|
TABLE 1. Estimated lifetime risk for HIV diagnosis, by race/ethnicity and sex --- 37 states and Puerto Rico, 2007 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Race/Ethnicity* |
Male |
Female |
Total |
||||||
|
Risk (%) |
(95% CI) |
Estimated HIV diagnoses in 2007 |
Risk (%) |
(95% CI) |
Estimated HIV diagnoses in 2007 |
Risk (%) |
(95% CI) |
Estimated HIV diagnoses in 2007 |
|
|
Total† |
1.98 |
(1.95--2.00) |
30,789 |
0.72 |
(0.71--0.73) |
10,822 |
1.36 |
(1.35--1.37) |
41,611 |
|
American Indian/Alaska Native |
1.00 |
(0.84--1.29) |
140 |
0.46 |
(0.35--0.67) |
65 |
0.76 |
(0.65--0.91) |
205 |
|
Asian |
0.69 |
(0.61--0.88) |
336 |
0.19 |
(0.15--0.33) |
94 |
0.45 |
(0.40--0.54) |
430 |
|
Black/African American |
6.27 |
(6.17--6.38) |
13,337 |
3.09 |
(3.02--3.17) |
6,810 |
4.65 |
(4.59--4.71) |
20,147 |
|
Hispanic/Latino |
2.80 |
(2.73--2.88) |
6,533 |
0.94 |
(0.90--0.99) |
1,878 |
1.92 |
(1.88--1.97) |
8,411 |
|
Native Hawaiian/Other Pacific Islander |
3.06 |
(2.00--32.67) |
35 |
0.55 |
(0.13--16.13) |
5 |
1.86 |
(1.24--12.71) |
40 |
|
White |
0.98 |
(0.96--1.00) |
10,107 |
0.19 |
(0.18--0.19) |
1,855 |
0.59 |
(0.58--0.60) |
11,962 |
|
Abbreviations: CI = confidence interval; HIV = human immunodeficiency virus. * Racial populations are all non-Hispanic. Hispanics/Latinos might be of any race. † Includes persons of multiple races. |
|||||||||
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Estimated Lifetime Risk for Diagnosis of HIV Infection Among Hispanics/Latinos --- 37 States and Puerto Rico, 2007
In 2008, the annual rate of diagnosis with human immunodeficiency virus (HIV) infection in the United States for Hispanics/Latinos (25.0 per 100,000 population) was approximately three times that for whites (8.2) (1). To calculate the estimated lifetime risk (ELR) and age-conditional risk for diagnosis of HIV infection among Hispanics/Latinos in 37 states and Puerto Rico, CDC analyzed HIV surveillance data, vital statistics data on general and HIV-specific mortality, and U.S. census data from 2007. The results of those analyses indicated that an estimated 1.92% (one in 52) of Hispanics/Latinos would receive HIV diagnoses during their lifetimes, compared with an ELR for HIV diagnosis of 0.59% (one in 170) for whites and 4.65% (one in 22) for blacks/African Americans. Among Hispanics/Latinos, those aged 35 years had the greatest risk for HIV diagnosis (males: 0.77% and females: 0.24%) during the next 10 years. Reducing HIV risk behaviors and increasing access to testing and care are important to decrease the number of diagnoses of HIV infection among disproportionately affected population groups.
