FIGURE. Timeline of course for a patient with presumptive abortive human rabies --- Texas, 2009
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Presumptive Abortive Human Rabies --- Texas, 2009
Rabies is a serious zoonotic disease. Recovery has been well documented in only six human patients worldwide (1,2). Five of those patients had received rabies vaccinations before illness; one had not received rabies vaccination but survived infection after prolonged intensive care. In most of these survivors, moderate to profound neurologic sequelae occurred (2,3). In all six survivors, rabies was diagnosed based on exposure history, compatible clinical symptoms, and detection of rabies virus-neutralizing antibodies (VNA). This report describes the clinical course and laboratory findings of an adolescent girl with encephalitis who had not had rabies vaccination and who had been exposed to bats 2 months before illness. Antibodies to rabies virus were detected in specimens of the girl's serum and cerebrospinal fluid (CSF) by indirect fluorescent antibody test (IFA). However, the presence of rabies VNA was not detected until after she had received single doses of rabies vaccine and human rabies immune globulin (HRIG). Although the patient required multiple hospitalizations and follow-up visits for recurrent neurologic symptoms, she survived without intensive care. No alternate etiology was determined, and abortive human rabies (defined in this report as recovery from rabies without intensive care) was diagnosed. Public education should emphasize avoiding exposure to bats and other potentially rabid wildlife and seeking prompt medical attention after exposure to such animals. Rabies is preventable if rabies immune globulin and vaccine are administered soon after an exposure; however, this case also suggests the rare possibility that abortive rabies can occur in humans and might go unrecognized.
Case Report
On February 25, 2009, an adolescent girl aged 17 years went to a community hospital emergency department with severe frontal headache, photophobia, emesis, neck pain, dizziness, and paresthesia of face and forearms. The headaches had begun approximately 2 weeks before she went to the hospital (Figure). Her examination was significant for intermittent disorientation, with a Glasgow Coma Score of 14, nuchal rigidity, and fever to 102.0oF (38.9oC). Computed tomography of her head was normal. A lumbar puncture (LP) was performed and revealed a white blood cell (WBC) count of 163/mm3, no red blood cells (RBC), 97% lymphocytes, 3% monocytes, and glucose of 61 mg/dL (Table 1). The patient was treated with intravenous ceftriaxone and dexamethasone, but when CSF bacterial cultures produced no growth, these medications were discontinued. After 3 days in the hospital, the girl's symptoms resolved, and she was discharged home.
Subsequently, her headaches recurred and intensified; on March 6, she went to another local hospital with photophobia, emesis, and myalgias, particularly of the neck and back. Magnetic resonance imaging (MRI) of her head demonstrated enlarged lateral ventricles for her age; another LP was performed and revealed a protein level of 160 mg/dL, WBC count of 185/mm3, and RBC count of 1/mm3 with 95% lymphocytes and 5% macrophages (Table 1). She was transferred to a tertiary-care children's hospital that same day.
On admission to the hospital (Figure), she was afebrile, alert, and oriented. Fundoscopic examination demonstrated a blurring of disk margins bilaterally. She was photophobic with transient limitation of vision in the left visual field. Initially, she had decreased strength of the left lower and upper extremities, but it resolved during subsequent examinations. She also had a new papular pruritic rash on her arms and back. She received a diagnosis of suspected infectious encephalitis and was treated during the hospitalization with intravenous acyclovir, ceftriaxone, ethambutol, isoniazid, pyrazinadmide, and rifapmin. On March 10, the girl reported loss of sensation and strength of the right extremities, and weakness was confirmed on examination. Emesis increased, and she became agitated and combative. But these symptoms resolved the next day. Repeat LP demonstrated increased intracranial pressure (Table 1).
An extensive workup for potential etiologies of encephalitis/aseptic meningitis was performed, but no definitive etiology was determined (Table 2). On March 10, the medical team elicited a history of bat exposure, and rabies was considered in the differential diagnosis. The patient recalled that approximately 2 months before her headaches began she had entered a cave while on a camping trip in Texas and came into contact with flying bats. Although several bats hit her body, she did not notice any bites or scratches. The patient also reported owning pet ferrets and a dog; all were in good health and under routine veterinary care.
