Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
HIV Testing Among Men Who Have Sex with Men --- 21 Cities, United States, 2008
Although men who have sex with men (MSM) comprise an estimated 2% of the overall U.S. population aged ≥13 years (1), 59% of persons with diagnoses of human immunodeficiency virus (HIV) infection in the United States in 2009 were MSM, including MSM who inject drugs (2). CDC recommends HIV testing at least annually for sexually active MSM to identify HIV infections and prevent ongoing transmission (3). Results of HIV testing conducted as part of the National HIV Behavioral Surveillance System (NHBS) in 21 cities indicated that 19% of MSM who were tested in 2008 were HIV-positive; of these, 44% were unaware that they were infected (4). To assess whether MSM were tested as recommended and whether more frequent testing might be indicated, CDC analyzed NHBS data for 2008. This report describes the results of that analysis, which indicated that, of 7,271 MSM interviewed and tested who did not report a previous positive HIV test, 61% had been tested for HIV infection during the past 12 months; among these, 7% had a new, positive HIV test result when tested as part of NHBS. Given the high prevalence of new HIV infection among MSM who had been tested during the past year, sexually active MSM might benefit from more frequent HIV testing (e.g., every 3 to 6 months).
NHBS is a behavioral surveillance system used to monitor HIV-related risk, testing, and prevention behaviors and HIV prevalence among populations at high risk for acquiring HIV (5). In 2008, NHBS staff members in 21 metropolitan statistical areas (MSAs) with high prevalence of acquired immunodeficiency syndrome (AIDS)* collected cross-sectional behavioral risk data and conducted HIV testing among MSM (4). MSM were sampled using venue-based sampling methods (6). NHBS staff members identified venues (e.g., bars, clubs, organizations, and street locations) and days and times when MSM frequented those venues (7). Venues and days/times were selected using a computerized random selection process each month for interviews and supplemented by up to three nonrandom events (e.g., Gay Pride events) per site per month. Staff members systematically approached men at each venue, intercepting potentially eligible men in the order in which they entered a designated "counting area" (6). Men eligible to be interviewed were aged ≥18 years, residents of the MSAs, and able to complete the interview in English or Spanish. After participants gave informed consent, trained interviewers used a handheld computer to administer a standardized, anonymous questionnaire about sex, drug use, and HIV testing behaviors. All respondents were offered anonymous HIV testing, which was performed by collecting blood or oral specimens for either rapid testing at venues or laboratory-based testing. A nonreactive rapid test was considered a definitive negative result; a reactive (preliminary positive) rapid test result was considered a definitive positive result only when confirmed by Western blot or immunofluorescence assay. Incentives were offered for participating in the interview and HIV test.
This analysis excluded MSM who reported a previous positive HIV test. CDC determined the proportion of MSM who received an HIV test during the past 12 months and, of these, the proportion with a positive NHBS test result, stratifying by demographic and risk characteristics. Those testing positive were considered to be unaware of their infection. CDC sexually transmitted disease (STD) treatment guidelines recommend that MSM who have multiple or anonymous partners, have sex in conjunction with illicit drug use, use methamphetamine, or whose sex partners participate in these activities be screened for STDs and HIV more frequently (every 3 to 6 months) than those without such risk factors (8). To reflect these guidelines, MSM with high-risk behaviors were defined as those reporting at least one of the following: more than one male sex partner during the past 12 months, methamphetamine use during the past 12 months, sex in conjunction with illicit drug use at most recent sex, or a most recent male sex partner who definitely or probably had concurrent sex partners. CDC determined the proportion of HIV-infected men among MSM who did and did not report high-risk behaviors.
A multivariable Poisson model was used to create unadjusted and adjusted prevalence ratios to determine factors associated with being HIV-infected (9). The adjusted model controlled for various factors: race/ethnicity, age, annual household income, education, health insurance status, time since most recent HIV test, unprotected anal sex, and high-risk behaviors.