To estimate lifetime risk and age-conditional risk, the number of HIV diagnoses in 2007 for persons in Puerto Rico and the 37 states with name-based HIV reporting since 2005* were obtained from the national HIV surveillance system. General and HIV-specific mortality data were obtained from death certificates from the 37 states and Puerto Rico for 2007. Population data for the 37 states were based on official postcensus estimates for 2007 from the U.S. Census Bureau (2). Because the postcensus estimates were not available for Puerto Rico by race/ethnicity, the 2000 census summary file was used to impute postcensus population estimates for Puerto Rico by race/ethnicity. Lifetime risk and age-conditional risk for HIV diagnosis were computed using statistical software (3) that can estimate the probabilities of acquiring a disease through analysis of population-based surveillance information. Lifetime risk modeling was based on a hypothetical cohort of 10 million live births, and probability estimates were derived for each 5-year age group in the cohort. The inverse of lifetime risk yields an estimate for the number of persons who would need to be followed throughout the specified life years to observe one HIV diagnosis (with smaller numbers indicating more likely diagnosis with HIV). For age-conditional risk, the percentage of HIV-uninfected persons aged 20--50 years expected to receive a diagnosis of HIV infection during the next 10 years was calculated at 5-year age intervals. HIV surveillance data were statistically adjusted to account for reporting delay (1).
In 2007, an estimated 41,611 persons received HIV diagnoses in the 37 states and Puerto Rico, of whom 8,411 (20.2%) were Hispanics/Latinos (Table 1). Overall, ELR for HIV diagnosis among Hispanics/Latinos was 1.92%, compared with 4.65% for blacks/African Americans, 1.86% for Native Hawaiians/Other Pacific Islanders, 0.76% for American Indians/Alaska Natives, 0.59% for whites, and 0.45% for Asians (Table 1). Among Hispanics/Latinos in Puerto Rico, ELR was 2.08%, whereas, among those in the 37 states, ELR was 1.90%.
By sex, ELR for HIV diagnosis was 2.80% (one in 36) among Hispanic/Latino males and 0.94% (one in 106) among Hispanic/Latino females (Table 1). ELR for white males and females was 0.98% and 0.19%, respectively. Among Hispanics/Latinos, ELR for both males and females increased slowly from ages 10--14 to 15--19 years, then increased more rapidly, but steadily, until approximately ages 50--54 years, when the rate of increase began to slow, leveling off at approximately ages 65--69 years. ELR for males was greater than that for females in every age group (Figure).
Among Hispanic/Latino males and females aged 20--50 years, calculations at 5-year intervals indicated that those who were HIV-uninfected at age 35 years had the greatest risk for HIV diagnosis in the next 10 years (males: 0.77% and females: 0.24%). The next greatest risks were among HIV-uninfected males at age 30 years (0.74%) and HIV-uninfected females at age 40 years (0.24%) (Table 2).
Reported by
WK Adih, MD, X Hu, MS, ML Campsmith, DDS, L Espinoza, DDS, HI Hall, PhD, Div of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC.
Editorial Note
The findings in this report reflect the disproportionate ELR for diagnosis of HIV infection among Hispanics/Latinos, compared with whites, and is consistent with other analyses of surveillance data (1). The ELR for HIV diagnosis for Hispanics/Latinos was approximately three times that for whites and, among racial/ethnic populations, was greater than all populations except blacks/African Americans. By sex, ELR for Hispanic/Latino males and females was three times and five times that for white males and females, respectively, confirming a previous analysis of data from 33 states (4). The greater ELR for HIV diagnosis for Hispanic/Latino males compared with females likely resulted from the high number of HIV diagnoses among Hispanic/Latino men who have sex with men (1).
Multiple factors might contribute to the disproportionate ELR for HIV diagnosis among Hispanics/Latinos, compared with whites. Migration (both within and across national borders) in search of work might contribute to increased HIV risk behaviors; change in residence can result in loneliness, isolation, and disruption of social, familial, and sexual relationships (5). These factors can lead to new sex partners, illegal drug use, and inadequate access to health-care services. Poverty, culture, limited use of English, and immigration status also represent barriers to obtaining information about HIV prevention (5). Lack of awareness regarding the risk for HIV infection also might be a factor affecting risk behaviors among some Hispanics/Latinos (6).
