Health Care Personnel and Flu Vaccination, Internet Panel Survey, United States, November 2015
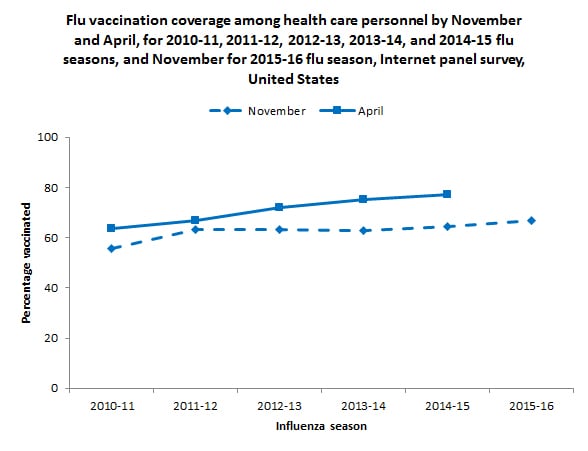
Figure 1.
Influenza (flu) among health care personnel (HCP) can result in lost work days for HCP and has the potential to spread flu to other HCP and to patients (1-5), including pregnant women, young children, older people, and those with medical conditions who are at higher risk of serious flu complications.
- Flu vaccination of HCP has been shown to reduce the risk of flu and absenteeism in vaccinated HCP and reduce the risk of respiratory illness and deaths in nursing home residents (2–5).
- The Advisory Committee on Immunization Practices (ACIP) recommends that all HCP receive an annual flu vaccination (1).
- Flu vaccination coverage among HCP has improved, but remains below the national Healthy People 2020 target of 90% (6).
- In the 2007–08 flu season, HCP vaccination coverage was 48% based on data from the National Health Interview Survey (NHIS), the data source used to monitor the Healthy People 2020 objective (7).
- By the 2013–14 flu season, vaccination coverage among HCP measured in the NHIS had increased to 65% (CDC, unpublished data).
- Flu vaccination coverage among HCP measured using Internet panel surveys* was 67% during the 2011–12 season, 72% during the 2012–13 season, 75% during the 2013–14 season, and 77% during the 2014-15 season (7, 8). In the most recent two flu seasons, coverage among HCP working in hospitals and coverage among doctors, nurses, and pharmacists has approached and sometimes exceeded 90% (8).
CDC analyzed data from an Internet panel survey conducted among HCP from October 29–November 13, 2015. The results of this survey provide information for use in vaccination campaigns during National Influenza Vaccination Week 2015 (December 6–12, 2015). This report provides early flu season (early November) estimates of vaccination coverage among HCP. Final 2015–16 flu season HCP vaccination coverage estimates will be available after the end of the season.
Key Findings
- Early season 2015–16 flu vaccination coverage among HCP was 66.7%, similar to early season coverage during the 2014–15 season (64.3%).
- During the previous two seasons, flu vaccination coverage increased by 12–13 percentage points from early season to the end of the season.
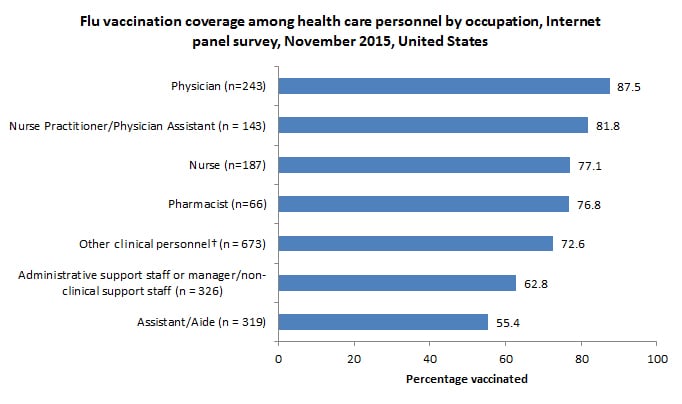
- By occupation, early season flu vaccination coverage was highest among physicians (87.5%), nurse practitioners/physician assistants (81.8%), nurses (77.1%), pharmacists (76.8%), and other clinical professionals (72.6%).
- Flu vaccination coverage was lowest among administrative and non-clinical support staff (62.8%) and assistants and aides (55.4%).
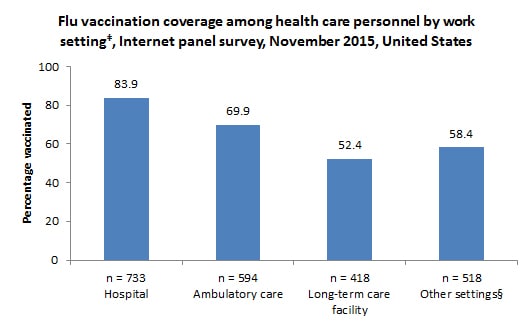
- By work setting, early season flu vaccination coverage was highest among HCP working in hospitals (83.9%).