The patient reportedly had never received rabies prophylaxis. On March 11, serologic tests of serum and CSF for antirabies virus antibodies, polymerase chain reaction (PCR) tests of saliva and nuchal skin biopsy for the presence of rabies virus RNA, and direct fluorescent antibody tests of the nuchal biopsy for rabies virus antigen were performed at CDC. No rabies virus antigens or RNA were detected. However, four serum and CSF samples tested positive for rabies virus antibodies by IFA. Serum immunoglobulin G (IgG) reactivity increased to a peak dilution of 1:8192 and immunoglobulin M (IgM) to 1:32. The CSF IgG was positive up to dilution 1:32 through March 19 and by April 3 had decreased to 1:8. The CSF IgM remained negative (Table 1). The positive IFA results were corroborated by a Western blot assay performed in blinded fashion by an independent investigator. Although rabies virus can crossreact serologically with other members of the Lyssavirus genus, Kern Canyon virus (KCV) is the only other rhabdovirus associated with bats in North America that potentially could demonstrate a limited serologic crossreactivity with rabies virus. KCV RNA was not detected in the patient's skin biopsy, saliva, and CSF by nested PCR.
On March 14, after notification of positive rabies serology results, the girl received 1 dose of rabies vaccine and 1,500 IU of HRIG. Additional doses of vaccine were not administered because of concern over possible adverse effects from potentiating the immune response. On March 19 and March 29, the patient's serum tested positive for rabies VNA by the rapid fluorescent focus inhibition test (RFFIT), whereas her CSF remained negative for rabies VNA (Table 1).
The patient was managed supportively and never required intensive care. She was discharged on March 22 with clinical symptom resolution but returned to the emergency department on March 29 with recurring headache. She left before an LP could be performed, but returned to the emergency department again on April 3 with headache and emesis. At that time, an LP was performed, and her CSF opening pressure was still elevated (Table 1). After the LP, her headache resolved. She was not rehospitalized and did not return for follow up in the outpatient clinic.
Questionnaires were administered to close friends and family members of the girl and to health-care workers to assess indications for postexposure prophylaxis (PEP). Only the girl's boyfriend met the criteria and received PEP (4). The current clinical status of the patient or her boyfriend is unknown.
Reported by
G Holzmann-Pazgal, MD, A Wanger, PhD, G Degaffe, MD, C Rose, MD, G Heresi, MD, R Amaya MD, Univ of Texas School of Medicine Dept of Pediatrics; A Eshofonie, MD, H Lee-Han, PhD, A Awosika-Olumo, MD, Bur of Epidemiology, Office of Surveillance and Public Health Preparedness, Houston Dept of Health and Human Svcs, Houston, Texas. I Kuzmin, MD, PhD, CE Rupprecht, VMD, PhD, Div of Viral and Rickettsial Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases, CDC.
Editorial Note
This is the first reported case in which certain clinical and serologic findings indicate abortive human rabies and in which, despite an extensive medical investigation, no alternate etiology for the illness was determined. The patient's positive serologic results offer evidence of rabies virus infection; IFA and Western blot assays indicated the presence of antibodies capable of binding to rabies virus antigens before the patient received rabies PEP. Rabies virus can crossreact serologically with other members of the Lyssavirus genus, distributed in Australia, Eurasia, and Africa (5) or, theoretically, with as yet uncharacterized rhabdoviruses. However, this patient had no history of foreign travel and no evidence of infection with KCV, the only other rhabdovirus associated with bats in North America.
Laboratory diagnosis of rabies antemortem is based typically on routine detection of viral antigen in a full-thickness skin biopsy, viral RNA in the skin biopsy or saliva, or antibodies in serum and CSF. Only antibodies were found in this patient. However, viral antigen and RNA often are not detected in infected humans antemortem because of limited virus replication and intermittent viral excretion in saliva (1,4,6). Notably, the diagnosis of rabies in all human survivors has been based solely on serologic findings, including the presence of VNA, but without virus isolation or detection of viral antigens or RNA (2,6).
