Mammography
The content on this page was last updated in June 2023. More recent estimates and visualizations may be available from the NCHS Data Query System.
Cancer screening tests aim to detect cancers at early stages, when cancer may be easier to treat successfully (1). Although breast cancer is the second leading cause of cancer death for women in the United States, advancements in and increased use of cancer screening tests have contributed to decreasing breast cancer death rates since 1989 (2–4). The U.S. Preventive Services Task Force recommends breast cancer screening every 2 years in women aged 50–74 (5–7).
Key Findings
The age-adjusted percentage of women aged 40 and over who reported having a mammogram within the past 2 years was stable from 67.1% in 2008 to 65.6% in 2018. In 2019, 67.5% of women aged 40 and over had a mammogram within the past 2 years. See Featured Charts for additional analysis and Notes for more information about analyzing trends using NHIS data.
SOURCE: National Center for Health Statistics, National Health Interview Survey. See Sources and Definitions, National Health Interview Survey (NHIS) and Health, United States, 2020–2021 Table CanBrTest.
From 2008 to 2019, use of mammography differed by age.
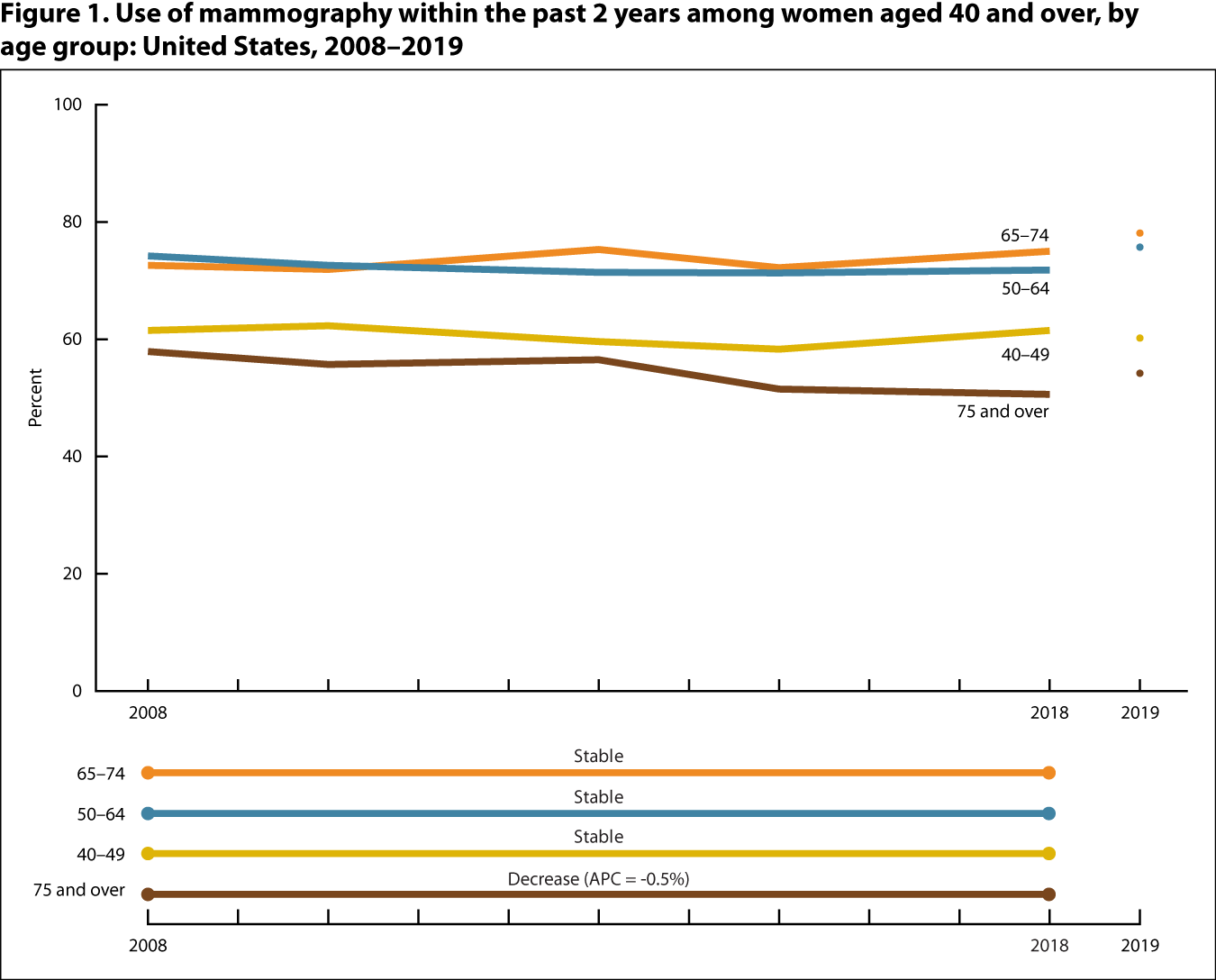
NOTES: “Stable” refers to no statistically significant trend during the period. APC is annual percent change.
SOURCE: National Center for Health Statistics, National Health Interview Survey. See Sources and Definitions, National Health Interview Survey (NHIS) and Health, United States, 2020–2021 Table CanBrTest.
- From 2008 to 2018, the percentage of women who reported having a mammogram within the past 2 years decreased for women aged 75 and over but remained stable during the period for other age groups of women aged 40 and over.
- In 2019, women aged 50–64 (75.7%) and 65–74 (78.1%) were more likely to report having a mammogram within the past 2 years than women aged 40–49 (60.2%) or 75 and over (54.2%).
In 2019, non-Hispanic Asian women were less likely to have a mammogram in the past 2 years than non-Hispanic Black and non-Hispanic White women.
