FIGURE 1. Distribution of sleep duration and number of sleep-related difficulties among adults aged ≥20 years --- National Health and Nutrition Examination Survey, United States, 2005--2008
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Effect of Short Sleep Duration on Daily Activities --- United States, 2005--2008
Little is known about the extent to which insufficient sleep affects the ability of U.S. adults to carry out daily activities. The National Sleep Foundation suggests that adults need 7--9 hours of sleep per night; shorter and longer sleep durations have been associated with increased morbidity and mortality (1). To assess the prevalence of short sleep duration (<7 hours on weekday or workday nights) and its perceived effect on daily activities, CDC analyzed data from the 2005--2008 National Health and Nutrition Examination Survey (NHANES). This report summarizes the results, which found that 37.1% of U.S. adults reported regularly sleeping <7 hours per night, similar to the 35.3% reporting <7 hours of sleep in a 24-hour period in another report using self-reported data (2). Short sleep duration was more common among adults aged 20--39 years (37.0%) or 40--59 years (40.3%) than among adults aged ≥60 years (32.0%), and more common among non-Hispanic blacks (53.0%) than among non-Hispanic whites (34.5%), Mexican Americans (35.2%), and persons of other races/ethnicities (41.7%). Among six sleep-related difficulties assessed, the most prevalent was not being able to concentrate on doing things, reported by 23.2% of U.S. adults. Perceived sleep-related difficulties were significantly more likely among persons reporting <7 hours of sleep than among those reporting 7--9 hours of sleep. Based on these findings, at least one third of U.S. residents do not get enough sleep on a regular basis, and this impairs their ability to perform daily tasks. Chronic sleep deprivation also has a cumulative effect on mental and physical well-being and can exacerbate chronic diseases.
This analysis was conducted using data from the last two survey cycles (2005--2006 and 2007--2008) of NHANES, a stratified, multistage probability sample of the civilian noninstitutionalized U.S. population.* A total of 10,896 respondents aged ≥20 years who completed the interviewer-administered survey questions on sleep duration were included in the sample. The response rate for the interviewed sample was 74.8%. Responses to the question "how much sleep do you usually get at night on weekdays or workdays" were grouped into categories as <7 hours, 7--9 hours, and >9 hours. Responses to six questions from the Functional Outcomes of Sleep Questionnaire (3) about sleep-related difficulties also were analyzed.†
Descriptive statistics, including population estimates, weighted prevalence, and 95% confidence intervals (CIs), were calculated to account for the complex study design. Analyses were stratified by age, sex, race/ethnicity, and education. Population estimates for sleep duration categories and each sleep-related difficulty were calculated using NHANES 4-year sample weights, which account for the differential probabilities of selection, nonresponse, and noncoverage. To compare prevalence estimates among subgroups that differed by age distribution, all estimates except age-specific estimates were adjusted by the direct method to the 2000 U.S. population. Prevalence estimates were considered significantly different if the 95% CIs did not overlap.
A short sleep duration of <7 hours on weekdays or workdays was reported by 37.1% of respondents; 60.5% reported 7--9 hours of sleep, and 2.4% reported >9 hours (Figure 1). Approximately one third of respondents reported one or more sleep-related difficulties. Among adults who reported <7 hours of sleep, the prevalence of each of the six sleep-related difficulties was higher compared with adults who reported 7--9 hours of sleep (Figure 2). For both groups, the most common sleep-related difficulty was concentrating, which was reported by 19.4% of respondents who received 7--9 hours of sleep, but 29.3% of those who received <7 hours of sleep per night.
Respondents aged 20--39 years (37.0%) or 40--59 years (40.3%) were more likely to report a short sleep duration than those aged ≥60 years (32.0%) (Table). Men (39.8%) and women (35.3%) did not differ significantly in prevalence of short sleep duration. Non-Hispanic blacks (53.0%) had the highest prevalence of short sleep duration compared with other racial/ethnic populations. Respondents who reported at least some college education (34.5%) had a lower prevalence of short sleep duration than persons with only a high school diploma (40.9%).
Among U.S. adults, 13.5% reported three or more sleep-related difficulties (Figure 1). Overall, the greatest percentage (23.2%) reported difficulty concentrating on things because they were sleepy or tired, followed by difficulty remembering things (18.2%) and difficulty working on hobbies (13.3%) (Table). Difficulty driving or taking public transportation, taking care of financial affairs, or performing employed or volunteer work because of sleepiness or tiredness was reported by 11.3%, 10.5%, and 8.6% of respondents, respectively. Adults aged ≥60 years were less likely than younger adults to report having each of the six sleep-related difficulties, and women were more likely than men to report four of the six sleep-related difficulties. Women were more likely to report most sleep-related difficulties than men, regardless of sleep duration, but both men and women reported greater difficulties if they slept <7 hours compared with 7--9 hours.
