FIGURE 1. Number of persons hospitalized with cholera, by department* --- Haiti, October 20--November 13, 2010
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Update: Cholera Outbreak --- Haiti, 2010
Please note: An erratum has been published for this article. To view the erratum, please click here.
On October 19, 2010, the Haitian Ministry of Public Health and Population (MSPP) was notified of unusually high numbers of patients from Artibonite and Centre departments who had acute watery diarrhea and dehydration, in some cases leading to death. Within 4 days, the National Public Health Laboratory (LNSP) in Haiti isolated Vibrio cholerae serogroup O1, serotype Ogawa, from stool specimens obtained from patients in the affected areas by an investigation team from MSPP and CDC Haiti. This report describes the investigation of the initial cases, the ongoing outbreak of cholera in Haiti, and initial control measures. Since the initial identification of cholera, the outbreak has expanded to include cases in seven of Haiti's 10 departments and the capital city of Port-au-Prince. As of November 13, MSPP had reported 16,111 persons hospitalized with acute watery diarrhea and 992 cholera deaths, 620 of which occurred among hospitalized patients. Prevention and control measures implemented by MSPP with assistance from governmental and nongovernmental partners include 1) providing better access to treated drinking water; 2) providing education on improvement of sanitation, hygiene, and food preparation practices; 3) advising ill persons to begin using oral rehydration solution immediately and seek health care at the onset of watery diarrhea; 4) enhancing cholera treatment capacity at existing health-care institutions; and 5) establishing cholera treatment centers.
Initial Epidemiologic Investigation
During October 21--23, an investigation was conducted by MSPP and CDC Haiti at five hospitals in Artibonite Department. The first patients with diarrhea and severe dehydration were admitted to these hospitals on October 19. During October 20--22, the majority of patients at these hospitals with diarrhea and severe dehydration were aged >5 years, and the majority of the patients at these hospitals who died were aged >5 years, suggesting that the outbreak might be caused by cholera.
On October 19 and 20, stool specimens from patients in health facilities in Artibonite and Centre departments were brought to LNSP, where rapid tests on eight specimens were positive for V. cholerae O1. LNSP identified V. cholerae serogroup O1, serotype Ogawa, from three specimens on October 22. Following confirmation of cholera, hospital staff members and public health authorities advised community members, including patients and their families, to boil or chlorinate their water before drinking.
During October 21--23, the investigative team used a standardized questionnaire to interview a convenience sample of 27 patients in the five hospitals in Artibonite Department. Most of these patients resided or worked in rice fields in communities located alongside a stretch of the Artibonite River approximately 20 miles (32 kilometers) long (Figure 1). Eighteen (67%) of the 27 hospitalized patients reported consuming untreated water from the river or canals before illness onset; 18 (67%) did not routinely use chlorine for treating water, and 21 (78%) practiced open defecation.
Cholera Surveillance and Laboratory Findings
A suspected case of cholera is defined as profuse, acute watery diarrhea in a patient. A confirmed case of cholera requires laboratory confirmation by culture of V. cholerae. When a department reports a case of laboratory-confirmed cholera, the department is declared "cholera affected." Only reports from cholera-affected departments are tallied and included in the MSPP daily surveillance summaries.
Since the initial identification of cholera in Artibonite and Centre departments, the outbreak has expanded to include cases in five additional departments and the capital city; cases have been reported in seven of 10 departments (Artibonite, Centre, Nord, Nord' Ouest, Nord' Est, Ouest, and Sud) and Port-au-Prince. As of November 13, MSPP had reported 16,111 persons hospitalized with acute watery diarrhea and 992 cholera deaths, 620 of which occurred among hospitalized patients (case-fatality rate among hospitalized patients: 3.8%) (Figure 2). Cases and deaths have been reported primarily from Artibonite department (63% of cases and 62% of deaths).