- Flu vaccination coverage was lowest among HCP working in long-term care (LTC) settings (52.4%).
- Early season flu vaccination coverage was higher among HCP whose employers required (87.2%) or recommended (61.9%) that they be vaccinated compared with those HCP whose employer did not have a requirement or a recommendation regarding flu vaccination (39.4%).
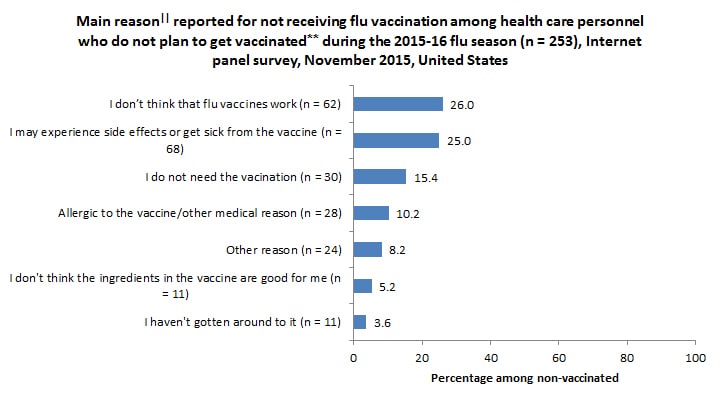
- Among unvaccinated HCP who did not intend to get the flu vaccination during this flu season, the most common reason reported for not getting vaccinated was that they don’t think that flu vaccines work. The second most common reason was fear of experiencing side effects or getting sick from the vaccine.
Conclusions/Recommendations:
- Vaccination continues to be low among assistants, aides, non-clinical support staff, and HCP working in LTC settings.
- While overall end-of-season HCP flu vaccination has steadily improved over the last five years, most of these increases have occurred in hospital settings.
- Increased efforts are needed to improve coverage among these HCP groups with lower coverage, especially those working in LTC settings where residents are often at higher risk of severe complications from flu.
- The highest vaccination coverage was reported among HCP with an employer requirement for vaccination.
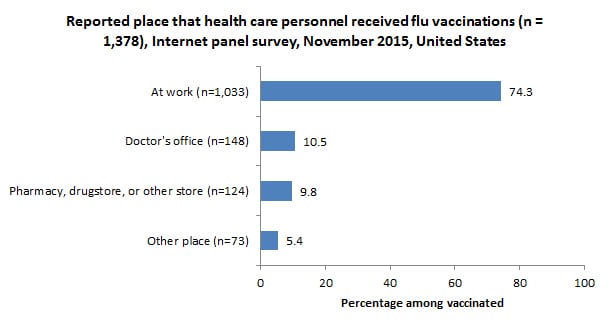
- In the absence of vaccination requirements, evidence-based measures associated with increased flu vaccination coverage of HCP include ensuring convenient access to flu vaccine at the workplace at no cost.
Who Was Vaccinated?
Coverage by Occupation
- Early season flu vaccination coverage was higher among physicians (87.5%), nurse practitioners and physician assistants (81.8%), nurses (77.1%), pharmacists (76.8%), and other clinical personnel (72.6%) compared with administrative/non-clinical support staff (62.8%) and assistants or aides (55.4%).
- Flu vaccination coverage increased from early season 2014–15 to early season 2015–16 by 8.8 percentage points among assistants and aides and by 5.3 percentage points among physicians. Flu vaccination coverage decreased from early season 2014–15 to early season 2015–16 by 9.9 percentage points among pharmacists. Coverage for other occupational groups was similar in early season 2014–15 and early season 2015–16.
Coverage by Work Setting
- Early season flu vaccination coverage varied by work setting and was highest among HCP working in hospitals (83.9%) and lowest among HCP working in long-term care settings (52.4%).
- Coverage among HCP working in hospitals increased by 5.2 percentage points from early season 2014–15 to early season 2015–16. Coverage in all other work settings was similar in early season 2014–15 and early season 2015–16.
Coverage by Employer Requirement or Recommendation
- Early season flu vaccination coverage was highest among HCP with an employer requirement for vaccination (87.2%). Vaccination coverage was higher among HCP with an employer recommendation for vaccination but no requirement (61.9%) compared to those whose employers had neither a requirement nor a recommendation for vaccination (39.4%).
