Traumatic Brain Injury in the United States: Assessing Outcomes in Children
Note: This publication is from 2000 and is included for historical purposes. See the Get the Facts and Data & Statistics pages for the most current data.
- Other TBI Issues
- Appendix A – Overview of Available Outcome Assessments
- Appendix B – Slides from Expert Group Presentation
- Appendix C – Data from the South Carolina Surveillance System
- Appendix D – Other Resources to Guide Selection of Research Topics
- Appendix E – Overview of TBI Surveillance Activities Funded by the CDC
Preface
Summary and Recommendations from the Expert Working Group
Atlanta, GA
October 26-27, 2000
Editor
Jean A. Langlois, Sc.D., M.P.H.
Epidemiologist
Division of Acute Care, Rehabilitation Research
and Disability Prevention,
National Center for Injury Prevention and Control
Department of Health and Human Services
Centers for Disease Control and Prevention
This report is a publication of the
National Center for Injury Prevention and Control
of the Centers for Disease Control and Prevention.
Centers for Disease Control and Prevention
Jeffrey P. Koplan, M.D., M.P.H., Director
National Center for Injury Prevention and Control
Sue Binder, M.D., Director
Division of Acute Care, Rehabilitation Research and Disability Prevention
Daniel Pollock, M.D., Acting Director
Acknowledgments
The editor wishes to acknowledge the valuable contributions of the following people to the meeting on Assessing Outcomes of Traumatic Brain Injury In Children and Youth and the preparation of this report: Shanthi Ameratunga, Patricia Allen, Allan Bergman, Doug Browne, Victor Coronado, Karen Gotsch, Melissa McCarthy, Jane McDonald, Audrey Reichard, Virginia Ross, Anbesaw Selassie, David Thurman and the staff of the Office of Communication Resources, the National Center for Injury Prevention and Control.
Sincere thanks also go to the Maternal and Child Health Bureau, the Health Resources and Services Administration for distributing this report through its National Maternal and Child Health Clearinghouse.
Group Participants
Shanthi Ameratunga, MB.Ch.B., M.P.H., F.R.A.C.P.
Senior Research Fellow
Department of Community Health
Faculty of Medicine and Health Science
The University of Auckland
Auckland, New Zealand
Allan Bergman
President and CEO
The Brain Injury Association, Inc.
Alexandria, Virginia
Nancy Carney, Ph.D.
Assistant Professor
Department of Emergency Medicine
School of Medicine
Oregon Health Sciences University
Director, Oregon Traumatic Brain Injury Model System Project
Portland, Oregon
Jeanne Dise-Lewis, Ph.D.
Associate Professor
University of Colorado Medical School
Director of Psychology Services,
Department of Rehabilitation Medicine
The Children’s Hospital
Denver, Colorado
Arlene Greenspan, Dr.P.H., P.T.
Assistant Professor
Center for Rehabilitation Medicine
Emory University School of Medicine
Atlanta, Georgia
Stephen M. Haley, Ph.D., P.T.
Director
Center for Rehabilitation Effectiveness
Sargent College of Health and Rehabilitation Sciences
Boston University
Boston, Massachusetts
Jeanne M. Landgraf, M.A.
Co-Founder, Vice President and Chief Scientific Officer
HealthAct and outcomesPro.com
Boston, Massachusetts
Jean A. Langlois, Sc.D., M.P.H. (moderator)
Epidemiologist
Division of Acute Care, Rehabilitation Research and Disability Prevention
National Center for Injury Prevention and Control
Centers for Disease Control and Prevention
Atlanta, Georgia
Melissa McCarthy, Sc.D.
Assistant Professor
Department of Emergency Medicine
Johns Hopkins University School of Medicine
Baltimore, Maryland
Terrie Price, Ph.D.
Director
Neuropsychology and Social Services
The Rehabilitation Institute of
Kansas City
Kansas City, Missouri
Bonnie Todis, Ph.D.
Associate Professor
Teaching Research
Western Oregon University
Eugene, Oregon
Keith Yeates, Ph.D.
Associate Professor
Department of Pediatrics
College of Medicine and Public Health
The Ohio State University
Columbus, Ohio
Executive Summary
This report summarizes the comments, suggestions, and recommendations of a working group convened by the Centers for Disease Control and Prevention (CDC) on assessment of Traumatic Brain Injury (TBI) outcomes in children and youth. It is intended for researchers, public health professionals—including those from state health departments—and advocates interested in furthering research on outcomes of TBI in children.
TBI is often described as the leading cause of disability in children, but data to support this assertion are lacking. We know that each year an estimated 3,000 children and youth die from TBI; 29,000 are hospitalized; and 400,000 are treated in hospital emergency departments. Currently, no population-based studies of the outcomes of TBI among children and youth exist to provide national estimates of TBI-related disability and document the need for services.
On October 26 and 27, 2000, the National Center for Injury Prevention and Control at the CDC held a meeting of researchers, advocates and other professionals from the U.S. and New Zealand to discuss “Methodological Issues in Assessing Outcomes of TBI in Children and Youth.” The primary purpose of this meeting was to determine the feasibility and appropriate methods for conducting population-based follow-up studies of outcomes of TBI in children and youth.
Meeting participants identified key research topics and variables to measure in assessing longer-term outcomes of TBI in children and youth (ages 0-16 years). They reviewed several conceptual models of disability, including the Institute of Medicine Model and the World Health Organization Model, that could provide a framework for designing appropriate studies of TBI outcomes. They also discussed the advantages and shortcomings of available measures for assessing these outcomes. Finally, the working group described the challenges in designing and implementing studies on TBI in children and youth and recommended ways to address those challenges.
Meeting participants recommended that further research be done to examine physiological responses to brain injury, patterns of recovery and treatment and costs of TBI. The group suggested that the field needs to explore the applicability of various types of research, including qualitative research. Some examples suggested included focus groups and individual interviews. Meeting participants also recommended methods for improving measurement, data analysis and terminology used in the study of TBI.
Background
Methodological Issues in Assessing Outcomes of Traumatic Brain Injury (TBI) in Children and Youth
Purpose of this Report
On October 26 and 27, 2000, the Centers for Disease Control and Prevention (CDC) convened an expert working group to discuss “Methodological Issues in Assessing Outcomes of Traumatic Brain Injury in Children and Adolescents.” This report documents the comments and suggestions of the working group.
Meeting Goal and Objectives
The goal of the meeting was to determine the feasibility and appropriate methods for conducting a population-based follow-up study of outcomes of TBI in children and youth.
The meeting objectives were to
- Identify key domains and variables to measure in assessing longer-term outcomes of TBI in children and youth (ages 0-16 years).
- Discuss the advantages and shortcomings of available measures for assessing these outcomes.
- Highlight the need for other types of research on TBI in children and youth.
- Discuss methodological issues in assessing TBI outcomes in this population.
Meeting Participants and Process
The eleven participants included researchers, advocates, psychologists, educators and other professionals from the United States and New Zealand. With input from the Brain Injury Association, CDC selected invitees for their potential to contribute to a greater understanding of the important outcomes of TBI in children that need to be studied or the methods appropriate for collecting information about those outcomes. Two of the participants are the developers of key measures of health status in children.
For each objective, CDC staff prepared background materials for discussion; selected meeting participants assisted in these preparations. The meeting began with presentations of preliminary CDC multi-state surveillance data and South Carolina surveillance data to provide background information on the importance of TBI among children and youth as a public health problem (See Appendix B and Appendix C). For the remainder of the first day, participants discussed the background materials. A professional note taker recorded participants’ comments and suggestions. On the second day, the moderator presented a synthesis of the suggestions for review and revision by the participants.
This report documents the final summary of the comments and recommendations. For some sections, more detailed definitions, references and other materials have been added to clarify the information from the meeting.
TBI as a Public Health Problem in Young People
Among children and youth aged 0 to 14 years in the U.S.:
Each year traumatic brain injury results in an estimated
- 3,000 deaths
- 29,000 hospitalizations
- 400,000 emergency department visits.*
Unintentional injury is the leading cause of death, and traumatic brain injury is the type of injury most often associated with death.
