FIGURE. Total number of reported measles cases, and coverage with 1 dose of measles-containing vaccine (MCV1) among children aged 13–24 months, by subregion* — European Region of the World Health Organization (WHO), 2004–2011
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Increased Transmission and Outbreaks of Measles — European Region, 2011
During 2003–2009, substantial progress was made toward the previous goal of measles elimination in the World Health Organization (WHO) European Region (EUR) by 2010 (1,2). However, since late 2009, measles virus transmission has increased, and outbreaks have become widespread. In 2011, measles outbreaks have been reported in 36 of 53 EUR member states; a total of 26,074 measles cases had been reported regionwide as of October 26. France reported the largest number of cases (approximately 14,000), predominantly among older children and young adults who had not been vaccinated or whose vaccination history was unknown. Overall, the primary reason for the increased transmission and outbreaks of measles in EUR is failure to vaccinate susceptible populations. Eliminating measles by 2015, a new measles elimination target date set in September 2010 by the 60th Regional Committee for Europe, will require 1) increasing demand for and delivery of vaccination to achieve and sustain ≥95% coverage with 2 doses of measles-containing vaccine (MCV) across a wide age range, 2) implementing effective outbreak control measures, and 3) further strengthening surveillance to identify cases and outbreaks promptly, and in the future, to validate elimination (3).
Measles is a notifiable disease in all 53 EUR member states,* and all states recommend 2 doses of MCV. Clinically diagnosed measles cases are reported annually from member states to the WHO Regional Office for Europe (WHO/Europe), using the WHO and United Nations Children's Fund (UNICEF) Joint Reporting Form.† Countries also are requested to report monthly individual case information (e.g., laboratory confirmation status and demographic, clinical, and vaccination data) and to report outbreaks as they occur. MCV coverage is reported to WHO/Europe annually using the Joint Reporting Form.
After 3 years of historically low measles incidence (1), the number of reported measles cases increased sharply in late 2009. In 2010, 30,639 measles cases were reported, the most since 2006. As of October 26, a total of 26,074 cases had been reported in EUR in 2011. The western European subregion (WE) reported 21,724 (83.3%) cases, the central and eastern European subregion (CEE) 3,570 (13.7%) cases, and the newly independent states (NIS) of the former Soviet Union 780 (3.0%) cases. Since 2008, WE has accounted for the largest proportion of measles cases in the region, with the exception of 2010, when most cases occurred in CEE because of a large outbreak in Bulgaria (24,401 reported cases during 2009–2011) (Figure).
As of October 26, 2011, a total of 12,882 (49.4%) cases had occurred among persons aged ≥15 years, 6,527 (25.0%) among children aged <5 years, and 6,423 (24.7%) among children aged 5–14 years (Table 1). The median age of patients was 15 years. Overall, 11,763 (45.1%) patients were unvaccinated, and vaccination histories of 11,825 (45.4%) were unknown (Table 1). A total of 7,288 (28.0%) measles patients were hospitalized, including 4,293 (58.9%) in WE, 2,609 (35.8%) in CEE, and 386 (5.3%) in NIS. The proportion of hospitalized patients was higher in CEE and NIS (73.1% and 49.5%, respectively), where hospitalization of measles patients is a long-standing routine practice, than in WE (19.8%), where only patients with severe cases usually are hospitalized. Nine measles-associated deaths were reported, including six in France, one in Germany, one in Kyrgyzstan, and one in Romania. Seven deaths occurred among persons aged >10 years. Four decedents were unvaccinated, and the vaccination histories of the remaining five, all adults, were unknown.
A total of 115 measles outbreaks, accounting for 21,177 (81.2%) cases, were reported in 36 countries from January 1 to October 26, 2011. The outbreak in France is the largest ongoing outbreak in the region, with 14,025 cases reported as of October 26. Cases have been reported nationwide, including 2,593 (18.5%) cases in the province of Rhône-Alpes; 2,167 (15.5%) in Provence-Alpes-Côte d'Azur; 1,191 (8.5%) in Languedoc-Roussillon; 1,158 (8.3%) in Limousin; and 1,080 (7.7%) in Île-de-France. In Spain, cases have been reported in 16 of the country's 17 autonomous communities (regional governments) and in the two autonomous cities, including 1,381 (50.3%) cases in Andalucia; 439 (16.0%) in Catalonia; and 329 (12.0%) in Madrid. In Romania, cases have been reported in 34 of 42 provinces, with six northwestern provinces (Arad, Bihor, Cluj, Maramures, Salaj, and Satu Mare) reporting 1,860 (86.3%) cases.
Overall, transmission settings in the region varied and included communities as a whole, groups with religious or philosophical objections to vaccination, underserved populations with limited health-care access, health-care facilities, and schools. Within specific countries, settings also included vacation camps (France) and rural populations (Romania); settings were not reported for Uzbekistan.
Measles virus genotypes detected by molecular sequencing from specimens from patients in EUR in 2011 included D4, B3, G3, D8, D9, and H1. Genotype D4, detected in 24 countries during 2011, was the predominant genotype. This genotype has been associated with outbreaks in EUR member states since 2008 (4,5), including outbreaks during 2011 in France, Spain, the former Yugoslav Republic of Macedonia, Romania, and Uzbekistan. Genotype G3 also was detected in France, and genotype B3 also was detected in Spain.