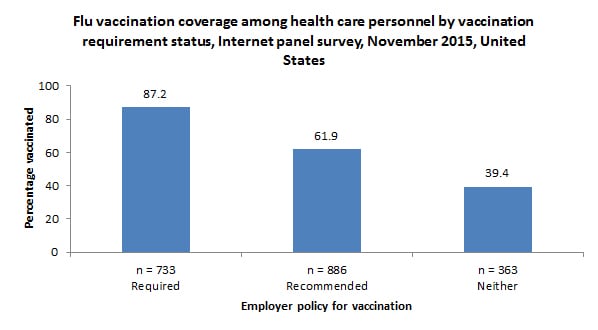
- HCP working in hospitals were more likely to report an employer requirement for vaccination than HCP working in ambulatory care, long-term care settings, and other settings (Table 1).
|
Percentage vaccinated among HCP with and without an employer requirement for vaccination |
||||
|---|---|---|---|---|
|
Percentage of HCP with an employer requirement for vaccination |
Required |
Not required |
||
|
Unweighted n |
Weighted % |
Weighted % |
Weighted % |
|
| Hospital |
468 |
60.7 |
88.9 |
76.2 |
| Ambulatory care / Physician office |
224 |
33.7 |
90.8 |
59.2 |
| Long-term care facility |
98 |
20.6 |
76.2 |
46.2 |
| Other setting§ |
103 |
23.3 |
89.7 |
48.9 |
| Total |
733 |
36.6 |
87.2 |
55.0 |
Main Reason for Not Receiving Vaccination
- Among unvaccinated HCP who reported that they do not intend to get flu vaccination during this flu season, the most commonly reported main reason¶ was that they do not think that flu vaccines work.
- This was also the most commonly reported reason for non-vaccination in early season 2014-15.
- Other reasons commonly reported for not receiving flu vaccination included fear of side effects or getting sick from the vaccine and thinking that they do not need the vaccine.
What Can Be Done? (Recommendations)
Overall, the early season estimate of flu vaccination coverage among HCP in 2015–16 (66.7%) was similar to early season coverage in 2014–15 (64.3%). Flu vaccination coverage among HCP working in hospital settings, and among physicians, nurse practitioners, physician assistants, nurses, pharmacists and other clinical personnel across all work settings was substantially higher than coverage among HCP working in long-term care and other work settings and among HCP working in other occupations. The success of onsite vaccination and other vaccine promotion in raising coverage in hospital settings could be implemented in other work settings with lower coverage.
Additional efforts are needed to improve vaccination coverage among HCP in work settings other than hospitals, especially in long-term care settings, and among assistants and aides and administrative and non-clinical support staff in all work settings. Continued efforts are needed to ensure all HCP are vaccinated as soon as possible during every flu season. Interventions to promote flu vaccination among HCP each season include:
- Employers should offer flu vaccination to HCP:
-
- Onsite over multiple days and shifts,
- Free of charge, and with
- Active promotion.
-
- Employers and health care administrators should make use of the Guide to Community Preventive Services, which provides guidance on effective interventions to increase the uptake of flu vaccination among HCP (9).
- Long-term care (LTC) employers can also use the LTC web-based toolkit developed by CDC and the National Vaccine Program Office, which provides access to resources, strategies, and educational materials for increasing flu vaccination among HCP in LTC settings (10).
- Measurement and feedback of vaccination coverage is recommended by the Community Preventive Services Task Force to increase uptake of recommended vaccinations (9). Measures such as recent requirements by the U.S. Centers for Medicare & Medicaid Services (CMS) for acute care hospitals, ambulatory surgery centers, and outpatient dialysis facilities to report their facilities’ HCP influenza vaccine coverage rates may be useful for this purpose (11-14).
The November internet panel survey of HCP is designed to provide estimates of national flu vaccination coverage among HCP and to assess the effectiveness of current vaccination efforts. The follow-up survey will be conducted in April 2016 to provide end-of-season flu vaccination coverage estimates.
Data Source and Methods
CDC collected data from two pre-existing web-based panels from October 28–November 13, 2015. Professional clinical personnel (physicians, nurse practitioners, physician assistants, nurses, dentists, pharmacists, allied health professionals, technicians, technologists, emergency medical technicians, and paramedics) were recruited from the membership of Medscape, a professional health website managed by WebMD Professional Services. HCP in other occupations (assistants, aides, administrative support staff and managers, and non-clinical support staff employed in health care work settings) were recruited from a general population Internet panel operated by Survey Sampling International. The sample was weighted to reflect the demographic composition of the target population of U.S. HCP. Survey items included vaccination during the current flu season, vaccination history, and knowledge, attitudes, and beliefs concerning flu and flu vaccination. There were 2,033 eligible HCP who started the survey, and 1,982 (97.5%) of those completed the survey. Weighted estimates were calculated based on each occupational group by age, gender, race/ethnicity, health care work setting, and Census region to be generalizable to the U.S. population of HCP.