The annual total of TBI-related deaths is
- More than 6 times the number the number of deaths related to HIV/AIDS*
- 20 times the number of deaths from asthma**
- 38 times the number of deaths from cystic fibrosis.***
* CDC
** NCHS, Monthly Vital Statistics Report. Vol. 45, No. 3 (S), September 30, 1996.)
*** CDC Wonder
TBI is reported to be the leading cause of disability in young people in the U.S., but the evidence is limited. Most studies of the outcomes of TBI in children and youth are based on case series from selected hospitals or rehabilitation facilities, small regional samples or anecdotal reports. Few studies have followed the same group of children over time. (See Appendix B for additional statistics on TBI in children and youth.)
The Need for More Research
Population-based longitudinal studies provide data representative of the long-term outcomes of all children and youth in a defined area who have had a TBI. They are necessary to allow generalization to the U.S. population of children and youth with TBI. Currently no population-based studies of the outcomes of TBI among children and youth exist to provide national estimates of TBI-related disability and to document the need for services.
CDC has funded such studies, referred to as “follow-up studies” or “outcomes surveillance,” of older adolescents and adults (ages 15 years and older) in two states, South Carolina and Colorado. In each of these studies, a sample of people hospitalized with a TBI is identified and given a telephone questionnaire at yearly intervals to find out about TBI outcomes, including disability. For more information about CDC-funded TBI studies, see Appendix E. When the first of these studies was initiated in 1994, children were not included, in part, because few measures were available. The difficulty of measuring the effects of the injury in the context of naturally occurring developmental changes contributes to the challenge of assessing outcomes of TBI in young people.
The Brain Injury Association, the Federal Advisory Committee for Injury Prevention and Control and a wide range of researchers and other professionals in the field have long argued for a population-based follow-up study of outcomes of TBI in children. In its October 2000 reauthorization of the TBI Act of 1996, Congress emphasized the need for CDC to support TBI studies among all age groups. This meeting was conducted to obtain advice regarding the feasibility of conducting a CDC-funded study of TBI outcomes in children and youth.
A Note about Terminology
Child vs. Pediatric: Meeting participants advocated using the term child because pediatric is associated with the medical model. Reference to child encourages consideration of broader, longer-term issues, not only medical concerns. Researchers and professionals should avoid using pediatric especially when referring to longer-term outcomes of TBI in children.
Youth vs. Adolescent: Participants referred to the term youth over teenagers or adolescents because it is more widely used in educational and other settings.
Caregiver vs. Parent: The term caregiver may be more appropriate than parent because in many cases the person caring for the child is someone other than a parent.
Designing Studies that Assess Longer-Term TBI Outcomes in Children and Youth: Conceptual Models, Operational Models and Other Resources
Objective
This section provides background information about selection of a conceptual model and development of an operational model as well as other resources available to help guide the study design.
Conceptual Models
Meeting participants mentioned several conceptual models that could provide a framework for designing appropriate studies of TBI outcomes. It is important to select an appropriate conceptual model before finalizing an operational model and selecting specific measures.
-
Institute of Medicine (IOM) Model
The original IOM model links the four main components of the disabling process–pathology, impairment, functional limitation and disability. The modified IOM model removes disability from this chain to emphasize that disability is not an individual characteristic but a result of interaction between an individual and his or her environment. (Brandt EN Jr., Pope AM, editors. Enabling America: Assessing the Role of Rehabilitation Science and Engineering. Washington, DC: National Academy Press; 1997). -
World Health Organization (WHO) Model (ICIDH-2)
This WHO model of disability addresses both the individual factors, including body systems, impairment, activity, and social participation, and the role of the environment. The model is still under revision and has not yet been adapted for children, although work is in progress. Meeting participants recommended that CDC consider adopting this model, which is being applied to disability research internationally. (ICIDH-2: International Classification of Functioning, Disability, and Health Website. Available at: www.who.int/icidh/. Accessed January 10, 2001; Simeonsson RJ, Lollar D, Hollowell J, Adams M. Revision of the International Classification of Impairments, Disabilities, and Handicaps Developmental Issues. J Clin Epidemiol 2000;53:113-124.) -
Family Systems Model
This model assesses the family environment, including structural dimensions such as family size and family composition, as well as qualitative aspects such as family stressors, sources of internal and external support, and areas of strength and need. (Kalesnik, J. Family assessment. In Nutall EV, Romero I, et al. editors. Assessing and Screening Preschoolers: Psychological and Educational Dimensions (2nd ed.). Boston: Allyn and Bacon, Inc; 1999. pp. 112-125.) -
Developmental Models
A developmental model is a framework that recognizes a wide range of factors including the intricate matrix of a changing child and environment, evolving familial and societal expectations, and the link between disrupted and normal development. (Pynoos RS, Steinberg AM, Wraith R. A developmental model of childhood traumatic stress. In: Cicchetti E, Cohen DJ, editors. Developmental Psychopathology. Vol 2: Risk, Disorder, and Adaptation. Wiley series on personality processes. New York: John Wiley and Sons; 1995. pp. 112-125. Brett AW, and Laatsch L. Cognitive rehabilitation therapy of brain-injured students in a public high school setting. Pediatric Rehabilitation 1998;2:27-31.) Consideration of developmental models is critical in designing studies of longer-term outcomes of TBI in children so that the studies address not only the effects of the injury but also how these effects relate to development.
Models of disability (IOM or WHO) are the most useful as overall guides for the study design. Family systems and developmental models suggest key areas to be considered for inclusion in the study.
Operational Models
Operational models are one-page summaries of topics and variables to consider in planning studies of outcomes of TBI in young people. Meeting participants reviewed and discussed draft operational models, which were prepared before the meeting. Figure 1 (General Model) and Figure 2 (Service-Related Model) show the topics and related variables recommended by the working group.
These topics and variables were suggested by researchers, advocates and professionals. It is also important to conduct qualitative research, such as focus groups, with families and children or youth with TBI to understand the key issues from their perspectives. Minority populations should be included in qualitative studies to increase understanding of the unique experiences and service needs of these subpopulations.
To date, studies have focused largely on determinants of secondary conditions and adverse outcomes, but studies must also be developed to identify factors related to good outcomes.
Other Resources
Meeting participants mentioned several other resources that could be used to guide selection of research priorities. These resources include:
- Healthy People 2010 Health Objectives for children and people with disabilities
- Declarations of children’s rights
- HRSA/Maternal and Child Health Bureau rights of the child
- United Nations Convention on the Rights of the Child.
To read portions of these documents, see Appendix C of this report.
More About the Domains for Assessing Service Needs
Parents and advocates report that appropriate services for children and youth with TBI are lacking. Studies of outcomes of TBI among this population should document the needs for services and the barriers to receiving them. For that reason, meeting participants developed a separate operational model specifically for these issues (Figure 2).
For clarification, a more detailed description of some of the important barriers that were discussed follows below:
- Lack of referrals made by healthcare providers.
- Caregivers not aware of available services.
- Lack of appropriate identification of TBI as the underlying reason for the need for the service or misidentification (e.g., instead of being identified as having a TBI, the child is diagnosed as having a learning disability).
- Lack of appropriate services and service providers with expertise specifically in TBI.
- Lack of insurance or inadequate insurance; e.g., an HMO or PPO may not have appropriate service providers.
- Continuation of pre-injury services; children may tend to receive the same kind of services after the TBI, even if these services are not appropriate for their specific post-TBI problems.
- Lack of acceptance of services because they are not perceived as culturally relevant.
- Lack of appropriate educational services; the Individualized Educational Plan (IEP) does not meet the child / youth’s need or schools may tend to identify conditions they know how to manage. Research is needed to determine whether classifying children as having a TBI affects how they are managed in school.
Figure 1

Figure 2
Available Measures for Assessing Outcomes of TBI in Children and Youth
Objective
This section summarizes existing measures for assessing outcomes and describes their applicability to studies of TBI.
Key Criteria
Meeting participants reviewed key criteria for evaluating the usefulness of currently available measures for assessing outcomes of TBI. These criteria included:
- Developed for use with children and youth
- Because the problems resulting from TBI in children are unique, most measures designed for adults cannot be effectively adapted for children and youth.
- Previously used with children/youth with TBI
- Potentially useful measures that were not developed specifically for this population need to be validated or, at a minimum, pilot-tested first.
- Useful for measuring change during longer-term follow-up
- Some measures have ceiling or floor effects (limitations in their ability to detect more minor or more severe problems, respectively). Ceiling effects in particular may limit the usefulness of a measure to assess changes over time, as recovery occurs. Many measures have only been used to assess status at one point of time; thus, their usefulness for measuring change is not known.