Of 28,468 men approached, 12,325 were screened for participation at 626 venues. Of men screened, 11,074 (90%) were eligible for the survey. Men who were surveyed were excluded from analysis if they did not complete both the survey (n = 396 [4%]) and the HIV test (n = 1,535 [14%]), did not report sex with a man during the preceding 12 months (n = 1,744 [16%]), had an indeterminate HIV test result (n = 85 [0.8%]), or reported being HIV-positive (n = 1,214 [11%]). These reasons were not mutually exclusive. Of eligible men, 7,271 (66%) were included in this analysis.
Of men included in this report, 44% were white, 25% were Hispanic, and 23% were black. Mean age was 34 years (range: 18--85 years); 62% had less than a college education, 29% reported an annual household income <$20,000, and 34% had no health insurance (Table 1).
Among the 7,271 MSM, 680 (9%) were HIV-infected. Of these, 16% had never been tested for HIV, and 29% had been tested during the past 6 months (Figure).
Among the 7,271 MSM, 4,453 (61%) had tested for HIV infection during the past 12 months and did not receive a positive HIV test result. The proportion tested was higher among MSM in younger age groups and those with higher levels of education and income but did not vary by race/ethnicity (Table 1). Among 5,864 (81%) MSM with high-risk behaviors, 44% had been tested for HIV infection during the past 6 months.
Among the 4,453 MSM who had not received a diagnosis of HIV infection previously and were tested for HIV during the past 12 months, 7% (15% of blacks, 7% of Hispanics, and 3% of whites) were found to be HIV-infected when tested by NHBS (Table 2). Of 3,672 MSM with high-risk behaviors who were tested for HIV in the past 12 months and did not receive a positive HIV test result, 7% were HIV-infected when tested by NHBS, compared with 8% of those who did not report any high-risk behaviors. Prevalence of HIV infection among these two groups remained similar after adjusting for time since most recent HIV test. After adjusting for risk and testing behaviors, substantial and significant differences between black, Hispanic, and white MSM persisted (Table 2).
Reported by
Alexandra M. Oster, MD, Isa W. Miles, ScD, Binh C. Le, MD, Elizabeth A. DiNenno, PhD, Ryan E. Wiegand, MS, James D. Heffelfinger, MD, Richard Wolitski, PhD, Div of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC. Corresponding contributor: Alexandra M. Oster, CDC, aoster@cdc.gov, 404-639-6141.
Editorial Note
The findings from this analysis suggest that adherence to annual HIV testing recommendations for MSM is low and that even among MSM who reported being tested during the past 12 months, a substantial proportion were newly infected. Because persons often reduce their risk behaviors when they receive a diagnosis of HIV infection and persons who do not know they are infected are estimated to account for more than half of sexually transmitted HIV infections (10), increasing the frequency of HIV testing for MSM can reduce the time from HIV infection to diagnosis and reduce HIV transmission.
Current CDC guidelines identify MSM who should be tested more frequently according to their risk behaviors (8). However, among MSM in this analysis, those who had high-risk behaviors were not more likely to be newly infected than those without high-risk behaviors, suggesting that self-reported risk behaviors might not determine which MSM should be tested more frequently. The 7% prevalence of new HIV infection detected through NHBS among MSM who had been tested for HIV during the past year and the similar prevalence of new HIV infection among MSM with and without high-risk behaviors suggests that more frequent testing, perhaps as often as every 3 to 6 months, might be warranted among all sexually active MSM, regardless of their risk behaviors. In considering revising guidelines regarding frequency of testing among MSM, public health officials also should weigh other factors, including the acceptability and cost effectiveness of testing MSM more frequently and the sensitivity of tests in the early stages of infection.
That MSM with less education and income were less likely to have been tested suggests that efforts to expand access to and use of HIV testing among MSM should concentrate on these populations. Additionally, although recent HIV testing did not vary by race/ethnicity, the high proportion of HIV-infected persons among minority MSM, particularly black MSM, who had not previously received a diagnosis of HIV infection and were tested during the past year underscores that testing among these populations should be a priority for HIV testing programs.
