Candida infections of the mouth, throat, and esophagus
About
Candidiasis is an infection caused by a yeast (a type of fungus) called Candida. Candida normally lives on the skin and inside the body, in places such as the mouth, throat, gut, and vagina, without causing any problems.1 Sometimes, Candida can multiply and cause an infection if the environment inside the mouth, throat, or esophagus changes in a way that encourages fungal growth.
Candidiasis in the mouth and throat is also called thrush or oropharyngeal candidiasis. Candidiasis in the esophagus (the tube that connects the throat to the stomach) is called esophageal candidiasis or Candida esophagitis. Esophageal candidiasis is one of the most common infections in people living with HIV/AIDS.2
Symptoms
Candidiasis in the mouth and throat can have many different symptoms, including:
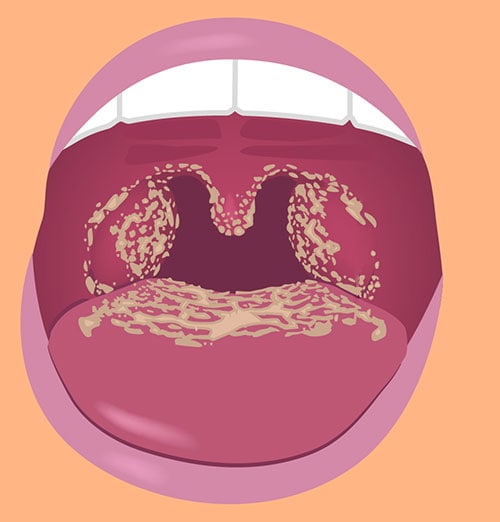
- White patches on the inner cheeks, tongue, roof of the mouth, and throat (photo showing candidiasis in the mouth)
- Redness or soreness
- Cotton-like feeling in the mouth
- Loss of taste
- Pain while eating or swallowing
- Cracking and redness at the corners of the mouth
Symptoms of candidiasis in the esophagus usually include pain when swallowing and difficulty swallowing.
Contact your healthcare provider if you have symptoms that you think are related to candidiasis in the mouth, throat, or esophagus.
Risk and Prevention
Who gets candidiasis in the mouth or throat?
Candidiasis in the mouth, throat, or esophagus is uncommon in healthy adults. People who are at higher risk for getting candidiasis in the mouth and throat include babies, especially those younger than 1 month of age, and people with at least one of these factors:3-7
- Wear dentures
- Have diabetes
- Have cancer
- Have HIV/AIDS
- Take antibiotics or corticosteroids, including inhaled corticosteroids for conditions like asthma
- Take medications that cause dry mouth or have medical conditions that cause dry mouth
- Smoke
Most people who get candidiasis in the esophagus have weakened immune systems, meaning that their bodies don’t fight infections well. This includes people living with HIV/AIDS and people who have blood cancers such as leukemia and lymphoma. People who get candidiasis in the esophagus often also have candidiasis in the mouth and throat.
How can I prevent candidiasis in the mouth or throat?
Ways to help prevent candidiasis in the mouth and throat include:
- Maintain good oral health
- Rinse your mouth or brush your teeth after using inhaled corticosteroids
Sources
Candida normally lives in the mouth, throat, and the rest of the digestive tract without causing any problems. Sometimes, Candida can multiply and cause an infection if the environment inside the mouth, throat, or esophagus changes in a way that encourages its growth.
This can happen when:
- a person’s immune system becomes weakened,
- if antibiotics affect the natural balance of microbes in the body,
- or for a variety of other reasons in other groups of people.
Diagnosis and Testing
Healthcare providers can usually diagnose candidiasis in the mouth or throat simply by looking inside.8 Sometimes a healthcare provider will take a small sample from the mouth or throat. The sample is sent to a laboratory for testing, usually to be examined under a microscope.
Healthcare providers usually diagnose candidiasis in the esophagus by doing an endoscopy. An endoscopy is a procedure to examine the digestive tract using a tube with a light and a camera. A healthcare provider might prescribe antifungal medicine without doing an endoscopy to see if the patient’s symptoms get better.
Treatment
Candidiasis in the mouth, throat, or esophagus is usually treated with antifungal medicine.6 The treatment for mild to moderate infections in the mouth or throat is usually an antifungal medicine applied to the inside of the mouth for 7 to 14 days. These medications include clotrimazole, miconazole, or nystatin. For severe infections, the most common treatment is fluconazole (an antifungal medication) taken by mouth or through a vein. If patient does not get better after taking fluconazole, healthcare providers may prescribe a different antifungal. The treatment for candidiasis in the esophagus is usually fluconazole. Other types of prescription antifungal medicines can also be used for people who can’t take fluconazole or who don’t get better after taking fluconazole.
If you are a healthcare provider, click here to see the Infectious Diseases Society of America’s Clinical Practice Guidelines for the Management of CandidiasisExternalexternal icon.
Statistics
The exact number of cases of candidiasis in the mouth, throat, and esophagus in the United States is difficult to determine. This is because there is no national surveillance for these infections. The risk of these infections varies based on the presence of certain underlying medical conditions. For example, candidiasis in the mouth, throat, or esophagus is uncommon in healthy adults. However, they are some of the most common infections in people living with HIV/AIDS.2 In one study, about one-third of patients with advanced HIV infection had candidiasis in the mouth and throat.9
- CDC – Oral Health
- CDC – Dental Hygiene
- CDC – Opportunistic infections
- Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescentsexternal icon
- Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Childrenexternal icon
- Nucci M, Anaissie E. Revisiting the source of candidemia: skin or gut?external icon Clin Infect Dis . 2001;33:195 9-67.
- Buchacz K, Lau B, Jing Y, Bosch R, Abraham AG, Gil MJ, et al. Incidence of AIDS-defining opportunistic infections in a multicohort analysis of HIV-infected persons in the United States and Canada, 2000-2010external icon. J Infect Dis. 2016;214:862-72.
- Epstein JB, Polsky B. Oropharyngeal candidiasis: a review of its clinical spectrum and current therapiesexternal icon. Clin Ther 1998;20:40-57.
- Lynch DP. Oral candidiasis. History, classification, and clinical presentation.external icon Oral Surg Oral Med Oral Pathol 1994;78:189-93.c.
- Pankhurst CL. Candidiasis (oropharyngeal)external icon. BMJ Clin Evid 2013;2013:1304.
- Pappas PG, Kauffman CA, Andes DR, Clark CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of Americaexternal icon. Clin Infect Dis 2016;62:e1-50.
- Lalla RV, Latortue MC, Hong CH, Ariyawardana A, D’Amato-Palumbo S, Fischer DJ, et al. A systematic review of oral fungal infections in patients receiving cancer therapyexternal icon. Support Care Cancer 2010;18:985-92.
- Coronado-Castellote L, Jimenez-Soriano Y. Clinical and microbiological diagnosis of oral candidiasisexternal icon. J Clin Exp Dent 2013;5:e279-86.
- Thompson GR, 3rd, Patel PK, Kirkpatrick WR, Westbrook SD, Berg D, Erlandsen J, et al. Oropharyngeal candidiasis in the era of antiretroviral therapyexternal icon. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:488-95.