- Norms/comparison data available for other conditions
- Measures with norms for the general population or that have been used to document outcomes associated with other conditions are very useful for determining the effects of TBI.
- Appropriate for the target age group
- Many more measures have been developed for use with school-aged children and youth than for very young children. The majority of measures developed for children aged 5 years or younger are developmental measures not specifically designed for children with TBI. Longitudinal research that applies the appropriate measures at each developmental level, but that also tracks important milestones and late emerging deficits from early childhood through older ages, will be especially challenging.
Specific Measures A wide range of child health and other measures are available. (For tables that summarize the measures, see Appendix A.) However, not all of these measures are useful or appropriate for studying children and youth with TBI.
Key Measures: The Child Health Questionnaire (CHQ) and the Pediatric Evaluation of Disability Inventory (PEDI)
Prior to the meeting, participants identified two promising measures for assessing outcomes of TBI in children and youth, CHQ and the PEDI. The working group discussed the characteristics of these measures, which are summarized below.
Child Health Questionnaire (CHQ)
This summary was presented by Jeanne Landgraf, who developed the measure.
| Characteristics |
|
| Strengths |
|
| Weaknesses |
|
Pediatric Evaluation of Disability Inventory (PEDI)
This summary was presented by Stephen Haley, who developed the measure.
| Original PEDI |
|
| New Version of PEDI |
|
Selected Clinical Measures
A wide range of clinical measures is available for assessing outcomes of TBI. The working group discussed the applicability of these measures, some of which were originally developed for use with adults, to studies of children and youth, and the comments are summarized below:
Glasgow Coma Scale (GCS)
- Is a useful indicator of severity, but not for children younger than age 5.
- Scores for the same patient vary depending on when they were collected, e.g., GCS scores collected by Emergency Medical Technicians (EMTs) before admission are not as reliable as those collected in the ED or hospital. CDC TBI surveillance guidelines recommend use of the first GCS after admission to ED or hospital.
Children’s Coma Score
- Is a modification of the Glasgow Coma Score designed to be used in children aged 3 years and younger.
- Eye opening and motor response subscales are identical to the GCS, but the verbal response subscale rates behavior/affect in preverbal populations. (Multilingual Resources Assessment Tools. Available at: www.multilingualresources.com/ assessment.html. Accessed January 9, 2001).
- Is unclear how widely this score is being used or whether the score represents a significant improvement in the GCS for use with children. More research on this topic is needed.
Abbreviated Injury Score/Injury Severity Score (AIS/ISS)
- Are used routinely in the clinical setting.
- Most recent version (AIS 98) is better than previous versions for assessing children.
- Because of the variability within AIS levels, researchers should consider supplementing AIS/ISS with Therapeutic Intensity Level, which is used in some clinical settings to determine severity based on the intensity of treatment required by the patient (according to Nancy Carney).
- The AIS score for the head is highly correlated with GCS and is a useful measure of TBI severity.
Loss of Consciousness (LOC)
- Measures the length of time between injury and when the patient regains consciousness.
- Is strongly correlated with outcomes in children and adults and is a key piece of information that should be collected.
Length of Post-traumatic Amnesia (PTA)
- Measures the time from when a patient emerges from coma until he or she is no longer disoriented.
- Appears to be strongly correlated with outcome; however, it is difficult to document consistently and accurately within a hospital protocol.
- Inter-rater reliability is low; that is, different people report different lengths of PTA.
- Despite limitations, PTA should be collected and reported as accurately as possible.
Rancho Los Amigos Scale
- Is a 7-level scale for assessing early recovery in the brain injury rehabilitation setting.
- Rates behavior, cognitive functioning, and response to the environment.
- Levels range from No Response (Level I) through Purposeful-Appropriate Responses (Level VII). Multilingual Resources Assessment Tools. Available at: www.multilingualresources.com/assessment.html. Accessed January 9, 2001).
- May be useful for research on outcomes but to date has not been used widely or evaluated for that purpose.
Pediatric Trauma Score (PTS)
- Is a composite injury score in which the injured child receives a score of -1 (severely injured), +1 (moderately injured) or +2 (slightly injured or not injured) in each of six areas–body weight/size, airway, blood pressure, central nervous system activity, open wounds and skeletal injuries.
- (Ford EG, Andrassy RJ. Pediatric Trauma: Initial Assessment and Management. Philadelphia: W.B. Saunders Company; 1994).
- Score is not useful for TBI research because it does not separate head injury from injury to other body regions/functions.
Neuropsychological/psychiatric tests
- These detailed tests of cognitive and psychological functioning are frequently conducted by trained professionals.
- Results from these tests are important, particularly to document more subtle deficits, but they must be done in a clinical setting.
School Performance Assessments
Assessments of school performance include achievement tests, which measure students’ academic performance, and school function assessments, which assess students’ ability to behave appropriately in the classroom.
Achievement tests
- These tests of academic achievement are not sensitive to TBI-related problems.
- Thinking and reasoning are not assessed.
- Bright students may do well based on previous learning, thus masking TBI-related problems.
- Scores may improve even as behavior worsens.
- Achievement test results, if available for review, might provide some useful information about previous performance; however, meeting participants did not strongly recommend including them in studies assessing longer term outcomes of TBI.
School function assessments
- These checklists are specifically designed to assess functioning in the classroom setting.
- They are helpful in detecting problems specific to the classroom, including awareness of hygiene and behavior regulation.
- Meeting participants recommended including at least some key items from school function assessments in studies of outcomes of TBI in children and youth.
Recommendations for Additional Research into TBI in Children and Youth
Objective
This section summarizes participant recommendations regarding the wide-ranging needs for additional research and improved research methods in studies of TBI in children and youth.
The Need for Qualitative Research
Qualitative research facilitates an increased understanding of the experiences of people with TBI, their caregivers, or professionals working with people with TBI from their own unique and personal perspectives. Such information can guide the development of informational materials and questionnaires for epidemiologic studies. Common qualitative research techniques include focus groups and individual interviews. (See Patton MQ. Qualitative Evaluation and Research Methods (2nd Ed). Newbury Park, CA: Sage Publications, 1990.)
One meeting participant also had experience in conducting in-depth ethnographic, naturalistic studies with children with other health conditions (e.g., a study of children with asthma collected data by allowing them to carry video cameras). Participants recommended exploring the applicability of these methods to studies of TBI.
Research Topics
Basic
Basic research addresses physiologic responses to brain injury. Meeting participants noted that further studies are needed to:
- Reveal the underlying mechanisms of recovery
- Identify outcomes due to the injury itself vs. those that are secondary (e.g., neurogenic vs. situational depression).
Patterns of Recovery
Because recovery after TBI can be lengthy and because the risk of developing secondary conditions changes over time, better information about patterns of recovery from TBI is needed to understand the long-term effects of TBI. Meeting participants noted that further studies are needed to describe:
- The natural history of recovery from TBI. For example, when are secondary conditions most likely to develop?
- Recovery trajectories. That is, how quickly does recovery occur and in what order are skills regained?
- The later emergence of TBI-related problems especially in children. For example, are infants with TBI more likely to have later learning disabilities, such as trouble with reading or math, or behavior problems that are associated with the TBI?
Treatment
The NIH Consensus Conference on the Rehabilitation of Persons with Traumatic Brain Injury documented the need for improved research on treatment of TBI, including treatment for children. Meeting participants noted the need for further studies about
- The effectiveness of various treatments and the importance of the intensity level of those treatments
- The effectiveness of educational and behavioral interventions
- The implementation of treatment guidelines – Specific issues include how widely the guidelines are being applied and what effects implementation has on TBI outcomes.
- Personal (or person-centered) outcomes – Personal outcomes are the expectations that people with disabilities have for their lives, including what they expect from the services and supports they receive. Many service providers have adopted personal outcomes as a measure of quality of their services. (The Council on Quality and Leadership in Supports for People with Disabilities, Towson, MD. 410-583-0060)
Costs
Few studies have looked at the cost of TBI, especially among children. Cost data can help focus greater attention on a public health problem such as TBI. Meeting participants noted that further studies are needed to document:
- The costs of TBI in children, including reduced quality of life, compared with costs for other child health conditions (e.g., asthma, HIV)
- The economic impact of TBI on children, their families, and society.