Weighted analyses were conducted using SAS v9.2 survey procedures. Because the opt-in Internet panel sample is based on those who self-selected for participation in the panels rather than a random probability sample, statistical measures such as calculation of confidence intervals and tests of differences cannot be performed (15). A change was noted as an increase or decrease when there was a difference in estimates of at least five percentage points.
Sample Demographics
- A total of 1,982 HCP were included in the survey.
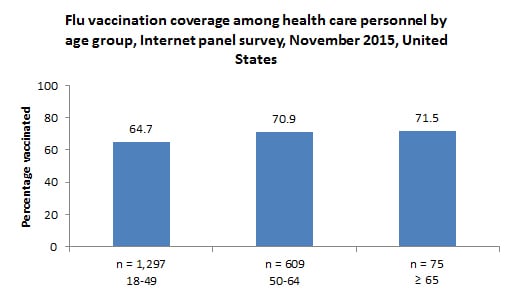
- By age††, 1,297 (65.5%) were 18–49 years, 609 (30.7%) were 50–64 years, and 75 (3.8%) were 65 years and older.
- For additional occupational characteristics, please see the attached table. hcp-occupation-2015.xlsx [XLSX – 17 KB]
- For additional work setting characteristics, please see the attached table. hcp-worksetting-2015.xlsx [XLSX – 17 KB]
Limitations
These results are preliminary and should be interpreted with caution. The follow-up survey in April 2016 will assess flu vaccination coverage at the end of the flu season.
The findings in the report are subject to several limitations.
- The sample was not necessarily representative of the approximately 18 million HCP in the United States. The survey was conducted among a group of volunteer HCP (a non-probability sample) who had already enrolled in Medscape or the Survey Sampling International panel, rather than among a randomly selected sample.
- Some bias might remain in estimates after weighting the sample to improve representativeness, given the exclusion of individuals with no Internet access and the self-selection processes for entry into the panels and participation in the survey. Estimates might be biased if the selection processes for entry into the Internet panels and the decision to participate in this particular survey were related to receipt of vaccination.
- All vaccination results are based on self-report and are not verified by employment or medical records.
- The definition of HCP used in this Internet panel survey (persons who worked in a health care setting) might vary from definitions used in other surveys of vaccination coverage.
- Occupational categories could not always be separated because of small sample sizes, questionnaire design, or other limitations.
- The 2015–16 estimates from this survey might not be directly comparable to estimates from population-based surveys.
- The estimates of flu vaccination coverage among HCP from the Internet panel surveys and the NHIS differed for the 2009-10 (63.4% versus 57.5%), 2010–11 (63.5% versus 55.8%), 2011-12 (66.9% versus 62.4%), 2012-13 (72.0% versus 66.9%), and 2013-14 (75.2% versus 64.9%) seasons (7; CDC, unpublished data).
Despite these limitations, Internet panel surveys are a useful surveillance tool for timely early season and post-season evaluation of flu vaccination coverage and vaccination-related knowledge, attitude, practice, and barrier data among HCP. Top of Page Authors: Carla L. Black, PhD1; Xin Yue, MPS, MS2; Sara M.A. Donahue, DrPH, MPH3; Sarah W. Ball, ScD, MPH3; David Izrael, MS3; Peng-Jun Lu, MD, PhD1; Walter W. Williams, MD, MPH1; Samuel B. Graitcer, MD1; Carolyn B. Bridges, MD1; Megan C. Lindley, MPH1; Marie A. de Perio, MD4 1Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; 2Leidos, Atlanta, GA; 3Abt Associates Inc., Cambridge, MA; 4Division of Surveillance, Hazard Evaluations, and Field Studies, National Institute for Occupational Safety and Health, CDC
Related Links
- FluVaxView Influenza Vaccination Coverage
- 2014-15 end-of-season MMWR
- 2014-15 early season online report
- 2013–14 end-of-season MMWR
- 2013-14 early season online report
- 2012–13 end-of-season MMWR
- 2012–13 early season online report
- 2011–12 end-of-season MMWR
- 2011–12 early season online report
- 2010–2011 end-of-season MMWR
- 2010–2011 early season online report [326 KB, 5 pages]
- ACIP flu vaccination recommendations for health care personnel
- Flu.gov for Health Professionals
- Influenza Vaccination Information for Health Care Workers
- NIVW Resources for Health Professionals and Partners
- CDC toolkit for increasing influenza vaccination among health care personnel in long-term care settings
- SSI Data Solutions and Technology
- SurveySpot
- Follow CDC Flu on Twitter: @CDCFlu
References/Resources
- CDC. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(No. RR-7).
