Surveillance
Rates of meningococcal disease in the United States increased in 2023. Public health officials track all meningococcal disease in the United States. Health departments respond to every case of meningococcal disease and implement control measures to reduce spread of the disease.
Increase in disease, 2023
Cases of meningococcal disease in the United States have increased sharply since 2021 and now exceed pre-pandemic levels (see Figure 1). In 2023, 422 confirmed and probable meningococcal disease cases were reported in the United States (preliminary data). This is the largest number of U.S. meningococcal disease cases reported since 2014.
Much of the increase in meningococcal disease is driven by Neisseria meningitidis serogroup Y.
People disproportionately affected by the increase include:
- People between the ages of 30 and 60 years
- Black or African American people
- Adults with HIV
CDC issued a Health Alert Network (HAN) Health Advisory on March 28, 2024, about the increase in invasive serogroup Y meningococcal disease in the United States.
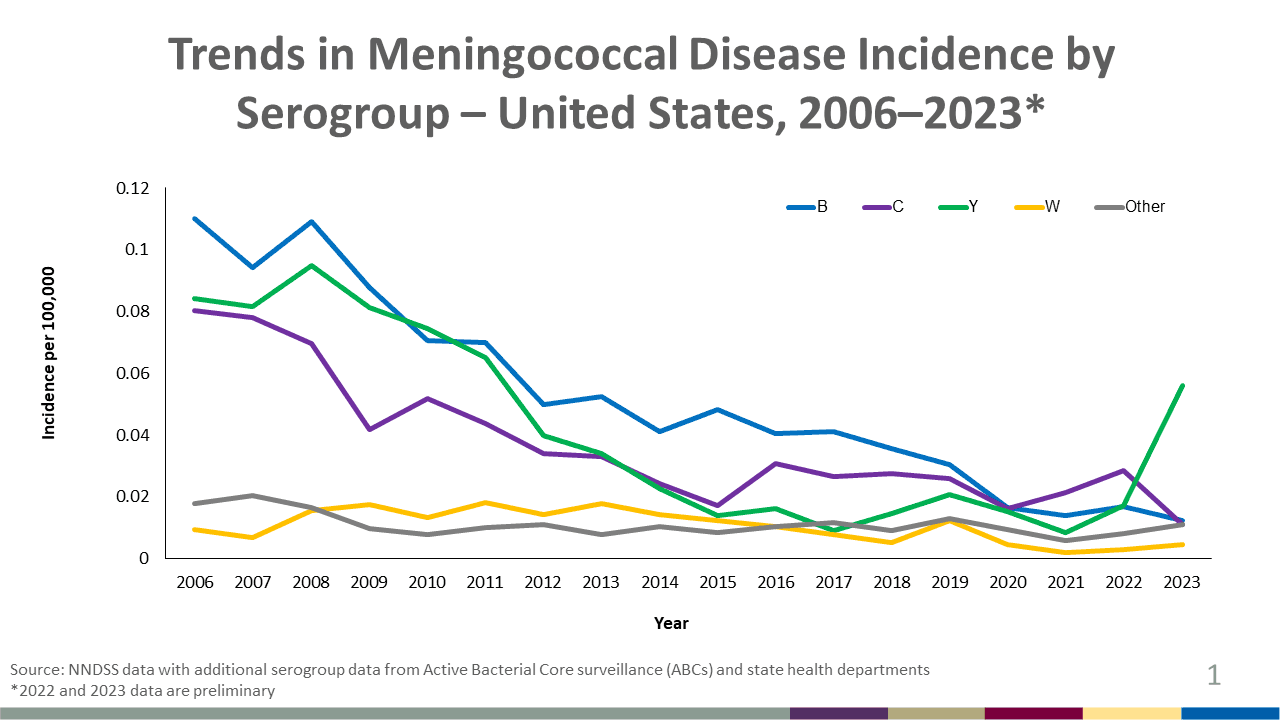
Figure 1 shows reported incidence of meningococcal disease declining or holding steady for all serogroups during 2006–2022 with an increase in serogroup Y incidence starting in 2022.
Public health officials should encourage healthcare providers to:
- Maintain a heightened suspicion for invasive meningococcal disease and recognize that invasive meningococcal disease may affect people of any age or demographic group.
- Current increases in disease are disproportionately affecting people aged 30–60 years, Black or African American people, and people with HIV.
- Be aware that patients with meningococcal bloodstream infection or septic arthritis may present without typical meningitis symptoms.
- Ensure that all people who are recommended to receive meningococcal vaccination are up to date.