Issues of Measurement and Data Analysis
Among the greatest challenges to conducting high-quality research on outcomes of TBI in children are limitations in existing outcome measures and analytic approaches as well as the lack of standard terminology to describe the outcomes. Meeting participants offered the following recommendations to improve measurement, analysis, and terminology:
- Conduct studies to assess the validity of existing measures for use in follow-up studies (i.e., sensitivity to individual changes over time) and apply improved methods for testing item validity.
- Use new types of measures including cognitive measures for use by school psychologists and applicable to consumers; a global measure of cognitive function that assesses memory; a cognitive screening tool for surveillance; a TBI-specific outcomes measure; a severity measure for comparing the burden of TBI with that of other conditions; and improved measures of the environment and its relationship to disability.
- Develop a standard terminology to describe and document service needs and barriers.
- Develop new analytic approaches including application of growth curve analysis to detailed studies of the relationship between development and recovery from TBI.
Other Methodologic Issues in Assessing TBI Outcomes in Children
Objective
The objective for this section is to review key issues to consider in conducting studies of TBI outcomes in children and youth.
Meeting participants had a wide range of experiences in obtaining information from children with TBI, their families and schools. These sections document participants’ ideas about the challenges of designing and implementing a study of outcomes of TBI in children and youth and how they should be managed.
Considerations for Defining the Study Population
Degree to which the Study Population Represents the General Population
Meeting participants discussed how representative the study population would be if children were selected for follow-up using the same approach used in CDC follow-up studies of older adolescents and adults. That approach, which identifies cases from surveillance systems using hospital discharge data sets, has some important limitations:
- It may underestimate problem outcomes because those who can still be identified and followed after one-year post-hospital discharge tend to have more resources and more stable lives (for adults followed in the Colorado follow-up system, about 35% are lost to follow-up within one year).
- It probably does not include an adequate subsample of children from low-income families.
- It does not include children seen in the emergency department (ED) but not admitted to hospital. The majority of children with TBI are seen only in the ED.
Sampling Frame
Participants discussed an appropriate sampling frame for selecting cases for follow-up studies of children. They determined that the sampling frame should include both children treated and released from the ED and children discharged from the hospital. The population should then be stratified by severity before selecting the sample.
Information from Parents / Caregivers and Schools
Participants also discussed whether the study should collect information from parents / caregivers or schools:
Parent / caregiver:
- A study should include assessments of both the parent (caregiver) and older children (age 8 to 10 or older). Parents and children may differ in reporting, especially about the social experiences of the child, with the parent reporting that the child has more friends and fewer problems with peer interactions than the child reports.
School:
- A study should incorporate school assessments of the child’s abilities, if possible.
- Parents’ and teachers’ understanding of the child’s individual educational plan (IEP) may differ, so getting both perspectives is important.
- Parents tend to rate their child’s school performance higher than do school personnel. The more time that has elapsed since the injury, the higher parents tend to rate pre-injury performance (including school performance).
- Interviews of teachers could yield some valuable information, especially for younger children who have one teacher only.
- Information from school records may also be useful; however, school records may not be complete, and schools are inconsistent in classifying children’s disability. For example, a child with a brain injury may be classified as having a learning disability, not a TBI.
- School records may not be a thorough source of information about grade retention and services received, but these areas are important, so a study should obtain information about them using other methods if necessary.
- Other school-related information of interest includes drop-out rates, achievement on statewide standardized tests and transfers to alternative schools.
- Whether obtaining information requires IRB approval from each school might vary by location, so researchers should check before beginning the study.
Appropriateness of Telephone Interviews for Children / Youth Follow-up Studies
Instead of using in-person interviewing, which is very expensive, CDC has used telephone interviewing to collect information in its follow-up studies of older adolescents and adults. Meeting participants discussed the appropriateness of this approach for studies among children and youth.
General Issues
Before beginning telephone interviewing, researchers should investigate telephone coverage among the proposed study population because low-income families may not have telephones. Researchers might also consider newer alternatives such as Internet administration, but Internet coverage among low-income families is likely to be even lower than for telephones.
Telephone vs. In-Person
Studies show that responses vary according to mode of administration (telephone vs. in-person and, for in-person interviews, whether the interview is conducted by a doctor/nurse or other type of interviewer). People tend to report fewer impairments when they are interviewed in-person than when they are interviewed by telephone. Therefore, researchers might need to compare responses from in-person and phone interviews in a sample of participants to evaluate reliability.
Interviewing Children by Telephone
Studies suggest that interviewing by telephone may not be appropriate for children and youth younger than age 13. TBI-related deficits and problems such as fatigue and limited attention span may make phone interviews with young people more difficult.
Suggestions for Enhancing Telephone Administration
- Pilot the questionnaire and revise based on results and experience before beginning the main study.
- Consider mailing the parent questionnaire before the interview to give them time to think about their answers.
Appropriate Interview Length
- Questionnaires for use with children and youth with TBI should be as short as possible to minimize fatigue among participants. Questionnaires for use with their parents may be longer but should also be kept as short as possible.
- Interviews should not exceed 45 minutes for adolescents while approximately 60 minutes is appropriate for parents. Meeting participants suggested that questionnaires for use with children should be pilot tested to determine the appropriate interview length.
- Meeting participants also suggested pilot testing a longer version for use with adolescents or parents to see how they respond. Families of children with TBI may be very invested in outcomes and often like to have someone to talk with. Some meeting participants reported surprise at the willingness of parents to be interviewed for longer than 60 minutes.
Effective Follow-up Interviews
Longitudinal studies of TBI outcomes involve an initial interview sometime after TBI, then tracking participants and re-interviewing them periodically, often at one-year intervals. Of particular concern is the potential for loss to follow-up because the families move or no longer agree to be part of the study. Meeting participants offered these suggestions for follow-up with children who have TBI:
Timing of Follow-Up
- Begin interviewing earlier than one year after the injury (optimally at 3-6 months). This approach could help decrease loss to follow-up because the family is less likely to have moved from the address found in the medical record. This approach would also provide useful information about patterns of early recovery.
- Consider beginning active surveillance and follow-up while people are still in the hospital.
- Follow-up beginning at one year is not timely enough to meet the needs of people with TBI to be identified early and linked to information that can help them get the services they need. Meeting these needs requires a case management approach, even if it is cost- and resource-intensive. The principal investigator for the South Carolina follow-up study of older adolescents and adults estimates that double the funding it currently receives from CDC would be required to initiate active surveillance of TBI. To decrease the cost and improve the feasibility of conducting more active surveillance, researchers should consider limiting surveillance to the few hospitals that see the majority of child TBI cases—for example, Level I trauma centers and children’s hospitals.
- Consider alternative approaches to tracking, especially for very young children, such as early intervention tracking systems that follow very young children (younger than age 3) who have TBI or other disability (e.g., in Rhode Island).
Length of Follow-Up
A single year of follow-up is insufficient to document important outcomes. Ideally, a study should follow children as long as possible through as many developmental transitions as possible to try identifying late-emerging problems resulting from TBI. Based on experience with the currently funded CDC studies of outcomes in older adolescents and adults, three- to five-year follow-up is feasible considering estimated cost and loss to follow-up.
Tracking
To reduce loss to follow-up, researchers should test a mechanism for routinely contacting participant families, such as sending a postcard at frequent intervals to track changes of address.
Advantages of and Selected Methods for Comparison Groups
Meeting participants strongly recommended including a comparison group as part of any follow-up study of outcomes of TBI in children to strengthen the study design and improve the usefulness of the findings. A comparison group completes the same questionnaire as the follow-up study participants, and researchers compare their responses with those of the children with TBI. The comparison group need not be the same size as the group of children with TBI. Methods of selecting a comparison group vary. Meeting participants discussed the pros and cons of each method, as summarized below:
Non-TBI Trauma Comparison Group
This approach entails selecting a population of children who were injured but did not have a TBI, matched by age and sex with the TBI children. The approach helps control for risk factors for injury that are similar between the two groups. The comparison group should be matched by socio-economic status to the TBI group.
- Researchers should consider the length of time following the trauma in selecting the comparison group. If the concern is adjusting for pre-injury risk factors only, selecting children who have recovered from the trauma may be more appropriate.
- Keeping non-TBI trauma controls involved in the study requires much effort, especially if they will be interviewed more than once, because they are not as invested in it as family members.
- Meeting participants strongly recommended this approach.
Friend Comparison Group
This approach involves selecting one similar-aged friend for each child with a TBI. The “friend control” completes the questionnaire. The approach helps control for social environment and school context, but friend controls might not have the same pre-injury risk factors.