The findings in this report are subject to at least three limitations. First, positive HIV status might have been underreported, and recent HIV testing might have been overreported during this interviewer-administered survey, thereby inflating estimates of the proportion of MSM in the sample with new HIV infections. Likewise, MSM might have underreported high-risk behaviors, resulting in some MSM being miscategorized as not having high-risk behaviors. This social-desirability bias also can influence response in HIV testing settings, which suggests that identifying persons for more frequent testing based on self-reported risk might not be effective because it might miss those at risk who underreport risk behaviors. Second, MSM with high-risk behaviors who were tested in the past 12 months might have been more likely to receive a positive HIV test result and be excluded from this analysis compared with MSM without high-risk behaviors, which might have resulted in an underestimation of HIV risk among those with high-risk behaviors. Finally, participants were recruited at venues, most of which were bars and clubs, in 21 cities with high AIDS prevalence and might not represent all MSM; data have not been weighted to account for the unequal selection probabilities of venues or frequency of venue attendance.
This analysis demonstrates that MSM remain a key population for expanded HIV testing efforts. Efforts to increase the proportion of HIV-infected MSM who are aware of their infection should include 1) enhanced outreach of HIV testing to sexually active MSM, particularly populations with higher HIV incidence, in clinical and nonclinical settings, and 2) reexamination of existing recommendations and consideration of HIV testing every 3 to 6 months for all sexually active MSM regardless of self-reported risk behaviors.
Acknowledgments
National HIV Behavioral Surveillance System staff members, including Jennifer Taussig, Robert Gern, Tamika Hoyte, Laura Salazar, Atlanta, Georgia; Colin Flynn, Frangiscos Sifakis, Baltimore, Maryland; Deborah Isenberg, Maura Driscoll, Elizabeth Hurwitz, Boston, Massachusetts; Nik Prachand, Nanette Benbow, Chicago, Illinois; Sharon Melville, Richard Yeager, Aaron Sayegh, Jim Dyer, Alicia Novoa, Dallas, Texas; Mark Thrun, Alia Al-Tayyib, Ralph Wilmoth, Denver, Colorado; Emily Higgins, Vivian Griffin, Eve Mokotoff, Detroit, Michigan; Marcia Wolverton, Jan Risser, Hafeez Rehman, Houston, Texas; Trista Bingham, Ekow Sey, Los Angeles, California; Marlene LaLota, Lisa Metsch, Dano Beck, David Forrest, Gabriel Cardenas, Miami, Florida; Chris Nemeth, Carol-Ann Watson, Nassau-Suffolk, New York; William T. Robinson, DeAnn Gruber, New Orleans, Louisiana; Chris Murrill, Alan Neaigus, Samuel Jenness, Holly Hagan, Travis Wendel, New York, New York; Helene Cross, Barbara Bolden, Sally D'Errico, Newark, New Jersey; Kathleen Brady, Althea Kirkland, Philadelphia, Pennsylvania; Vanessa Miguelino, Al Velasco, San Diego, California; H. Fisher Raymond, Willi McFarland, San Francisco, California; Sandra M. De León, Yadira Rolón-Colón, San Juan, Puerto Rico; Maria Courogen, Hanne Thiede, Nadine Snyder, Richard Burt, Seattle, Washington; Michael Herbert, Yelena Friedberg, Dale Wrigley, Jake Fisher, St. Louis, Missouri; Tiffany West-Ojo, Manya Magnus, Irene Kuo, District of Columbia.
References
- Purcell DW, Johnson C, Lansky A, et al. Calculating HIV and syphilis rates for risk groups: estimating the national population size of men who have sex with men. Presented at 2010 National STD Prevention Conference; Atlanta, GA. Abstract no. 22896.
- CDC. HIV surveillance report, 2009. Atlanta, GA: US Department of Health and Human Services, CDC; 2011. Available at http://www.cdc.gov/hiv/topics/surveillance/resources/reports. Accessed May 26, 2011.
- CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR 2006;55(No. RR-14).
- CDC. Prevalence and awareness of HIV infection among men who have sex with men---21 cities, United States, 2008. MMWR 2010;59:1201--7.
- Gallagher KM, Sullivan PS, Lansky A, et al. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Rep 2007;122(Suppl 1):32--8.
- MacKellar DA, Gallagher KM, Finlayson T, et al. Surveillance of HIV risk and prevention behaviors of men who have sex with men---a national application of venue-based, time-space sampling. Public Health Rep 2007;122(Suppl 1):39--47.