In response to measles outbreaks, a wide range of control measures have been implemented, including 1) activities to strengthen surveillance for timely identification and monitoring of cases and outbreaks, 2) social mobilization and advocacy for immunization among the general population and among health-care providers, 3) modifying immunization schedules and vaccination policies, and 4) implementing supplementary immunization activities (SIAs) of various scales, from offering free vaccination to persons not covered by routine vaccination programs to nationwide or subnational campaigns (Table 2).
During 2004–2010, overall coverage with 1 dose of MCV (MCV1) for the entire region was 92%–94%; WE had lower MCV1 coverage (90%–92%) than CEE (88%–97%) and NIS (91%–96%) (Figure). MCV1 coverage in France during 2004–2010 was 87%–90%.
Reported by
Rebecca Martin, PhD, Dragan Jankovic, MD, Ajay Goel, Mick Mulders, PhD, World Health Organization Regional Office for Europe, Copenhagen, Denmark. Alya Dabbagh, PhD, World Health Organization, Geneva, Switzerland. Nino Khetsuriani, MD, Ikechukwu Ogbuanu, MD, Global Immunization Div, Center for Global Health, CDC. Corresponding contributor: Nino Khetsuriani, nkhetsuriani@cdc.gov, 404-639-4671.
Editorial Note
The increase in measles virus transmission in EUR poses a serious challenge to achieving the regional measles elimination goal by 2015. Despite overall high coverage with MCV in the region, MCV1 coverage remains below the target of 95%, particularly in WE. These data confirm the existence of susceptible groups, which can include older children and adults, and vaccination coverage <95% can support ongoing virus transmission, leading to large-scale outbreaks (1,6). Additional measures targeting susceptible populations to achieve ≥95% coverage with 2 doses of MCV are needed to increase immunity levels in the EUR population.
Principal factors contributing to decreased demand for measles vaccination in EUR include lack of knowledge of the seriousness of the disease, resulting in a reluctance to be vaccinated; skepticism about the benefits of vaccination; fear of adverse effects from being vaccinated; and limited health-care access for some underserved populations (6). Religious or philosophical objections to vaccination are serious barriers to increasing population immunity in certain communities in EUR, particularly in WE (6).
The accumulation of susceptible persons among older children and young adults because of low coverage in the past and the decline in natural exposure to measles virus because of successful vaccination programs has resulted in an increase in the median age of measles patients in EUR (1,7). This change in measles epidemiology requires strategies tailored to older age groups and strategies to prevent transmission among infants too young to be vaccinated. To prevent further spread of the virus, effective surveillance, outbreak prevention, and control measures need to be continued, especially before mass gatherings (e.g., the European Football Championship in Poland and Ukraine in 2012). Implementation of the revised Guidelines for Measles and Rubella Surveillance in the European Region (8), beginning in 2012, will help to further strengthen surveillance capacity in the member states.
Measles in EUR is causing preventable death, illness, and financial costs and has global implications. The nine deaths and thousands of measles-associated hospitalizations in EUR during 2011 are reminders that measles is a serious disease that can lead to death in all age groups, even in countries with high-quality health care and minimal incidence of malnutrition. The substantial financial and human costs of responding to these outbreaks impose an additional burden on already limited resources. In addition, EUR has become a source of virus introduction into other areas, such as the measles-free WHO Region of the Americas. Importations from EUR have accounted for most measles importations in the United States since 2008, with 20 importations in 2011 alone, including 11–13 cases from France (9). During 2011, approximately 1,000 measles cases were reported in the Region of the Americas, necessitating extensive and costly public health responses (10).
To increase demand for measles vaccination in EUR, innovative strategies and tools are needed to effectively communicate the seriousness of measles and the benefits of vaccination to the general public and to health-care professionals. Reaching the EUR measles elimination target by 2015 is achievable. However, reaching the target will require ongoing, high-level political commitment to routine childhood immunization throughout EUR. Additional measures also are warranted, including SIAs to reduce susceptibility among older cohorts and strategies to ensure access to health care among underserved populations.
Acknowledgments
Immunization program staff members in all 53 World Health Organization European Region member states.
References
- Martin R, Wassilak S, Emiroglu N, et al. What will it take to achieve measles elimination in the World Health Organization European Region: progress from 2003–2009 and essential accelerated actions. J Infect Dis 2011;204(Suppl 1):S325–34.
- World Health Organization. Health 21: the health for all policy framework for the WHO European Region. European health for all series, no. 6. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1999. Available at http://www.euro.who.int/__data/assets/pdf_file/0010/98398/wa540ga199heeng.pdf. Accessed November 23, 2011.
- World Health Organization. Renewed commitment to elimination of measles and rubella and prevention of congenital rubella syndrome by 2015 and sustained support for polio-free status in the WHO European Region. Resolution 12 (EUR/RC60/R12). Copenhagen, Denmark: World Health Organization Regional Committee for Europe; 2010. Available at http://www.euro.who.int/__data/assets/pdf_file/0016/122236/RC60_eRes12.pdf. Accessed November 23, 2011.