Mexican Americans were less likely to report sleep-related difficulty in performing employed or volunteer work (4.9%), taking care of financial affairs (7.5%), and working on hobbies (8.7%) than non-Hispanic whites (9.1%, 10.7%, and 13.9%, respectively) and non-Hispanic blacks (8.7%, 11.2%, and 14.1%, respectively). Non-Hispanic blacks reported a greater prevalence than other racial/ethnic populations of sleep-related difficulty in driving or taking public transportation (14.8%). Persons with at least some college education were more likely to report sleep-related difficulty performing employed or volunteer work (9.8%), but less likely to report difficulty remembering things (17.0%), compared with persons with less than a high school education (6.7% and 20.8%, respectively) (Table).
Reported by
AG Wheaton, PhD, Y Liu, MS, MPH, GS Perry, DrPH, JB Croft, PhD, Emerging Investigations and Analytic Methods Br, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC.
Editorial Note
This is the first investigation of the relationship between reported short sleep duration and sleep-related difficulties in performing daily activities among persons in a broad, nonclinical population. The National Sleep Foundation suggests that adults need 7--9 hours of sleep per night; both shorter and longer sleep durations have been associated with increased morbidity and mortality (1). In this analysis, adults who reported usually getting <7 hours of sleep on weekdays or workdays were more likely to have difficulties with daily activities than adults who reported getting 7--9 hours of sleep. Women were more likely to report four of the six sleep-related difficulties than men, regardless of sleep duration. One factor that might contribute to these differences is that men and women might differ in their recognition of sleepiness and its effect on their ability to perform daily functions (4).
Most sleep disorders are marked by difficulty falling or staying asleep (e.g., insomnia), sleep-breathing disorders (e.g., sleep apnea), or abnormal movements, behaviors, or sensations during sleep (e.g., restless legs syndrome) (5). The sleep-related difficulty questions used in NHANES surveys have been used primarily to measure the effect of excessive sleepiness on functional outcomes in populations with disorders associated with excessive sleepiness (e.g., sleep apnea, narcolepsy, and depression). A previous analysis using 2005--2006 NHANES data found associations between having sleep apnea, insomnia, and restless legs syndrome and having sleep-related difficulties (6). In that NHANES sample, the prevalence of specific physician-diagnosed sleep disorders ranged from 4.2% for sleep apnea to 1.2% for insomnia and 0.4% for restless legs syndrome. Difficulties concentrating (44.1%--63.7%) and remembering (29.5%--44.6%) were the most prevalent sleep-related difficulties among persons with those sleep disorders (6).
The findings in this report are subject to at least five limitations. First, NHANES only surveyed the noninstitutionalized U.S. population; persons in nursing homes, the military, and other institutions were not included. Second, because of the cross-sectional design of NHANES, causality in the relationship between short sleep duration and the sleep-related difficulties could not be inferred. Third, this analysis relies on self-reported measures that cannot be validated. Fourth, the prevalence of drowsy driving, an important public safety issue related to sleepiness (7), could not be estimated because NHANES does not include a question about drowsy driving. Finally, this survey asked about duration of sleep at night, not about total sleep per 24-hour period; therefore, sleep duration estimates are not precisely comparable to those from surveys such as the Behavioral Risk Factor Surveillance System or the National Health Interview Survey.
Poor sleep habits, which include not scheduling enough time for sleep, can be assessed during general medical care visits and improved with effective behavioral changes. Health-care providers should advise patients who need to improve their sleep quality to 1) keep a regular sleep schedule; 2) avoid stimulating activities (e.g., vigorous exercise) within 2 hours of bedtime; 3) avoid caffeine, nicotine, and alcohol in the evening (8); 4) avoid going to bed on a full or empty stomach; and 5) sleep in a dark, quiet, well-ventilated space with a comfortable temperature. Because chronic sleep loss has a cumulative effect on mental and physical well-being, potentially exacerbating depression, obesity, diabetes, and other chronic conditions (5), treatment of patients with chronic diseases might benefit from counseling about the importance of sufficient sleep. Some patients might need referral to a sleep specialist for evaluation to determine whether they have a specific chronic sleep disorder. Evaluation might include sleep logs to monitor sleep patterns and polysomnography to assess breathing during sleep and measure rapid eye movement and physiologic changes during sleep. Treatment of chronic sleep disorders could include weight loss, changes in sleep behaviors, pharmacologic management, use of continuous positive airway pressure devices, use of dental devices, or upper airway surgery.
References
- National Sleep Foundation. How much sleep do we really need? Washington, DC: National Sleep Foundation; 2010. Available at http://www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need. Accessed February 22, 2011.