- Allen DR, Finlayson T, Abdul-Quadar A, et al. The role of formative research in the National HIV Behavioral Surveillance System. Public Health Rep 2009;124:26--33.
- CDC. Sexually transmitted diseases treatment guidelines, 2010. MMWR 2010;59(No. RR-12).
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702--6.
- Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS 2006;20:1447--50.
* The 21 MSAs included in this analysis were Atlanta--Sandy Springs--Marietta, GA; Baltimore--Towson, MD; Boston--Cambridge--Quincy, MA--NH: Boston--Quincy Division; Chicago--Joliet--Naperville, IL: Chicago--Joliet--Naperville Division; Dallas--Fort Worth--Arlington, TX: Dallas--Plano--Irving Division; Denver--Aurora--Broomfield, CO; Detroit--Warren--Livonia, MI: Detroit--Livonia--Dearborn Division; Houston--Sugar Land--Baytown, TX; Los Angeles--Long Beach--Santa Ana, CA: Los Angeles--Long Beach--Glendale Division; Miami--Ft. Lauderdale--Pompano Beach, FL: Miami Division; New Orleans--Metairie--Kenner, LA; New York--Northern New Jersey--Long Island, NY--NJ--PA: New York--White Plains--Wayne Division; New York--Northern New Jersey--Long Island, NY--NJ--PA: Nassau--Suffolk Division; New York--Northern New Jersey--Long Island, NY--NJ--PA: Newark--Union Division; Philadelphia--Camden--Wilmington, PA--NJ--DE--MD: Philadelphia Division; San Diego--Carlsbad--San Marcos, CA; San Francisco--Oakland--Fremont, CA: San Francisco--San Mateo--Redwood City Division; San Juan--Caguas--Guaynabo, PR; Seattle--Tacoma--Bellevue, WA: Seattle--Bellevue--Everett Division; St. Louis, MO--IL; and Washington--Arlington--Alexandria, DC--VA--MD--WV: Washington--Arlington--Alexandria Division.
What is already known on this topic?
The greatest numbers of human immunodeficiency virus (HIV) infections in the United States occur among men who have sex with men (MSM). CDC recommends that sexually active MSM be tested for HIV infection at least annually.
What is added by this report?
Data from MSM recruited by the National HIV Behavioral Surveillance System (NHBS) for interviews and HIV testing at venues in 21 U.S. cities indicated that 61% of MSM reported an HIV test during the preceding year; among these, 7% had a new, positive HIV test result.
What are the implications for public health practice?
Given the 7% prevalence of HIV infection among MSM who had not previously received a diagnosis of HIV infection and were tested for HIV during the preceding 12 months, sexually active MSM might benefit from more frequent HIV testing (e.g., every 3 to 6 months).
FIGURE. Time since most recent human immunodeficiency virus (HIV) test among men who have sex with men who were unaware they were HIV-infected* --- National HIV Behavioral Surveillance System, 21 cities, United States, 2008
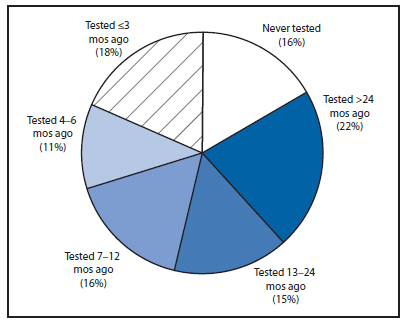
* N = 680.
Alternate Text: The figure above shows the time since most recent human immunodeficiency virus (HIV) test among men who have sex with men who were unaware they were HIV-infected in 21 U.S. cities in 2008, based on data from the National HIV Behavioral Surveillance System.