At LNSP, the outbreak isolates were identified as V. cholerae serotype O1, serogroup Ogawa, and selected specimens were sent to CDC for confirmation and additional analyses. As of November 13, CDC had isolated V. cholerae from 14 specimens received from LNSP. All isolates were identified phenotypically and characterized by serotyping, biotyping, antimicrobial susceptibility testing, and by pulsed-field gel electrophoresis (PFGE), performed using a protocol developed by PulseNet International, the international molecular subtyping network for foodborne and waterborne disease surveillance. Additionally, the isolates were characterized genetically for the presence and subtype of certain virulence factors (e.g., the cholera toxin, genes specific for strains associated with the ongoing cholera pandemic, and antimicrobial resistance genes). The 14 isolates associated with the outbreak in Haiti were indistinguishable by all laboratory methods, revealing that the outbreak strain was V. cholerae serogroup O1, serotype Ogawa, biotype El Tor, and PulseNet PFGE pattern combination KZGN11.0092/KZGS12.0088. The strain possessed a cholera toxin variant that was first seen in cholera strains of the classical biotype. As of November 13, data indicated that a single strain caused illness among the 14 persons from Artibonite Department. If these isolates are representative of those currently circulating in Haiti, the findings suggest that V. cholerae was likely introduced into Haiti in one event. V. cholerae strains that are indistinguishable from the outbreak strain by all methods used have previously been found in countries in South Asia and elsewhere. PFGE analysis on isolates obtained from cholera patients who became ill in other departments in Haiti is ongoing.
Whole genome sequence (WGS) analysis of three isolates from the current outbreak, and other V. cholerae strains is under way. Comparative WGS analysis is the ultimate discriminatory subtyping tool because it detects any and all genetic difference among isolates. Limited WGS data are available currently for V. cholerae. Comprehensive libraries of V. cholerae genomes from epidemiologically or geographically related and unrelated isolates are needed before the sequence data of the Haiti outbreak strain can be interpreted in the proper epidemiologic context.
A representative outbreak isolate has been deposited into the American Type Culture Collection (ATCC) under the strain number BAA- 2163, and the draft genome sequences of the three isolates have been deposited into the GenBank database under the accession numbers AELH00000000, AELI00000000, and AELJ00000000.* Genome sequences will be updated in this database as they become available. Availability of an isolate and WGS of the Haiti outbreak strain as a public resource should facilitate rapid additional characterization by the global scientific community.
Initial antimicrobial susceptibility testing performed at LNSP indicated that all isolates were susceptible to tetracycline (a proxy for doxycycline) but resistant to sulfisoxazole and nalidixic acid. Additional antimicrobial susceptibility testing at CDC on 14 isolates determined that these isolates demonstrated susceptibility to azithromycin, reduced susceptibility to ciprofloxacin, and resistance to furazolidone. Antimicrobial treatment is recommended for severe cholera cases only. Recommended regimens include single-dose doxycycline (for nonpregnant adults and children), azithromycin (for pregnant women and all others), and other antimicrobial agents.†
Prevention and Control Measures
MSPP, the Pan American Health Organization (PAHO), CDC, and selected health facilities have established national daily cholera surveillance and disseminated educational messages encouraging persons with acute watery diarrhea to use oral rehydration solution (ORS) and seek immediate medical care. MSPP and partners also developed and disseminated messages on cholera prevention encouraging persons to treat drinking water and to improve handwashing, sanitation, food preparation, and cleaning practices.§ Community surveys are under way to ascertain knowledge levels and practices among community members regarding cholera, ORS use, and safe water and sanitation practices, and to determine the need for additional prevention messages. Cholera treatment capacity was enhanced at existing health-care institutions, and new cholera treatment centers were opened with support from the Haitian government and other governmental and nongovernmental partners.
Reported by
Ministry of Public Health and Population, Haiti. Pan American Health Organization. CDC.