The findings in this report are subject to at least three limitations. First, the estimates of HIV diagnoses are from 37 states and Puerto Rico and thus do not represent all HIV diagnoses in the United States. HIV surveillance data from several high-morbidity areas with sizeable Hispanic/Latino populations (e.g., California) are not yet available; inclusion of such data in the future will provide a more complete and accurate analysis of the epidemiology of HIV for Hispanics/Latinos. Second, potential exists for racial/ethnic misclassification in the surveillance and mortality data, with some Hispanics/Latinos classified as white (7). Such misclassification can attenuate the actual differences by race/ethnicity. Finally, the statistical adjustment procedures applied to HIV surveillance data to account for reporting delay are subject to a degree of uncertainty (1), which could result in overadjustment or underadjustment of the data. However, this uncertainty would be applied across race/ethnicity categories and would not affect data for Hispanics/Latinos disproportionately.
CDC is engaged in a wide range of activities to reduce the disparity in HIV diagnoses among minority populations, including Hispanics/Latinos. CDC has adapted its evidence-based HIV behavioral interventions from the Diffusion of Effective Behavioral Interventions project (8) for Hispanics/Latinos; an example is VOICES/VOCES, a video-based intervention designed to increase condom use among heterosexual black/African American and Hispanic/Latino men who visit STD clinics.† Another program, Popular Opinion Leader (POL), identifies, enlists, and trains key opinion leaders to encourage safer sex norms and behaviors among young Hispanic/Latino migrant men who have sex with men.§ In 2009, CDC launched a communication campaign, Act Against AIDS, to address complacency, lack of knowledge, and misperceptions about HIV and AIDS in the United States (9). Many of the resources and messages in the campaign are available in Spanish, with electronic and print media campaigns currently under way in several cities with large Hispanic/Latino populations.
The National HIV/AIDS Strategy (10) calls for increased focus on interventions for Hispanics/Latinos, such as culturally and linguistically appropriate interventions that include effective communication strategies, expansion of HIV testing and diagnosis, and improved access to prevention, care, and treatment services to reduce the number of new HIV infections. The goal is to lower ELR for HIV diagnosis and reduce the disproportionate impact of HIV in the Hispanic/Latino population.
References
- CDC. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2008: HIV surveillance report, volume 20. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.cdc.gov/hiv/surveillance/resources/reports/2008report/index.htm. Accessed October 8, 2010.
- US Census Bureau. Population estimates. Available at http://www.census.gov/popest/estimates.php. Accessed October 8, 2010.
- National Cancer Institute. DevCan: probability of developing or dying of cancer. Bethesda, MD: National Institutes of Health, National Cancer Institute; 2010. Available at http://www.srab.cancer.gov/devcan. Accessed October 8, 2010.
- Hall HI, An Q, Hutchinson AB, Sansom S. Estimating the lifetime risk of a diagnosis of the HIV infection in 33 states, 2004--2005. J Acquir Immune Defic Syndr 2008;49:294--7.
- Organista KC, Carrillo H, Ayala G. HIV prevention with Mexican migrants: review, critique, and recommendations. J Acquir Immune Defic Syndr 2004;37(suppl 4):S227--39.
- Shedlin MG, Decena CU, Oliver-Velez D. Initial acculturation and HIV risk among new Hispanic immigrants. J Natl Med Assoc 2005;97(7 Suppl):32--7S.
- Swallen KC, West DW, Stewart SL. et al. Predictors of misclassification of Hispanic ethnicity in a population-based cancer registry. Ann Epidemiol 1997;7:200--6.
- CDC. 2009 compendium of evidence-based HIV prevention interventions. Atlanta, GA: US Department of Health and Human Services, CDC; 2009. Available at http://www.cdc.gov/hiv/topics/research/prs/evidence-based-interventions.htm. Accessed October 8, 2010.
- CDC. Act against AIDS. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.nineandahalfminutes.org. Accessed October 8, 2010.
- Office of National AIDS Policy. National HIV/AIDS strategy. Washington, DC: Office of National AIDS Policy; 2010. Available at http://www.whitehouse.gov/onap. Accessed October 8, 2010.