- CDC. Unhealthy sleep-related behaviors---12 states, 2009. MMWR 2011;60:233--8.
- Weaver TE, Laizner AM, Evans LK, et al. An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep 1997;20:835--43.
- Herrmann US, Hess CW, Guggisberg AG, Roth C, Gugger M, Mathis J. Sleepiness is not always perceived before falling asleep in healthy, sleep-deprived subjects. Sleep Med 2010;11:747--51.
- Institute of Medicine. Sleep disorders and sleep deprivation: an unmet public health problem. Washington, DC: National Academies Press; 2006. Available at http://www.iom.edu/cms/3740/23160/33668.aspx. Accessed February 22, 2011.
- Ram S, Seirawan H, Kumar SKS, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath 2010;14:63--70.
- National Highway Traffic Safety Administration. Drowsy driving. Ann Emerg Med 2005;45:433--4.
- Gillin JC, Drummond SPA, Clark CP, Moore P. Medication and substance abuse [Chapter 115]. In: Kryger MH, Roth T, Dement WC, eds. Principles and practice of sleep medicine. 4th ed. Philadelphia, PA: Elsevier; 2005.
* Data and additional information are available at http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
† The questions pertaining to the sleep-related difficulties were "Do you have difficulty concentrating on the things you do because you feel sleepy or tired?" "Do you generally have difficulty remembering things because you are sleepy or tired?" "Do you have difficulty working on a hobby, for example, sewing, collecting, gardening, because you are sleepy or tired?" "Do you have difficulty getting things done because you are too sleepy or tired to drive or take public transportation?" "Do you have difficulty taking care of financial affairs and doing paperwork (for example, paying bills or keeping financial records) because you are sleepy or tired?" and "Do you have difficulty performing employed or volunteer work because you are sleepy or tired?" Affirmative responses to these questions included a "yes" to any level of difficulty. Negative responses were "don't do this activity for other reasons," "no difficulty," or "don't know."
What is already known on this topic?
The National Sleep Foundation suggests that adults need 7--9 hours of sleep per night; shorter and longer sleep durations have been associated with increased morbidity and mortality.
What is added by this report?
Perceived difficulty in carrying out each of several daily activities because of being too sleepy or tired was as much as 50% greater among adults who usually slept <7 hours on weekdays or workdays than among those who usually slept 7--9 hours.
What are the implications for public health practice?
Public health workers should educate themselves and their communities on the substantial impact that insufficient sleep and sleep disorders have on health, wellness, and the ability to perform daily activities, such as concentrating and remembering things. Health-care providers can advise patients on lifestyle changes to improve sleep; patients with more serious sleep problems should be evaluated by a specialist.
* 95% confidence interval.
Alternate Text: The figure above shows the distribution of sleep duration and number of sleep-related difficulties among adults aged ≥20 years in the United States from 2005-2008, according to the National Health and Nutrition Examination Survey. According to the survey, a short sleep duration of <7 hours on weekdays or workdays was reported by 37.1% of respondents; 60.5% reported 7-9 hours of sleep, and 2.4% reported >9 hours. Among U.S. adults, 13.5% reported three or more sleep-related difficulties.
FIGURE 2. Age-adjusted prevalence of adults aged ≥20 years reporting sleep-related difficulty carrying out selected activities, by usual sleep duration --- National Health and Nutrition Examination Survey, United States, 2005--2008
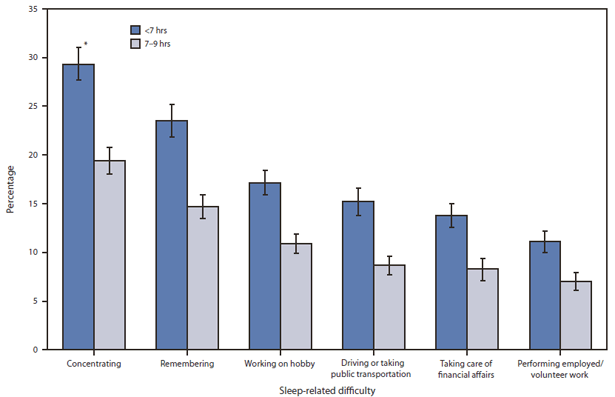
* 95% confidence interval.
Alternate Text: The figure above shows the age-adjusted prevalence of adults aged ≥20 years reporting sleep-related difficulty carrying out selected activities, by usual sleep duration in the United States from 2005-2008, according to the National Health and Nutrition Examination Survey. Among adults who reported <7 hours of sleep, the prevalence of each of the six sleep-related difficulties was higher compared with adults who reported 7-9 hours of sleep. For both groups, the most common sleep-related difficulty was concentrating, which was reported by 19.4% of respondents who received 7-9 hours of sleep, but 29.3% of those who received <7 hours of sleep per night.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