Editorial Note
Cholera, a gastrointestinal infection caused by toxigenic V. cholerae serogroup O1 or O139, can cause acute, severe, watery diarrhea, dehydration, and death. Outbreaks of cholera are frequent in Asia and Africa. During the 1990s, multiple countries in Latin America had cholera outbreaks; however, cholera was not reported from the Caribbean during or since that period. No cholera outbreaks have been reported from Haiti in more than a century (1--3). Known risk factors for cholera outbreaks include lack of access to safe drinking water, contaminated food, inadequate sanitation, and large numbers of refugees or internally displaced persons (IDPs).
The cholera outbreak in Haiti underscores the continuing vulnerability of much of the world's population to sudden severe illness and death from cholera. In 2009, a total of 221,226 cases of cholera and 4,946 cholera deaths were reported to the World Health Organization (WHO) from 45 countries; however, the actual number of annual cases is thought to be substantially higher (4). Haiti is the latest country to be affected by the ongoing cholera pandemic, which began 49 years ago in Sulawesi, Indonesia, and has lasted longer and spread farther than any previously known cholera pandemic (5).
Although multiple foods have been implicated as vehicles for cholera transmission, the driving forces in cholera outbreaks are contaminated drinking water and inadequate sanitation. In 2008, 63% of the 9.8 million persons in Haiti had access to an improved drinking water source¶; only 12% received piped, treated water, and only 17% had access to adequate sanitation (6). The earthquake on January 12, 2010, worsened conditions by damaging drinking water treatment facilities and piped water distribution systems, and displaced an estimated 2.3 million Haitians, further increasing the risk for waterborne outbreaks. The initial cholera outbreak investigation suggested that exposure to contaminated water was the likely cause of the initial cases in Artibonite Department. However, a case-control study is under way that will provide additional information about risk factors for illness in Artibonite. In addition, risk factors for illness might change as the outbreak expands over time. Contamination of food by persons who are ill, either via the use of contaminated water or poor food preparation hygiene also can contribute to the spread of disease.
Vigorous efforts to restore public health surveillance and laboratory diagnostic capacity in Haiti after the earthquake enabled rapid detection and identification of V. cholerae by MSPP within a few days of the first case report and determination of the antimicrobial susceptibility of circulating strains followed soon after. The Haitian government immediately declared a public health emergency and has worked closely with international organizations and governmental and nongovernmental partners to raise community awareness of and access to cholera prevention and treatment measures, strengthen staffing and treatment supplies at health centers in affected areas, and support creation of dedicated cholera treatment centers in those areas already affected and in areas not yet affected by cholera. Suspected cases in unaffected areas will be identified and reported to MSPP through enhanced daily surveillance and laboratory testing. As surveillance systems improve and outpatients with cholera are reported, the number of cases identified is likely to increase substantially.
Early administration of ORS is the mainstay of cholera treatment and should begin as soon as symptoms develop, continue while the patient seeks medical care, and be maintained until hydration returns to normal in the health-care facility. ORS, combined with intravenous rehydration for those with severe dehydration, has been shown to reduce case-fatality rates to <1% (7). ORS is available in Haiti, but continued emphasis on maintaining supplies at the local level, dissemination of messages about how to correctly prepare and use ORS at home, and provision of ORS for use in the home, is needed. Health-care facilities in Haiti will need considerable assistance in preparing their facilities to provide the rapid clinical assessment and aggressive rehydration treatment necessary to reduce the risk for death from severe cholera.
The course of the cholera outbreak in Haiti is difficult to predict. The Haitian population has no preexisting immunity to cholera, and environmental conditions in Haiti are favorable for its continued spread. Approximately 1.3 million Haitians remain in IDP camps (8), but the capacity of IDP camps to provide centrally treated drinking water, adequate sanitation, handwashing facilities, and health care varies. The number of cases might be lowered substantially if efforts to reduce transmission are implemented fully (Box), but they also might be increased substantially by delays in implementation, flooding, or other disruptions. Longer-term persistence of V. cholerae in the environment in Haiti and recurrent cholera outbreaks also are possible. After the January 12, 2010, earthquake, intensive efforts to provide safe drinking water and sanitation were made in some areas. Expanding these activities over the coming months and years will be critical to reducing the risk for cholera in Haiti and protecting the Haitian population from other waterborne diseases.
