barns and areas where animals have been kept, standard procedures for cleaning, disinfection, and facility design should be adopted to minimize the risk for exposure to pathogens (1). These environments should be considered contaminated and should not be located in areas where food and beverages are served. Hands should always be washed with soap and clean running water, and dried with clean towels immediately upon exiting areas containing animals or where animals have been kept previously, after removing soiled clothing or shoes, and before eating or drinking (2). Event organizers can refer to published recommendations for preventing disease associated with animals in public settings (1).
1Epidemic Intelligence Service, CDC; 2Division of Foodborne, Waterborne, and Environmental Diseases, National Center for Emerging and Zoonotic Infectious Diseases, CDC; 3Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC; 4Whatcom County Health Department, Bellingham, Washington; 5Washington State Department of Health.
Corresponding author: Kathryn Curran, ydh9@cdc.gov, 404-639-4638.
References
- National Association of State Public Health Veterinarians. Compendium of measures to prevent disease associated with animals in public settings. J Am Vet Med Assoc 2013;243:1270–88.
- CDC. Show me the science—how to wash your hands. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. Available at http://www.cdc.gov/handwashing/show-me-the-science-handwashing.html.
FIGURE. Number of persons (N = 54) infected with the outbreak strains of Escherichia coli O157:H7, by date of illness onset and dairy education event attendance — Whatcom County, Washington, April 20–June 1, 2015*
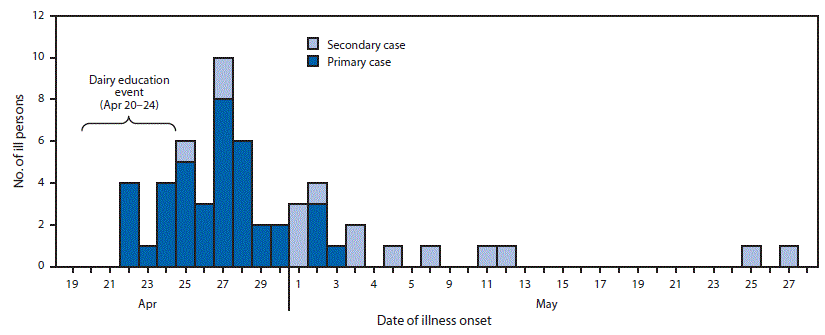
* Six additional patients (one primary, five secondary) were ill during April 20–June 1, but exact illness onset dates were unknown.
Alternate Text: The figure above is an epidemiologic curve showing the number of persons (N = 54) infected with the outbreak strains of Escherichia coli O157:H7, by date of illness onset and dairy education event attendance in Whatcom County, Washington, during April 20-June 1, 2015.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