- Defining “friend” may be difficult for very young children. Also, many children lose their friends after the TBI, so identifying a friend control may be difficult.
- Keeping friends involved in the study requires effort because they are not as invested in it as family members.
- Meeting participants recommended this approach as useful but with several limitations.
Sibling Comparison Group
This approach involves selecting a brother or sister of the child with TBI to serve in the comparison group. The approach helps control for family environment factors, but matching on age and sex may be impossible or there may not be any siblings.
- Siblings may not be a good comparison group because, as part of the family of the child with TBI, they also feel effects of the trauma.
- Meeting participants did not recommend this approach.
- Age- and Sex-Matched Comparison group
This approach involves selecting a sample of children from the general population, matched by age and sex. The approach allows comparison of the normal developmental trajectory with the trajectory for children with TBI.
Meeting participants recommended this approach. They also suggested that the optimal study would include both an age- and sex-matched comparison group and a non-TBI trauma comparison group.
Other TBI Issues
Research on outcomes of TBI is only one component of a broader effort to improve the lives of children with TBI. Meeting participants also noted the need for improved education and awareness of TBI as a public health problem and the need for more CDC research. To address those needs, participants offered the following suggestions:
Education and Awareness
In the TBI Act Reauthorization of 2000, CDC has been given expanded authorization for an education and awareness campaign. The campaign should consider:
Increasing overall public awareness
- A recent Harris poll, commissioned by the Brain Injury Association, revealed that the American public greatly underestimates the magnitude and importance of TBI (www.biausa.org/harrispollresults.htm. Accessed January 24, 2001).
- All educational efforts should strive to use standard terminology to increase understanding and improve communication about TBI.
Raising awareness in the medical and TBI communities
- The campaign should educate the medical and TBI communities that so-called “mild” TBI can result in serious, long-term deficits. A relatively large number of children have problems after mild TBI.
- A group of neuropsychologists, now at the University of Pittsburgh, has developed a computer-based sports sideline screening for symptoms of concussion. The National Football League (NFL) first used the screening, and now some college and high school sports use it, which has generated a lot of attention from parents.
Increasing the awareness of parents and caregivers
- Parents and caregivers also need to better understand what they can expect after a child has a TBI, especially a less severe TBI.
- Cultural sensitivity is critical.
- Efforts to develop materials that increase awareness should begin with focus groups to understand children’s and families’ perspectives and the language that is meaningful to them.
- Educational efforts should be sensitive to the different information needs of parents of children whose disability resulted from a sudden change (i.e., TBI) and of parents of children with developmental disability. An education campaign should try to ensure that the information about possible outcomes of TBI in children does not result in negative self-fulfilling prophecies. For example, children with mild-to-moderate TBI may have cognitive deficits, but they are still capable of learning.
Dissemination
CDC should distribute educational materials as widely as possible, including through the HRSA Maternal and Child Health Bureau Clearinghouse, which distributes a wide range of materials on children’s health.
CDC Research Efforts
Meeting participants offered the following additional suggestions for steps the CDC should take to improve knowledge about TBI outcomes in children.
- Continue to collect data while ensuring more widespread dissemination.
- CDC should continue to increase awareness of the TBI problem by collecting and sharing data about the incidence and prevalence of TBI and TBI-related disability. Information should be in a form that can be distributed by health professionals to people with TBI and their families. For example, CDC should publish more brochures like the concussion brochure (Facts about Concussion and Brain Injury, Accessed January 24, 2001).
- Support, promote and conduct additional research.
- CDC should make its surveillance data sets more widely and readily available to other researchers and professionals, including via the Internet.
- CDC needs to identify research gaps and issue requests for proposals (RFPs) to address those gaps. Future CDC studies should document:
- the disproportionately low funding for TBI compared with the burden of TBI
- poor coverage of services by insurance companies
- the percentage of children with TBI receiving services and the percentage not receiving them
- the need for appropriate educational programming for children and youth with TBI.
Appendex A
References for Appendix A
- Achenbach System of Empirically Based Assessment Web Site. Available at: www.uvm.edu/~cbcl. Accessed October 19, 2000.
- Boston University Center for Rehabilitation Effectiveness PEDI page. Available at: www.bu.edu/cre/pedi. Accessed October 19, 2000.
- Bradlyn AS, Harris CV, Warner JE, Ritchey AK, Zaboy K. An investigation of the validity of the Quality of Well-Being Scale with pediatric oncology patients. Health Psychology. 1993;12:246-250.
- Burgess ES. Drotar D, Taylor HG, Wade S, Stancin T, Yeates KO. The Family Burden of Injury Interview: Reliability and validity studies. Journal of Head Trauma Rehabilitation. 1999;14:394-405.
- Carlson EB. Trauma assessments: A clinician’s guide. New York: The Guilford Press; 1997.
- Child Health Questionnaire. Availble at: www.chqmanual.com. Accessed October 19, 2000.
- Coster W, Deeney T, Haltiwanger J, Haley S. Technical Report for the School Function Assessment. Available at: www.psychcorp.com/catg/resource/techrpts/sfa1.html. Accessed November 6, 2000.
- Czyzewski DI, Mariotto MJ, Bartholomew LK, LeCompte SH, Sockrider MM. Measurement of quality of well-being in a child and adolescent cystic fibrosis population. Medical Care. 1994;32:965-972.
- Dittmar SS, Gresham GE. Functional assessment and outcome measures for the rehabilitation health professional. Gaithersburg, MD: Aspen Publishers, Inc.; 1997.
- Gioia G. Personal communication, November 1, 2000.
- Hill B. Adaptive and maladaptive behavior scales. Available at: www.isd.net/bhill/compare.htm. Accessed November 3, 2000.
- Landgraf JM. Abetz LN. Measuring health outcomes in pediatric populations: Issues in psychometrics and application. In: Spilker B, editor. Quality of life and pharmacoeconomics in clinical trials. 2nd ed. Philadelphia: Lippincott-Raven Publishers; 1996. p. 793-800.
- Lansky LL, List MA, Lansky SB, Cohen ME, Sinks LF. Toward the development of a Play Performance Scale for Children (PPSC). Cancer. 1985;56:1837-1840.
- Kamphaus RW, Petoskey MD, Cody AH, Rowe EW, Huberty CJ. A typology of parent rated child behavior for a national U.S. sample. Journal of Child Psychology and Psychiatry. 1999;40:607-616.
- Kozinetz CA, Warren RW, Berseth CA, Aday LA, Sachdeva R, Kirkland RT. Health status of children with special health care needs: Measurement issues and instruments. Clinical Pediatrics. 1999;38:525-533.
- Max JE, Koele SL, Lindgren SD, Robin DA, Smith WL, Sato Y, Arndt S. Adaptive functioning following traumatic brain injury and orthopedic injury: A controlled study. Archives of Physical Medicine and Rehabilitation. 1998;79:893-899.
- McDowwell I, Newell C. Measuring health: A guide to rating scales and questionnaires. 2nd ed. New York: Oxford University Press; 1996.
- Middleton HA, Keene RG, Brown GW. Convergent and discriminant validities of the Scales of Independent Behavior and the Revised VinelandAdaptive Behavior Scales. American Journal on Mental Retardation. 1990;94:669-673.
- Scales of Independent Behavior-Revised. Available at: www.riverpub.com/products/clinical/sibr_indepth.htm. Accessed November 3, 2000.
- Spreen O, Strauss E. A compendium of neuropyschological tests: Administration, norms, and commentary. 2nd ed. New York: Oxford University Press; 1998.
- Stancin T, Taylor HG, Thompson GH, Wade S, Drotar D, Yeates KO. Acute psychosocial impact of pediatric orthopedic trauma with and without accomplanying brain injuries. Journal of Trauma. 1998;45:1031-1038.
- Starfield B, Ensminger M, Riley A, Ryan S, Green B, McHauhey P, Skinner A, Kim S. Adolescent health status measurement: Development of the Child Health and Illness Profile. Pediatrics. 1993;91:430-435.
- Stein RE, Jessop DJ. Functional Status II(R): A measure of child health status. [published erratum appears in Medical Care 1991;29:489]. Medical Care. 1990;28: 1041-1055.
- Uniform Data System for Medical Rehabilitation. Available at: www.udsmr.org. Accessed October 19, 2000.
