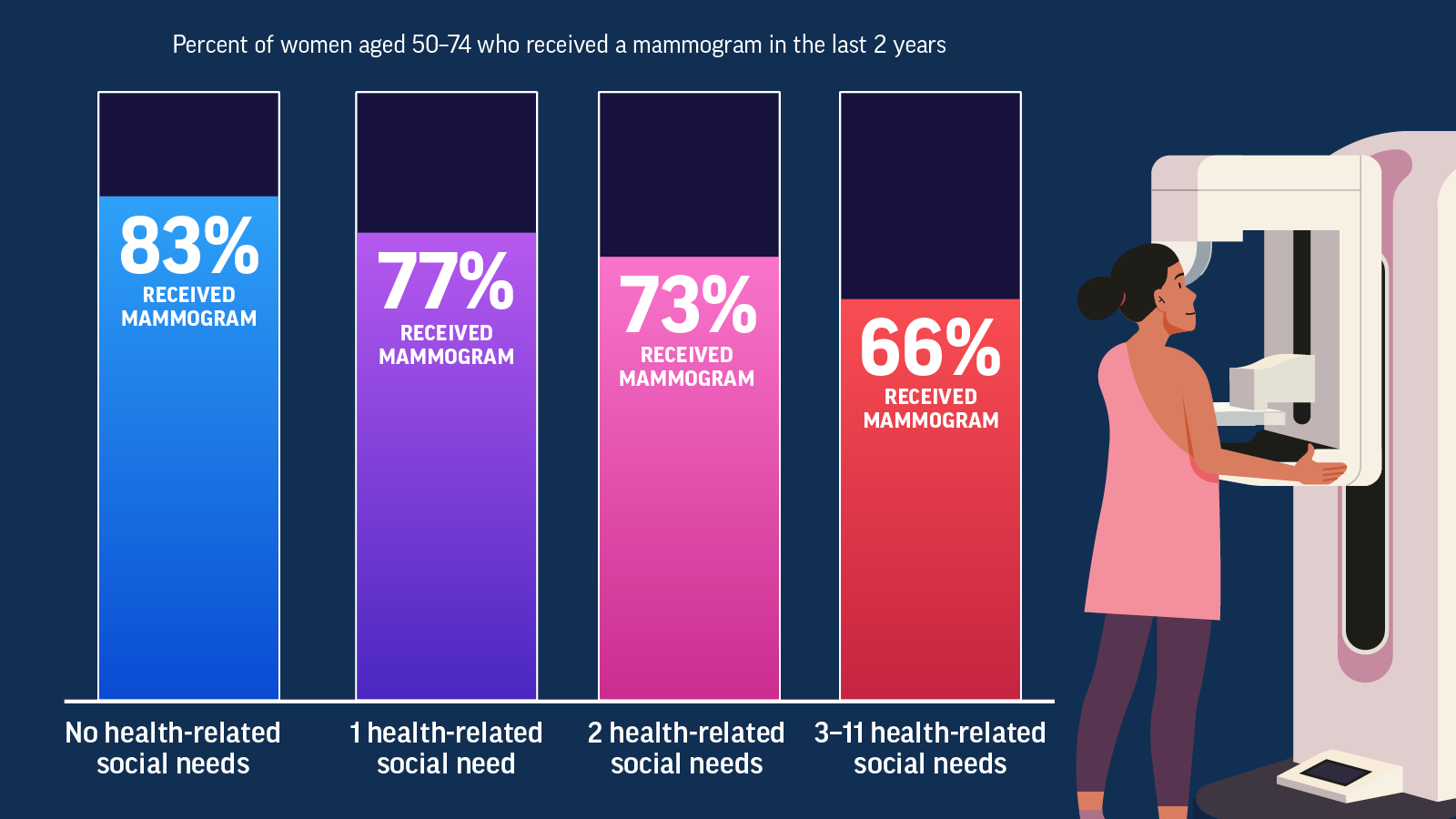
Only about 3 in 4 women ages 50 to 74 years were up to date with their mammograms in 2022. More women need to get screening mammograms that can save lives.
- Health-related social needs can have an impact on a woman’s chance of being up to date with her mammogram. For example, women are less likely to get a mammogram if they feel socially isolated, have lost a job, or don’t have reliable transportation. The more health-related social needs a woman has, the less likely she is to have a mammogram. Only about 7 in 10 women ages 50 to 74 years with three or more health-related social needs were up to date with mammograms, compared to about 8 in 10 of those with no health-related social needs.
- The cost of accessing health care was the greatest challenge for women who did not receive a mammogram in the past 2 years.
- Women without health insurance, who had low incomes, and who did not have a usual source of health care were less likely to get mammograms.
Health-related social needs can lower a woman’s chance of being up to date with her mammogram
Women are more likely to get lifesaving mammograms when their health-related social needs are met.
Women who were not experiencing health-related social needs were more likely to receive a mammogram
The more health-related social needs a woman experiences, the less likely she is to receive a mammogram.
Women ages 50 to 74 years who are at average risk for breast cancer should get a screening mammogram every 2 years.
This will help find breast cancer early when treatment works best. Average risk refers to women without a strong family history of breast cancer, without changes in certain breast cancer genes, and who have not had chest radiation.
Women who are 40 to 49 years old should talk to their doctor about when to start and how often to get a mammogram.
Get email updates about Vital Signs
VITAL SIGNS RESOURCES