* Alabama, Alaska, Arizona, Arkansas, Colorado, Connecticut, Florida, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, New Hampshire, New Jersey, New Mexico, New York, Nevada, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, and Wyoming.
† Information available at http://www.cdc.gov/hiv/topics/research/prs/resources/factsheets/voices-voces.htm.
§ Information available at http://www.cdc.gov/hiv/topics/prev_prog/rep/packages/pol.htm.
What is already known on this topic?
In the United States, Hispanics/Latinos are disproportionately impacted by human immunodeficiency virus (HIV) compared with whites.
What is added by this report?
Data from 37 states and Puerto Rico indicated that an estimated 1.92% (one in 52) of Hispanics/Latinos would receive HIV diagnoses during their lifetimes, approximately three times the lifetime risk for whites. Among Hispanics/Latinos, those aged 35 years had the greatest risk for a diagnosis of HIV infection during the next 10 years.
What are the implications for public health practice?
Culturally and linguistically appropriate interventions, including effective communication strategies and expansion of access to testing and care services, are necessary to reduce the disproportionate impact of HIV infection among Hispanics/Latinos.
FIGURE. Estimated lifetime risk for HIV diagnosis among Hispanics/Latinos, by age group and sex --- 37 states and Puerto Rico, 2007
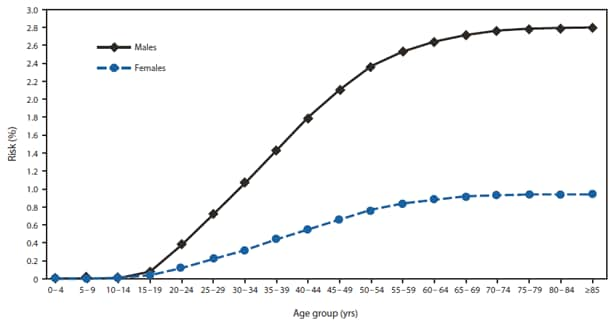
Abbreviation: HIV = human immunodeficiency virus.
Alternate Text: The figure above shows the estimated lifetime risk (ELR) for HIV diagnosis among Hispanics/Latinos, by age group and sex in 37 states and Puerto Rico in 2007. Among Hispanics/Latinos, ELR for both males and females increased slowly from ages 10-14 to 15-19, then increased more rapidly, but steadily, until approximately ages 50-54, when the rate of increase began to slow, leveling off at approximately ages 65-69. ELR for males was greater than that for females in every age group.
|
TABLE 2. Estimated 10-year age-conditional risk for HIV diagnosis among HIV-uninfected Hispanic/Latino males and females aged 20--50 years --- 37 states and Puerto Rico, 2007 |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Sex |
At age 20 yrs |
At age 25 yrs |
At age 30 yrs |
At age 35 yrs |
At age 40 yrs |
At age 45yrs |
At age 50 yrs |
|||||||
|
Risk (%) |
(95% CI) |
Risk (%) |
(95% CI) |
Risk (%) |
(95% CI) |
Risk (%) |
(95% CI) |
Risk (%) |
(95% CI) |
Risk (%) |
(95% CI) |
Risk (%) |
(95% CI) |
|
|
Male |
0.65 |
(0.59--0.68) |
0.71 |
(0.68--0.74) |
0.74 |
(0.71--0.77) |
0.77 |
(0.74--0.80) |
0.71 |
(0.68--0.75) |
0.61 |
(0.58--0.65) |
0.47 |
(0.43--0.50) |
|
Female |
0.18 |
(0.17--0.20) |
0.20 |
(0.18--0.21) |
0.22 |
(0.20--0.24) |
0.24 |
(0.22--0.26) |
0.24 |
(0.21--0.26) |
0.22 |
(0.20--0.24) |
0.18 |
(0.16--0.20) |
|
Abbreviations: CI = confidence interval; HIV = human immunodeficiency virus. |
||||||||||||||
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