- Varni JW, Seid M, Rode CA. The PedsQL: Measurement model for the Pediatric Quality of Life Inventory. Medical Care. 1999;37:126-139.
- Vila G, Nollet-Clemecon C, Vera M, Robert JJ, deBlic J, Jouvent R. Prevalence of DSM-IV disorders in children and adolescents with asthma versus diabetes. Canadian Journal of Psychiatry. 1999;44:562-569.
- Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO. Family burden and adaptation during the initial year after traumatic brain injury in children. Pediatrics. 1998;102:110-116.
- Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: The Guilford Press; 1997.
Appendix B
Traumatic Brain Injury in Children and Youth as a Public Health Problem: An Overview
Presented by Dr. David Thurman, CDC
This section features copies of the slides from Dr. David Thurman’s presentation. The surveillance data (beginning with Slide 2) are from selected states for the information available at the time of the meeting; therefore, the data should be considered preliminary.
Slide 1 – Estimated Impact of TBI on Children Aged 0-14 Years in the United States
- 3,000 deaths (NCHS, 1994)
- 29,000 hospitalizations
- 400,000 ED visits (NHAMCS, 1996)
- Unknown number with long-term disability
Slide 2 – Preliminary Surveillance Findings for TBI-Related Hospitalizations & Deaths –1997
TBI Surveillance–Background
- CDC collects data on TBI-related injuries from 15 states.
- Clinical case definition: Injury to the head associated with decreased consciousness, amnesia, neurologic abnormalities, skull fracture, intracranial lesion or death.
- Data case definition: ICD-9 codes 800-801, 803-804, 850-854 and (for fatalities only) 873.
- Data sources: Vital records, hospital discharge data and medical records (for a sample of cases).
- Data elements: Demographic, nature of injury (ICD-9 N-codes), cause of injury (ICD-9 E-codes), severity, and outcome.
- For this presentation, unless otherwise noted, data are from Minnesota, Missouri, South Carolina and Utah
Slide 3 – Figure 1: Rates of TBI in Children and Youth by Age Group & Care Level, 1997
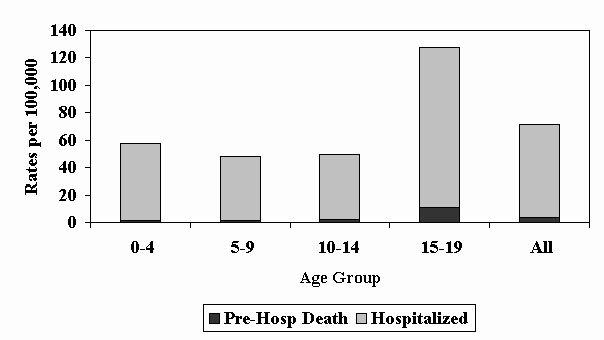
TBI death and hospitalization rates were highest among those aged 15-19 year
Slide 4 – Figure 2: TBI in Children and Youth: Percent with Fatal Outcomes, 1997
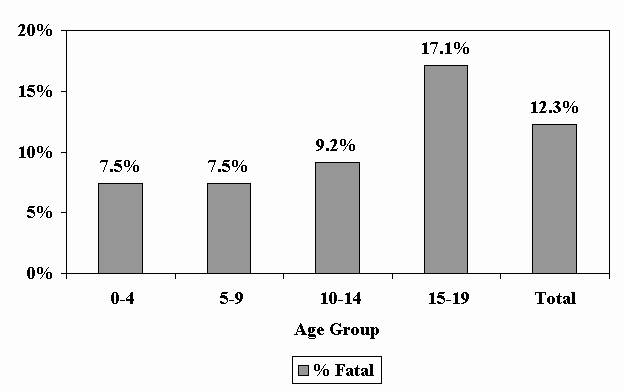
Slide 5 – Figure 3: TBI Rates in Children and Youth by Age and Race, 1997
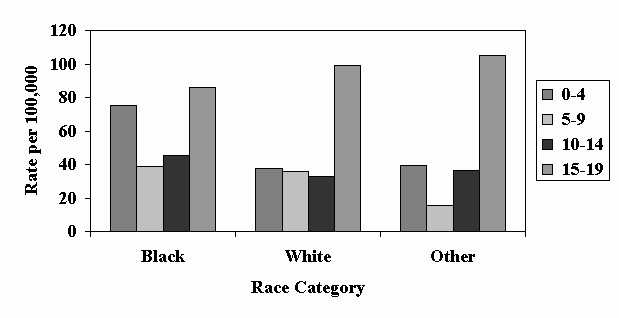
(28% of cases were of unknown race)
- For all categories of race, the highest TBI rates were among youth, aged 15-19 years followed by children aged 0-4 years.
- The TBI rate in black children aged 0-4 years was approximately twice as high as for the same-aged white or other race children.
Slide 6 – Figure 4: Rates of TBI in Children and Youth by Age Group and External Cause of Injury, 1997
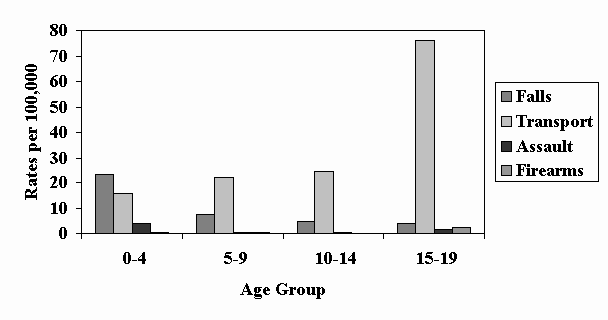
- The rate of TBI from falls decreased with increasing age.
- The rate of TBI from transportation incidents was more than three times as high for youth aged 15-19 years as for children in the younger age groups.
- The rate of TBI from firearm-related injuries was highest among 15-19 year-olds.
- The rate of TBI from non-firearm assaults was highest among 0-4 year-olds.
Slide 7 – Figure 5: TBI in Children Aged 0-4 Years: Proportion by Cause & Race, 1997
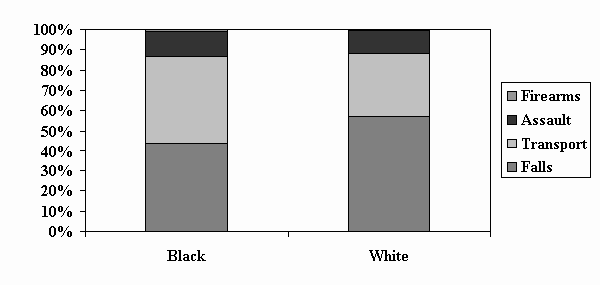
Children aged 0-4 years, falls were the leading cause of TBI, followed by transportation and assaults; however, transportation-related TBIs accounted for a greater proportion among black children than among whites.
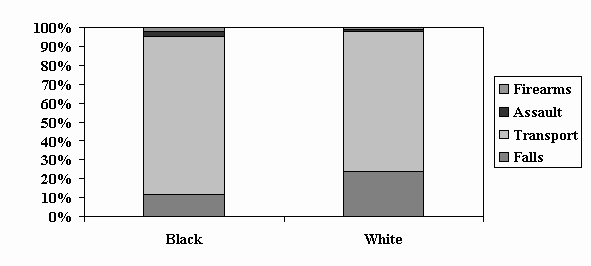
Slide 8 – Figure 6: TBI in Children Aged 5-14 Years: Proportion by Cause & Race, 1997
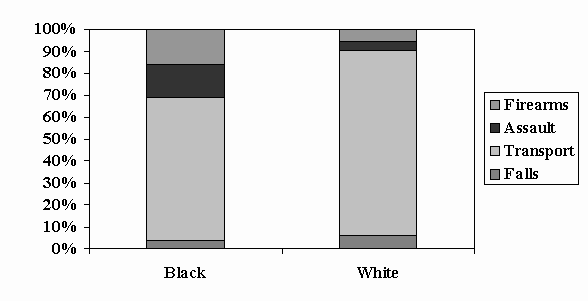
Slide 9 – Figure 7: TBI in Youth Aged 15-19 Years: Proportion by Cause and Race, 1997
Appendix C
TBI in Children and Youth Data from the South Carolina Surveillance System
The following are copies of the lecture slides from Dr. Anbesaw Selassie’s presentation:
Slide 1 – Table 1: Distribution of TBI in Children Treated and Released from Emergency Departments—South Carolina, 1996-1999
|
Female |
Male |
All |
||||
|---|---|---|---|---|---|---|
| Age Group (yrs) | Number | Percent (%) | Number | Percent (%) | Number | Percent(%) |
| 0-4 | 1008 | 42 | 1395 | 58 | 2403 | 40 |
| 5-9 | 623 | 34 | 1192 | 66 | 1815 | 31 |
| 10-14 | 564 | 33 | 1168 | 67 | 1732 | 29 |
| All | 2195 | 37 | 3755 | 63 | 5950 | 100 |
- Males 0 to 4 years of age had the greatest number of TBI-related ED visits.