Certain other clinical and laboratory findings also support a diagnosis of abortive rabies in the patient described in this report. First, the onset of acute encephalopathy approximately 2 months after exposure to bats is compatible with documented incubation periods after rabies virus exposure. Second, central nervous system (CNS) findings (e.g., fever, photophobia, emesis, neck pain, dizziness, paresthesia, limitation of visual field, and altered behavior with agitation and combativeness) are compatible with clinical aspects of rabies. Although this patient did not have classic symptoms such as laryngeal spasms (manifested as hydrophobia) or autonomic instability, the lack of such symptoms has been documented in other rabies patients (1,2,6). Finally, despite an extensive medical workup, no alternate infectious etiology was identified for the patient's neurologic symptoms, increased intracranial pressure, and CSF pleocytosis.
In animal models, both cellular and humoral immune responses are important indicators in survivorship after rabies virus infection (7--9). In this report, the patient's serologic profile suggests that her immune system cleared the rabies virus before production of VNA. This might help explain the patient's atypical (i.e., waxing and waning) neurologic course. In more typical rabies cases, infected persons who have not received rabies PEP experience a rapid neurologic decline, resulting in death. Human survivors of rabies have demonstrated a vigorous immune response to the virus, as measured by serum and CSF antibody levels (2,4). However, CSF IgG in the patient in this report never exceeded a dilution of 1:32, with serum IgG reaching 1:8192, not nearly as high as values reported in previous survivors (1). Another patient, given experimental treatment, showed evidence for neurologic recovery, with high serum but low CSF VNA, but died shortly after therapy (10).
Detection of viral antibodies in serum can be indicative of previous vaccination or exposure to a lyssavirus, but does not necessarily indicate the development of disease. Contact with virus does not ultimately constitute a productive infection (e.g., the virus can be inactivated by the host innate response or by other means before replication in host cells). Similarly, a productive infection does not necessarily result in transportation of virus to the CNS. An abortive infection can occur outside the CNS, with limited replication of the virus at the exposure site and further clearance by the host immune system (7,8).
Rabies virus is a highly neurotropic pathogen, transported from the exposure site to the CNS by peripheral nerves without significant local replication and avoiding or impairing the host immune response during the incubation period. Thereafter, when the virus reaches higher concentrations in the CNS and spreads peripherally, specific antibodies can be detected as the clinical course evolves. Typically, the detection of specific virus antibodies in the CSF indicates a CNS infection. Based on evidence to date with U.S. rabies patients, antibodies to the abundant viral nucleocapsid antigens detected by IFA are registered first, whereas VNA, directed to the outer viral glycoprotein, are only detected later by RFFIT, if VNA are detected at all. The patient described in this report did not have detectable rabies VNA in the serum until after receiving rabies vaccine and HRIG.
In all previous human survivors, rabies was diagnosed based on exposure histories, compatible clinical symptoms, and detection of rabies virus antibodies. However, in all of those patients, the clinical courses were substantially longer, with more severe neurologic compromise and more prominent stimulation of the immune system, including the induction of VNA. In the case presented here, the clinical manifestation was relatively mild, which might imply variables associated with viral dose, route, and type, with a more limited virus replication and less apparent stimulation of the immune system. Clinicians treating possible cases of human rabies, indicated by acute, progressive infectious encephalitis, a compatible exposure history, and serologic evidence of a specific lyssavirus response, even in the absence of detectable VNA or fulminant neurologic decline, should contact their state health department for engagement with CDC.