During November 15--16, CDC, MSPP, and the International Centre for Diarrhoeal Disease Research, Bangladesh (ICCDR,B) launched a 2-day train-the-trainer program in Port-au-Prince to educate health-care providers on cholera treatment and management techniques in Haiti. Master trainers were trained and are now prepared to train additional health-care workers in departments across Haiti in the next few weeks. The train-the-trainer program will expand beyond the persons directly trained by CDC, MSPP, and ICDDR,B to reach a much larger number of Haitians providing health-care to patients in the communities. The train-the-trainer program is designed to improve the standard of care of cholera patients and reduce the number of cholera patients dying from severe dehydration.
Travelers to Haiti are encouraged to take certain basic precautions to reduce their risk for acquiring cholera (9). Further spread of cholera from Haiti to other countries might occur; therefore, cholera surveillance should be enhanced in those areas. Exports from Haiti, including foods, are not likely to pose a risk for cholera transmission. However, CDC discourages travelers from bringing noncommercial, perishable "souvenir seafood" from Haiti to the United States because of the risk for contamination (10).
References
- Pollitzer R, Swaroop S, Burrows W. Cholera. Monogr Ser World Health Organ 1959;58:1001--19.
- Guerra F. American and Filipino epidemiology, 1492--1898. Madrid, Spain: Ministry of Health and Consumption; 1999.
- Bordes A. Vol. 2. Médecine et santé publique sous l'occupation Américaine, 1915--1934. In: Évolution des sciences de la santé et de l'hygiène publique en Haïti. Port-au-Prince, Haiti: Centre d'Hygiène Familiale. Imprimerie Deschamps; 1979.
- World Health Organization. Cholera, 2009. Wkly Epidemiol Rec 2010;85:293--308.
- Wachsmuth IK, Blake PA, Olsvik O, eds. Vibrio cholerae and cholera: molecular to global perspectives. Washington, DC: ASM Press; 1994:293--5.
- World Health Organization and UNICEF. Progress on sanitation and drinking water: 2010 update. Geneva, Switzerland: WHO Press; 2010. Available at http://www.who.int/water_sanitation_health/publications/9789241563956/en/index.html. Accessed November 16, 2010.
- Swerdlow DL, Ries AA. Cholera in the Americas: guidelines for the clinician. JAMA 1992;267:1495--9.
- United Nations Office for the Coordination of Humanitarian Affairs, Haiti. Situation report no. 7. October 28, 2010. Available at http://www.reliefweb.int/rw/rwfiles2010.nsf/filesbyrwdocunidfilename/mmah-8ap826-full_report.pdf/$file/full_report.pdf. Accessed November 16, 2010.
- CDC. Traveler's health. Outbreak notice: cholera in Haiti. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://wwwnc.cdc.gov/travel/content/outbreak-notice/haiti-cholera.aspx. Accessed November 16, 2010.
- Finelli L, Swerdlow D, Mertz K, Ragazzoni H, Spitalny K. Outbreak of cholera associated with crab brought from an area with epidemic disease. J Infect Dis 1992;166:1433--5.
* Information available at http://www.ncbi.nlm.nih.gov/nuccore/AELH00000000, http://www.ncbi.nlm.nih.gov/nuccore/AELI00000000, and http://www.ncbi.nlm.nih.gov/nuccore/AELJ00000000.
† Additional information available at http://www.cdc.gov/haiticholera/clinicalmanagement.
§ Additional information available at http://new.paho.org/blogs/haiti/?p=274.
¶ Defined as a piped household water connection located inside the user's dwelling, plot, or yard; public taps or standpipes; tube wells or boreholes; protected dug wells; protected springs; or rainwater collection.
What is already known on this topic?
A cholera outbreak has not been reported from Haiti in more than a century.