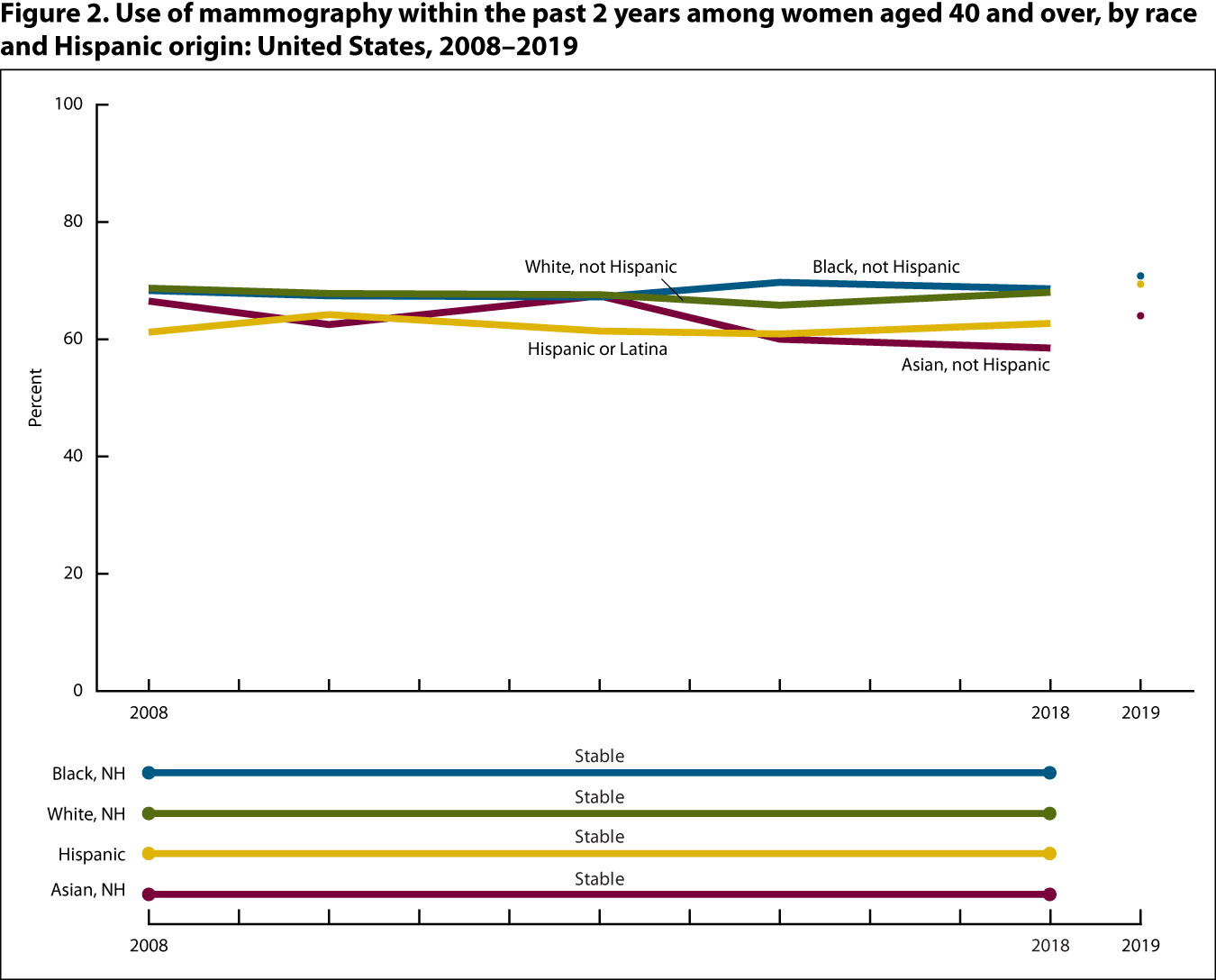
NOTES: NH is not Hispanic. “Stable” refers to no statistically significant trend during the period.
SOURCE: National Center for Health Statistics, National Health Interview Survey. See Sources and Definitions, National Health Interview Survey (NHIS) and Health, United States, 2020–2021 Table CanBrTest.
- For all race and Hispanic-origin groups, the percentage of women aged 40 and over who reported having a mammogram within the past 2 years fluctuated but did not change significantly from 2008 to 2018.
- In 2019, among women aged 40 and over, non-Hispanic Asian women (64.0%) were less likely to report having a mammogram within the past 2 years than non-Hispanic White (69.4%) and non-Hispanic Black (70.8%) women but were not statistically different from Hispanic women (69.4%).
- Hispanic origin: People of Hispanic origin may be of any race. See Sources and Definitions, Hispanic origin.
- Mammography: Use of mammography is defined as the percentage of women aged 40 and over who had a mammogram within the past 2 years. Survey questions have changed over time. See Sources and Definitions, Mammography.
- Race: Estimates are presented according to the 1997 Office of Management and Budget’s “Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity” and are for people who reported only one racial group. See Sources and Definitions, Race.
- Pinsky PF. Principles of cancer screening. Surg Clin North Am 95(5):953–66. 2015.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. 2018.
- Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L. Effectiveness of breast cancer screening: Systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med 164(4):244–55. 2016.
- American Cancer Society. Breast cancer facts & figures 2019–2020. Atlanta, GA: American Cancer Society, Inc. 2019.
- Siu AL, U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 164(4):279–96. 2016.
- U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 151(10):716–26. 2009.
- Force USPST. Screening for breast cancer: Recommendations and rationale. Ann Intern Med 137(5 Part 1):344–6. 2002.