- Among 0 to 14 year-olds, the total number of TBI ED visits (5,950) was more than 4 times the number of TBI-related hospital discharges (1,451–see Table 2).
Slide 2 – Figure 1: Annual Rate of TBI in Children Treated and Released from Emergency Departments – South Carolina, 1996-1999
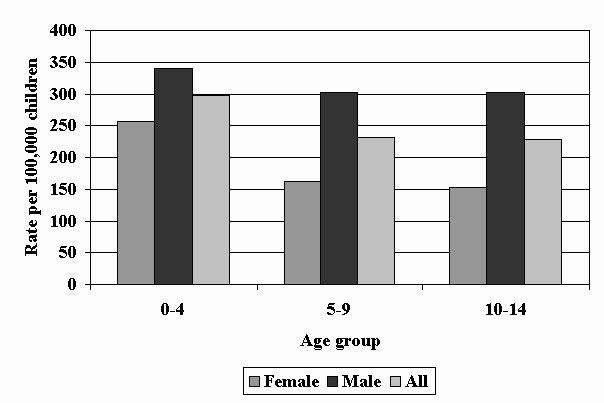
- The annual rate of TBI-related ED visits was greatest among children aged 0-4 years (298 visits per 100,000).
- The rate of TBI-related ED visits was similar for children aged 5-9 years and 10-14 years (232 and 228 per 100,000, respectively).
- For all age groups, males had higher rates of TBI-related ED visits, and the difference increased with age.
Slide 3 – Table 2: Distribution of TBI in Children Discharged from Acute Care Facilities—South Carolina, 1996-1999
|
Female |
Male |
All |
||||
|---|---|---|---|---|---|---|
| Age Group (yrs) | Number | Percent (%) | Number | Percent (%) | Number | Percent(%) |
| 0-4 | 230 | 41 | 336 | 59 | 566 | 39 |
| 5-9 | 152 | 36 | 271 | 64 | 423 | 29 |
| 10-14 | 146 | 32 | 316 | 68 | 462 | 32 |
| All | 528 | 36 | 923 | 64 | 1451 | 100 |
Slide 4 – Figure 2: Annual Rate of TBI in Children Discharged from Acute Care Facilities – South Carolina, 1996-1999
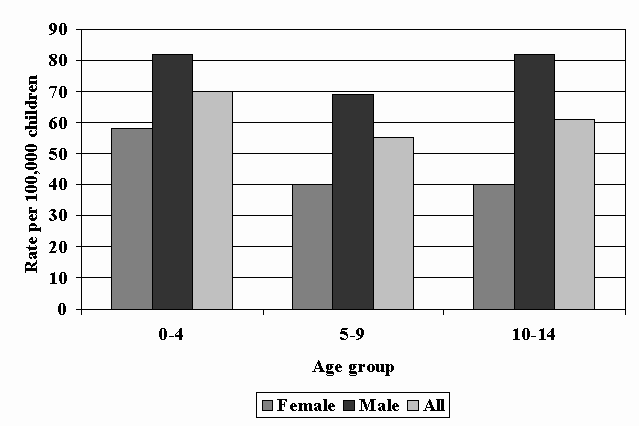
- The highest rate of hospitalization was for children aged 0-4 years (70 per 100,000), followed by 10 to14 year-olds (61 per 100,000), and 5 to 9 year-olds (55 per100,000).
- The rate of hospitalization for males was greater than for females at all ages.
Slide 5 – Table 3: Type of TBI in Children Treated and Released from EDs – South Carolina, 1996-1999
Slide 6 – Table 4: Type of TBI in Children Discharged from Acute Care Facilities – South Carolina, 1996-1999
- Intracranial hemorrhages were the third most common TBI-related discharge diagnosis after unspecified closed head injuries and concussions.
- Although less common than for ED visits, concussions accounted for nearly 1 in 5 TBI-related hospitalizations.
Slide 7 – Table 5: Distribution of Predicted H Disablement from TBI in Children Treated and Released from ED Facilities – South Carolina, 1996-1999
| Age (Yrs) |
Probable |
Possible |
Unlikely |
All |
||||
|---|---|---|---|---|---|---|---|---|
| Num. | % | Num. | % | Num. | % | Num. | % | |
| 0-4 | 55 | 2 | 126 | 5 | 2222 | 92 | 2403 | 40 |
| 5-9 | 30 | 2 | 82 | 5 | 1703 | 94 | 1815 | 31 |
| 10-14 | 46 | 3 | 107 | 6 | 1579 | 91 | 1732 | 29 |
| All | 131 | 2 | 315 | 5 | 5504 | 93 | 5950 | 100 |
H Prediction based on an algorithm that incorporated severity, disposition, and type of injury. ROC curve C-Statistic expressing “Association of Predicted Probabilities and Observed Responses” is 0.86 for probable and 0.68 for possible disablement categories.
- These figures represent conservative estimates.
- For additional information, contact Dr. Anbesaw Selassie (please refer to the list of participants).
Slide 8 – Table 6: Distribution of Predicted H Disablement from TBI in Children Discharged from Acute Care Facilities – South Carolina, 1996-1999
| Age (Yrs) |
Probable |
Possible |
Unlikely |
All |
||||
|---|---|---|---|---|---|---|---|---|
| Num. | % | Num. | % | Num. | % | Num. | % | |
| 0-4 | 50 | 9 | 250 | 44 | 266 | 47 | 566 | 40 |
| 5-9 | 20 | 5 | 203 | 48 | 200 | 47 | 423 | 29 |
| 10-14 | 52 | 12 | 223 | 48 | 187 | 40 | 462 | 29 |
| All | 122 | 8 | 676 | 47 | 1451 | 45 | 1451 | 100 |
H Prediction based on an algorithm that incorporated severity, disposition, and type of injury. ROC curve C-Statistic expressing “Association of Predicted Probabilities and Observed Responses@ is 0.86 for probable and 0.68 for possible disablement categories.
- These figures represent conservative estimates.
- For additional information, contact Dr. Anbesaw Selassie (please refer to the list of participants).
Appendix D
Other Resources
In addition to this report, the following resources can help researchers select topics for research studies of TBI outcomes in young people.
HRSA/MCHB Principles for Meeting the Needs of the Child
Bright Futures Children’s Health Charter
Throughout this century, principles developed by advocates for children have been the foundation for initiatives to improve children’s lives. Bright Futures participants have adopted these principles to guide their work and meet the unique needs of children and families into the 21st century.
- Every child deserves to be born well, to be physically fit and to achieve self-responsibility for good health habits.
- Every child and adolescent deserves ready access to coordinated and comprehensive preventive, health-promoting, therapeutic, and rehabilitative medical, mental health and dental care. Such care is best provided through a continuing relationship with a primary health professional or team and ready access to secondary and tertiary levels of care.
- Every child and adolescent deserves a nurturing family and supportive relationships with other significant persons who provide security, positive role models, warmth, love and unconditional acceptance.
- A child’s health begins with the health of his parents.
- Every child and adolescent deserves to grow and develop in a physically and psychologically safe home and school environment free of undue risk of injury, abuse, violence or exposure to environmental toxins.
- Every child and adolescent deserves satisfactory housing, good nutrition, a quality education, an adequate family income, a supportive social network and access to community resources.
- Every child deserves quality childcare when her parents are working outside the home.
- Every child and adolescent deserves the opportunity to develop ways to cope with stressful life experiences.
- Every child and adolescent deserves the opportunity to be prepared for parenthood.
- Every child and adolescent deserves the opportunity to develop positive values and become a responsible citizen in his community.
- Every child and adolescent deserves to experience joy, have high self-esteem, have friends, acquire a sense of efficacy and believe that she can succeed in life. She should help the next generation develop the motivation and habits necessary for similar achievement.