|
TABLE 2. (Continued) Proportion of men who have sex with men (MSM) with unrecognized human immunodeficiency virus (HIV) infection among MSM not previously diagnosed with HIV infection who had been tested during the past 12 months, by selected characteristics and risk behaviors --- National HIV Behavioral Surveillance System, 21 cities, United States, 2008* |
|||||||
|---|---|---|---|---|---|---|---|
|
Characteristic |
No. |
Unadjusted proportion HIV-infected and unaware |
Unadjusted prevalence ratio |
Adjusted prevalence ratio† |
|||
|
% |
(95% CI) |
PR |
(95% CI) |
PR |
(95% CI) |
||
|
No. of male sex partners during the past 12 mos |
|
|
|
||||
|
1 |
1,010 |
7.5 |
(6.0--9.3) |
--- |
--- |
||
|
2 |
683 |
8.6 |
(6.6--11.0) |
--- |
--- |
||
|
3 |
576 |
6.6 |
(4.7--8.9) |
--- |
--- |
||
|
≥4 |
2,184 |
6.1 |
(5.1--7.2) |
--- |
--- |
||
|
Methamphetamine use during the past 12 mos |
|
|
|
||||
|
Yes |
320 |
6.6 |
(4.1--9.9) |
--- |
--- |
||
|
No |
4,132 |
6.9 |
(6.1--7.7) |
--- |
--- |
||
|
Drug use before or during sex at most recent sex |
|
|
|
||||
|
Yes |
600 |
11.0 |
(8.6--13.8) |
--- |
--- |
||
|
No |
3,849 |
6.2 |
(5.5--7.0) |
--- |
--- |
||
|
Most recent partner had concurrent partners |
|
|
|
|
|
||
|
Definitely yes |
986 |
8.1 |
(6.5--10.0) |
--- |
--- |
||
|
Probably yes |
1,153 |
6.6 |
(5.2--8.2) |
--- |
--- |
||
|
Probably no |
758 |
6.2 |
(4.6--8.2) |
--- |
--- |
||
|
Definitely no |
1,217 |
6.2 |
(5.0--7.8) |
--- |
--- |
||
|
Reports one or more high-risk behaviors** |
|
|
|
||||
|
Yes |
3,672 |
6.7 |
(5.9--7.5) |
0.8 |
(0.6--1.1) |
0.9 |
(0.7--1.2) |
|
No |
781 |
8.0 |
(6.1--10.2) |
Referent |
Referent |
||
|
Unprotected anal intercourse during the past 12 mos |
|
|
|
||||
|
Yes |
2,541 |
6.3 |
(5.4--7.3) |
0.8 |
(0.7--1.02) |
1.0 |
(0.8--1.2) |
|
No |
1,907 |
7.7 |
(6.5--8.9) |
Referent |
Referent |
||
|
Type of partners during the past 12 mos |
|
|
|
||||
|
Main only |
1,161 |
7.4 |
(6.0--9.1) |
--- |
--- |
||
|
Main and casual |
1,799 |
6.7 |
(5.6--8.0) |
--- |
--- |
||
|
Casual only |
1,492 |
6.6 |
(5.4--8.0) |
--- |
--- |
||
|
Most recent HIV test |
|
|
|
||||
|
≤6 mos ago |
3,055 |
6.4 |
(5.6--7.4) |
Referent |
Referent |
||
|
7--12 mos ago |
1,353 |
7.8 |
(6.5--9.4) |
1.2 |
(0.97--1.5) |
1.2 |
(0.98--1.5) |
|
Unknown |
45 |
6.7 |
(1.4--18.3) |
1.03 |
(0.3--3.1) |
0.6 |
(0.2--1.9) |
|
Total |
4,453 |
6.9 |
(6.1--7.7) |
--- |
--- |
||
|
Abbreviation: CI = confidence interval; PR = prevalence ratio. * Numbers might not add to total because of missing data. † Adjusted for race/ethnicity, age, income, education, health insurance status, months since most recent HIV test, one or more high-risk behaviors, and unprotected anal intercourse. Robust variance estimation was used to calculate 95% confidence intervals for the adjusted prevalence ratios. Source: Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702--6. § Includes persons who indicated American Indian/Alaska Native, multiple races, or other race. ¶ 66% of respondents indicated a household size of one. ** High-risk behavior defined as the following: more than one male sex partner during the past 12 months, methamphetamine use during the past 12 months, drug use before or during sex at most recent sex, or most recent partner definitely or probably had concurrent partners. |
|||||||
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.