What is added by this report?
In October 2010, an outbreak of Vibrio cholerae serogroup O1, serotype Ogawa, biotype El Tor, was reported from Haiti; as of November 13, the Haitian Ministry of Public Health and Population had reported 16,111 hospitalized cases of acute watery diarrhea and 992 cholera deaths, 620 of which occurred among hospitalized patients. Laboratory data suggest that V. cholerae was likely introduced into Haiti in one event and that the strain is indistinguishable by all methods used from strains circulating in countries in South Asia and elsewhere.
What are the implications for public health practice?
Continued cholera surveillance is required to follow the course of the outbreak and to target resources in areas of greatest need. Cholera treatment and prevention strategies need to be enhanced. Long-term improvements in water and sanitation likely will be needed to control cholera in Haiti. Travelers to Haiti are encouraged to take certain basic precautions to reduce their risk for acquiring cholera.
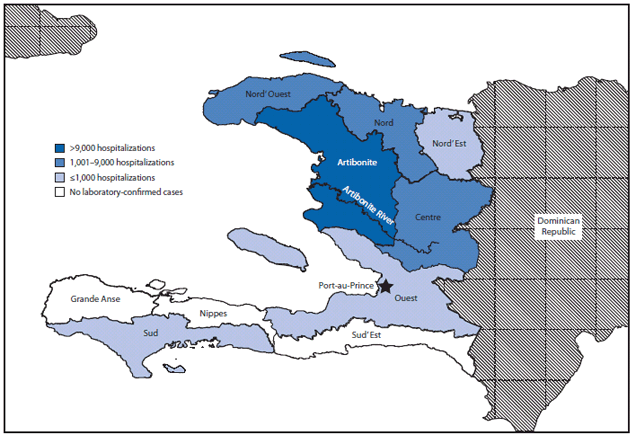
* Artibonite (10,230), Nord' Ouest (1,548), Nord (1,513), Centre (1,086), Port-au-Prince (875), Ouest outside of Port-au-Prince (794), Sud (45), and Nord' Est (1).
Alternate Text: The figure above shows the number of persons hospitalized with cholera (N = 16,111), by department in Haiti during October 20-November 13, 2010. Most of the hospitalizations (10,230) occurred in Artibonite Department.
FIGURE 2. Number of persons hospitalized (N=16,111) with cholera and daily hospital case-fatality rate (CFR) --- Haiti, October 20--November 13, 2010
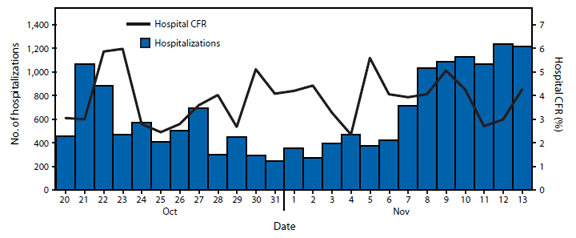
Alternate Text: The figure above shows the number of persons hospitalized with cholera and the daily hospital case-fatality rate in Haiti, during October 20-November 13, 2010. As of November 13, MSPP had reported 16,111 persons hospitalized with acute watery diarrhea and 992 cholera deaths, of which 620 occurred among hospitalized patients (case-fatality rate among hospitalized patients: 3.8%).
|
BOX. Recommendations for reducing the risk for cholera --- Haiti, 2010* |
|
Drink and use safe water
Be sure water is safe to drink and use
Cook food well, keep it covered, eat it hot, and peel fruits and vegetables.
Wash hands often with soap and water
Use latrines or bury feces; do not defecate in any body of water.
What if I don't have a latrine or chemical toilet?
Clean up safely, in the kitchen and in places where the family bathes and washes clothes.
|
|
Source: CDC. Five basic cholera prevention messages. Available at http://www.cdc.gov/haiticholera/five_messages.htm. * Additional information regarding cholera is available at http://www.cdc.gov/cholera. |
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