Reference: www.brightfutures.org
Bright Futures is sponsored by MCHB, HRSA and, in part, supported by unrestricted educational grants from Pfizer Pediatric Health. Bright Futures material is produced by NCEMCH and is not copyrighted.
Selected Articles from the United Nations Convention on the Rights of the Child
Article 2
- States Parties shall respect and ensure the rights set forth in the present Convention to each child within their jurisdiction without discrimination of any kind, irrespective of the child’s or his or her parents’ or legal guardians’ race, color, sex, language; religion, political or other opinion; national, ethnic or social origin; property, disability, birth or other status.
Article 6
- States Parties shall ensure to the maximum extent possible the survival and development of the child.
Article 23
- States Parties recognize that a mentally or physically disabled child should enjoy a full and decent life, in conditions that ensure dignity, promote self-reliance and facilitate the child’s active participation in the community.
- States Parties recognize the right of the disabled child to special care and shall encourage and ensure the extension, subject to available resources, to the eligible child and those responsible for his or her care, of assistance for which application is made and which is appropriate to the child’s condition and to the circumstances of the parents or others caring for the child.
- Recognizing the special needs of a disabled child, assistance extended in accordance with paragraph 2 of the present article shall be provided free of charge whenever possible, taking into account the financial resources of the parents or others caring for the child, and shall be designed to ensure that the disabled child has effective access to and receives education, training, health care services, rehabilitation services, preparation for employment and recreation opportunities in a manner conducive to the child’s achieving the fullest possible social integration and individual development, including his or her cultural and spiritual development
- States Parties shall promote, in the spirit of international cooperation, the exchange of appropriate information in the field of preventive health care and of medical, psychological and functional treatment of disabled children, including dissemination of and access to information concerning methods of rehabilitation, education and vocational services, with the aim of enabling States Parties to improve their capabilities and skills and to widen their experience in these areas. In this regard, particular account shall be taken of the needs of developing countries.
Article 24
- States Parties recognize the right of the child to the enjoyment of the highest attainable standard of health and to facilities for the treatment of illness and rehabilitation of health. States Parties shall strive to ensure that no child is deprived of his or her right of access to such health care services.
Article 28
- States Parties recognize the right of the child to education and, with a view to achieving this right progressively and on the basis of equal opportunity, they shall, in particular:
- Make primary education compulsory and available free to all;
- Encourage the development of different forms of secondary education, including general and vocational education, make them available and accessible to every child and take appropriate measures such as the introduction of free education and offering financial assistance in case of need;
- Make higher education accessible to all on the basis of capacity by every appropriate means;
- Make educational and vocational information and guidance available and accessible to all children;
- Take measures to encourage regular attendance at schools and the reduction of drop out rates.
Article 29
- States Parties agree that the education of the child shall be directed to:
- The development of the child’s personality, talents and mental and physical abilities to their fullest potential;
Article 31
- States Parties recognize the right of the child to rest and leisure, to engage in play and recreational activities appropriate to the age of the child and to participate freely in cultural life and the arts.
- States Parties shall respect and promote the right of the child to participate fully in cultural and artistic life and shall encourage the provision of appropriate and equal opportunities for cultural, artistic, recreational and leisure activity.
Reference: www.unicef.org/crc/crc.htm Accessed January 24, 2001
Selected Healthy People 2010 Goals and Objectives
Goal 1: Increase quality and years of healthy life.
- Access to Medical Care
- Objective 1-6: Reduce the proportion of families that experience difficulties or delays in obtaining health care or do not receive needed care for one or more family members.
- Objective 1-15: Increase the proportion of persons with long-term care needs who have access to the continuum of long-term care services.
- Disability and Secondary Conditions
- Objective 6-1: Include in the core of all relevant Healthy People 2010 surveillance instruments a standardized set of questions that identify “people with disabilities.”
- Objective 6-2: Reduce the proportion of children and adolescents with disabilities who are reported to be sad, unhappy or depressed.
- Objective 6-4: Increase the proportion of adults with disabilities who participate in social activities.
- Objective 6-5: Increase the proportion of adults with disabilities reporting sufficient emotional support.
- Objective 6-6: Increase the proportion of adults with disabilities reporting satisfaction with life.
- Objective 6-7: Reduce the number of people with disabilities in congregate care facilities, consistent with permanency planning principles.
- Target: For persons 21 years and younger–total elimination.
- Objective 6-9: Increase the proportion of children and youth with disabilities who spend at least 80% of their time in regular education programs.
- Objective 6-10: Increase the proportion of health and wellness and treatment programs and facilities that provide full access for people with disabilities.
- Objective 6-11: Reduce the proportion of people with disabilities who report not having the assistive devices and technology needed.
- Objective 6-12: Reduce the proportion of people with disabilities reporting environmental barriers to participation in home, school, work, or community activities.
- Objective 6-13: Increase the number of Tribes, States, and the District of Columbia that have public health surveillance and health promotion programs for people with disabilities and caregivers.
- Maternal, Infant and Child Health
- Objective 16-22: Increase the proportion of children with special health care needs who have access to a medical home [for the provision and coordination of care].
- Objective 16-23: Increase the proportion of Territories and States that have service systems for children with special health care needs.
- Mental Health and Mental Disorders
- Objective 18-7: Increase the proportion of children with mental health problems who receive treatment.
- Public Health Infrastructure
- Objective 23-2: Increase the proportion of Federal, Tribal, State and Local health agencies that have made information available to the public in the past year on the Leading Health Indicators, Health Status Indicators, and Priority Data Needs.
- Objective 23-5: Increase the proportion of Leading Health Indicators, Health Status Indicators, and Priority data Needs for which data–especially for select populations–are available at the Tribal, State, and Local levels.
Reference: Accessed January 25, 200; or U.S. Department of Health and Human Services. Healthy People 2010. 2nd ed. With Understanding and Improving Health and Objectives for Improving Health. 2 vols. Washington, DC: U.S. Government Printing Office, November 2000.
Appendix E
I. Basic Surveillance: Defining the Magnitude of the Problem, Identifying Causes and High Risk Groups
In 1995, CDC funded TBI surveillance efforts in 4 states and developed Guidelines for Surveillance of Central Nervous System Injury.3 These surveillance efforts expanded with the implementation of Public Law 104-166, the Traumatic Brain Injury Act of 1996. Under the TBI Act, the CDC has developed a uniform reporting system to answer questions about the incidence and causes of TBI deaths and hospitalizations. The surveillance program currently supports data collection in the following 15 states:
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Louisiana
- Maryland
- Minnesota
- Missouri
- Nebraska
- New York
- Oklahoma
- Rhode Island
- South Carolina
- Utah
II. Outcomes Surveillance: The Colorado and South Carolina Traumatic Brain Injury Follow-up Systems
In 1995, CDC funded a follow-up study in Colorado to describe TBI-related disability, use of services, and other outcomes. A similar project was begun in South Carolina in 1998 including people with TBI aged 15 years or older. These projects:
- Each year, select a representative sample of people identified by surveillance who have been hospitalized and survived with a TBI.
- Locate each person in the sample within one year of their injury.
- Contact them and obtain consent to do a telephone interview.
- Interview each person about a wide range of outcomes and service needs (approximately 40 minutes); proxies are interviewed if the person is unable to participate themselves.
- Track each person and interview them again at 2 and 3 years post-injury.
- Analyze and report the results.
Project Strengths
- Population-based findings with the potential to generalize results to all people aged 16 years or older who have been hospitalized with a TBI.
- Wide range of outcomes assessed using both standardized and nonstandardized measures.
- Focus on “macro” outcomes relevant to policy-makers.
- Potential to build a case for the needs of people with TBI.
- The addition of a comparison group to the SC study to better delineate the impact of TBI.
Project Limitations
- Outcomes are assessed in limited detail.
- Self-report may not be valid among people with decreased awareness of problems.
- Loss to follow-up is high (approx. 35% at one year, 10-15% at years 2 and 3).
- Do not include people with less severe TBI seen in the ED or not receiving medical care.
- Do not include children and adolescents.
III. Future Directions: Adding Children and Adolescents to the TBI Outcomes Surveillance Projects
Obtaining population-based TBI outcomes data for children and youth is a high priority for the Advisory Committee of the National Center for Injury Prevention and Control, the Brain Injury Association and a wide range of experts and professionals who participated in the CDC-sponsored TBI in Public Health Meeting in April 1999. The TBI Act Reauthorization of 2000 also highlights it as a priority activity.