- Mankertz A, Mulders MN, Shulga S, et al. Molecular genotyping and epidemiology of measles virus transmission in the World Health Organization European Region, 2007–2009. J Infect Dis 2011;204(Suppl 1):S335–42.
- Mankertz A, Mihneva Z, Gold H, et al. Spread of measles virus D4-Hamburg, Europe, 2008–2011. Emerg Infect Dis 2011;17:1396–401.
- Muscat M. Who gets measles in Europe? J Infect Dis 2011;204(Suppl 1):S353–65.
- Doshi S, Khetsuriani N, Zakhashvili K, Baidoshvili L, Imnadze P, Uzicanin A. Ongoing measles and rubella transmission in Georgia, 2004–05: implications for the national and regional elimination efforts. Int J Epidemiol 2009;38:182–91.
- World Health Organization. Surveillance guidelines for measles, rubella and congenital rubella syndrome in the WHO European Region. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2009. Available at http://www.euro.who.int/__data/assets/pdf_file/0018/79020/E93035.pdf. Accessed November 23, 2011.
- CDC. Measles—United States, January–May 20, 2011. MMWR 2011;60:666–8.
- Panamerican Health Organization. Measles and rubella surveillance in the Americas. Measles/Rubella Wkly Bull 2011;17. Available at http://new.paho.org/hq/dmdocuments/2011/sme1717.pdf. Accessed November 23, 2011.
* In 2011, the European Region of WHO included 53 member states, grouped for the purpose of this report into the western European subregion (Andorra, Austria, Belgium, Cyprus, Denmark, Finland, France, Germany, Greece, Iceland, Ireland, Israel, Italy, Luxembourg, Malta, Monaco, Netherlands, Norway, Portugal, San Marino, Spain, Sweden, Switzerland, and the United Kingdom), the central and eastern European subregion (Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Estonia, Hungary, Latvia, Lithuania, Montenegro, Poland, Romania, Serbia, Slovakia, Slovenia, the former Yugoslav Republic of Macedonia, and Turkey), and the newly independent states of the former Soviet Union subregion (Armenia, Azerbaijan, Belarus, Georgia, Kazakhstan, Kyrgyzstan, Republic of Moldova, Russian Federation, Tajikistan, Turkmenistan, Ukraine, and Uzbekistan).
† Available at http://www.who.int/immunization_monitoring/routine/joint_reporting/en/index.html.
What is already known on this topic?
During 2003–2009, substantial progress toward the goal of measles elimination in the World Health Organization (WHO) European Region by 2010 was achieved. However, after 3 years of historic low measles incidence, the number of reported measles cases increased sharply, beginning in late 2009.
What is added by this report?
As of October 26, a total of 26,074 measles cases with onset in 2011 have been reported regionwide, with outbreaks in 36 of 53 member states and nine measles-associated deaths. France reported the largest number of cases (approximately 14,000). Approximately half (49.4%) of patients in the region were aged ≥15 years, and the majority were unvaccinated (45.1%) or had unknown vaccination status (45.4%).
What are the implications for public health practice?
Failure to vaccinate, leading to the existence of susceptible populations across a wide age range, particularly in the western European subregion, has contributed to increased transmission and outbreaks of measles in the European Region. Eliminating measles by the WHO regional target of 2015 will require 1) increasing and sustaining ≥95% coverage with 2 doses of measles-containing vaccine across a wide age range, 2) implementing effective outbreak control measures, and 3) further strengthening surveillance to identify cases and outbreaks quickly, and to validate measles elimination.
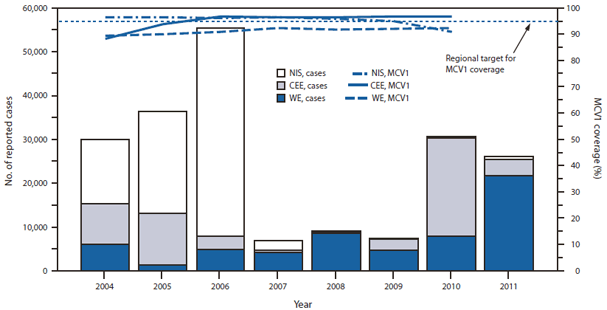
Sources: Annual WHO/UNICEF Joint Reporting Forms and, for 2011, monthly surveillance reports submitted to WHO as of October 26, 2011; MCV1 coverage data for 2011 is not yet available.
* Subregions: WE = western European, CEE = central and eastern European, NIS = newly independent states of the former Soviet Union.
Alternate Text: The figure above shows the total number of reported measles cases and coverage with 1 dose of measles-containing vaccine (MCV1) among children aged 13-24 months, by subregion in the European Region of the World Health Organization, during 2004-2011. Since 2008, the western European subregion has accounted for the largest proportion of measles cases in the region, with the exception of 2010, when most cases occurred in the central and eastern European subregion because of a large outbreak in Bulgaria (24,401 reported cases during 2009-2011). During 2004-2010, overall MCV1 coverage for the entire European Region was 92%-94%.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