- Saxen H, Virtanen M. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of healthcare workers. Pediatr Infect Dis J. 1999; 18:779-83.
- Oshitani H, Saito R, Seki N, et al. Influenza vaccination levels and influenza-like illness in long-term care facilities for elderly people in Niigata, Japan, during an Influenza A (H3N2) epidemic. Infect Control Hosp Epidemiol 2000;21:728-30.
- Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ 2006;333:1241.
- Lemaitre M, Meret T, Rothan-Tondeur M, et al. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc. 2009; 57:1580-1586
- HealthyPeople.gov. Immunization and Infectious Diseases. Available at https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed November 9, 2015.
- CDC. Surveillance of influenza vaccination coverage – United States, 2007-08 through 2011-12 influenza seasons. MMWR Surveill Summ 2013;62(No. SS-04):1-29.
- Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel—United States, 2014-15 influenza season. MMWR Morb Mortal Wkly Rep 2015;64:993-9.
- Community Preventive Services Task Force. Interventions to promote seasonal influenza vaccination among healthcare workers. Available at http://www.thecommunityguide.org/worksite/flu-hcw.html. Accessed November 9, 2015.
- CDC. A toolkit for long-term care employers: increasing influenza vaccination among health care personnel in long-term care settings. Available at https://www.cdc.gov/flu/toolkit/long-term-care/index.htm. Accessed November 9, 2015.
- U.S. Department of Health and Human Services. Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and FY2012 rates; hospitals’ FTE resident caps for graduate medical education payment; final rules. Fed Regist 2011;76:1631-3.
- Lindley MC, Bridges CB, Strikas RA, et al. Influenza vaccination performance measurement among acute care hospital-based health care personnel—United States, 2013-14 influenza season. MMWR 2014;63:812-5.
- U.S. Department of Health and Human Services. Medicare and Medicaid programs; hospital outpatient prospective payment; ambulatory surgical center payment; hospital value-based purchasing program; physician self-referral; and patient notification requirements in provider agreements; final rules. Fed Regist 2011;76:74470-2.
- U.S. Department of Health and Human Services. Medicare Program; end–stage renal disease prospective payment system quality incentive program and durable medical equipment, prosthetics, orthotics, and supplies; final rule. Fed Regist 2014;79:66206-8.
- American Association for Public Opinion Research. Report of the AAPOR Task Force on non-probability sampling. Available at http://www.aapor.org/AAPORKentico/AAPOR_Main/media/MainSiteFiles/NPS_TF_Report_Final_7_revised_FNL_6_22_13.pdf. Accessed November 9, 2015.
Footnotes
* The methods used in the Internet panel survey differ from those of the NHIS; thus, results from the Internet panel survey should not be directly compared to the Healthy People 2020 target.
† Includes allied health professionals, dentists, technicians, technologists, emergency technicians, EMTs, and paramedics.
‡ Respondents could specify working in more than one setting.
§ Includes dental offices, pharmacies, emergency medical services locations, and other health care settings.
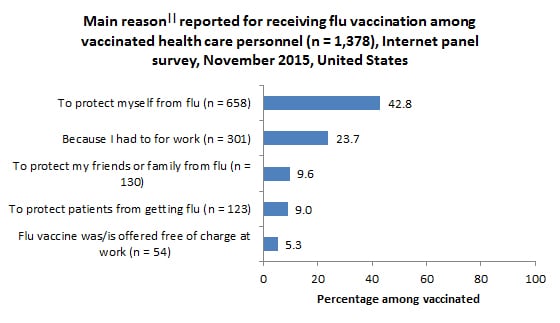
|| Single main reason.
¶ Among respondents, 30.8% initially selected “I just don’t want the vaccine” as their main reason for not being vaccinated. When these persons were asked in a follow-up question to identify a more specific reason for not wanting the vaccine, 33.6% replied “I don’t need it,” 29.9% said “I don’t think the ingredients in the vaccine are good for you,” 21.8% said “I don’t think that flu vaccines work,” and 14.7% said “I might get sick from the vaccine.”
** Includes respondents who have not received the flu vaccine since July 2015 and who reported that they probably or definitely do not intend to be vaccinated in the 2015–16 flu season. †† One respondent was missing information for age.