Acknowledgments
This report is based, in part, on contributions by J Murphy, PhD, I Butler, MD, C Dreyer, MD, B Aalbers, MD, Univ of Texas School of Medicine; R Arafat, MD, Office of Surveillance and Public Health Preparedness, D Persse, MD, Houston Dept of Health and Human Svcs; P Grunenwald, DVM, Texas Dept of State Health Svcs, Region 6/5 South; C Kilborn, MPH, Harris County Public Health and Environmental Svcs, Houston; T Sidwa, DVM, Texas Dept of State Health Svcs, Austin, Texas; J Blanton, MPH, R Franka, DVM, PhD, M Niezgoda, MS, L Orciari, MS, A Velasco-Villa, PhD, X Wu, DVM, PhD, and P Yager, Div of Viral and Rickettsial Diseases, National Center for Emerging and Zoonotic Diseases, CDC.
References
- Willoughby RE, Tieves KS, Hoffman GM, et al. Survival after treatment of rabies with induction of coma. N Engl J Med 2005;352:2508--14.
- Hattwick MA, Weis TT, Stechschulte CJ, Baer GM, Gregg MB. Recovery from rabies: a case report. Ann Intern Med 1972;76:931--42.
- Jackson AC, Warrell MJ, Rupprecht CE, et al. Management of rabies in humans. Clin Infect Dis 2003;36:60--3.
- CDC. Human rabies prevention---United States, 2008: recommendations of the Advisory Committee on Immunization Practices. MMWR 2008;57(No. RR-3).
- Calisher CH, Karabatsos N, Zeller H, et al. Antigenic relationships among rhabdoviruses from vertebrates and hematophagous arthropods. Intervirology 1989;30:241--57.
- World Health Organization. WHO expert consultation on rabies: first report. WHO Technical Report Series 931. Geneva, Switzerland: World Health Organization; 2005. Available at http://www.who.int/rabies/trs931_%2006_05.pdf. Accessed February 22, 2010.
- Lodmell DL, Ewalt LC. Pathogenesis of street rabies virus infections in resistant and susceptible strains of mice. J Virol 1985;55:788--95.
- Bell JF. Abortive rabies infection: experimental production in white mice and general discussion. J Infect Dis 1964;114:249--57.
- Perry LL, Lodmell DL. Role of CD4 and CD8 T cells in murine resistance to street rabies virus. J Virol 1991;65:3429--34.
- Rubin J, David D, Willoughby RE, Jr., et al. Applying the Milwaukee Protocol to treat canine rabies in Equatorial Guinea. Scand J Infect Dis 2009;41:372--5.
What is already known on this topic?
Only six human rabies survivors have been well documented after clinical onset, and none of the survivors had abortive rabies (i.e., recovery without intensive care).
What is added by this report?
This is the first reported case in which certain clinical and serologic findings indicate abortive human rabies and in which, despite an extensive medical investigation, no alternate etiology for the illness was determined.
What are the implications for public health practice?
Clinicians treating possible human rabies, indicated by acute, progressive infectious encephalitis, a compatible exposure history, and serologic evidence of a specific lyssavirus response, should contact their state health department for engagement with CDC; public education should continue to stress the importance of avoiding exposure to bats and seeking prompt medical attention after exposure to any potentially rabid animals.
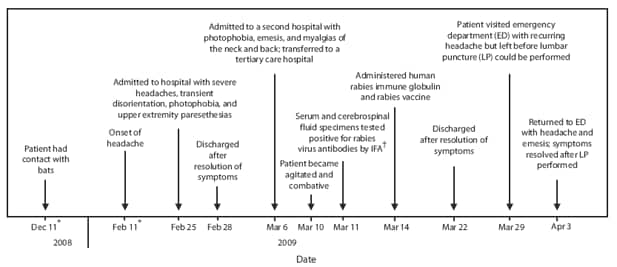
* Approximate date.
† Indirect fluorescent antibody.
Alternate Text: The figure above shows the timeline of course for a patient with presumptive abortive human rabies in Texas in 2009. On February 25, 2009, an adolescent girl aged 17 years went to a community hospital emergency department with severe frontal headache, photophobia, emesis, neck pain, dizziness, and paresthesia of face and forearms. The headaches had begun approximately 2 weeks before she went to the hospital.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