- For people with HIV, recommended MenACWY vaccination includes a 2-dose primary series with booster doses every 3 to 5 years depending on age.
Antibiotic-resistant N. meningitidis serogroup Y
Due to recent reports of β-lactamase-producing N. meningitidis serogroup Y in the United States, including 24 cases also resistant to ciprofloxacin:
- Healthcare providers should ascertain susceptibility of meningococcal isolates to penicillin before using penicillin or ampicillin for treatment.
- Clinicians and public health staff should consider antimicrobial susceptibility testing (AST) on meningococcal isolates to inform prophylaxis decisions if their state has reported a case of meningococcal disease caused by ciprofloxacin-resistant strains within the past 2 years.
- Update prophylaxis practices around N. meningitidis cases as needed based on detection of ciprofloxacin-resistance cases.
- View CDC guidance on changing prophylaxis antibiotics in areas with ciprofloxacin resistance.
- State and territorial health departments are asked to
- Continue submitting all meningococcal isolates to CDC for AST and whole-genome sequencing
- Report any suspected meningococcal treatment or prophylaxis failures
- Complete a supplemental case report form; [2 pages] for cases with isolates determined to be β-lactamase screen-positive or ciprofloxacin-resistant; forms can be submitted to CDC via secure email (meningnet@cdc.gov) or SAMS
Disease trends overall
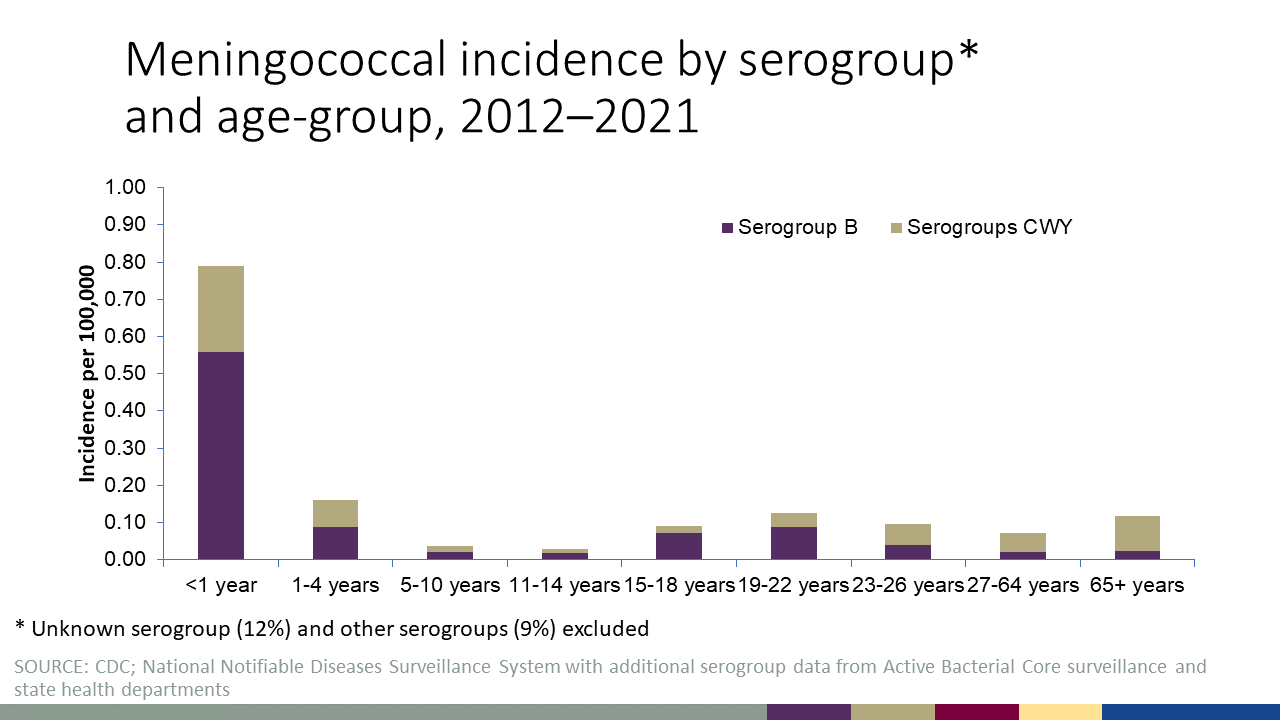
Rates of meningococcal disease have declined sharply in the United States since the 1990s. Anyone can get meningococcal disease, but rates of disease are highest in children younger than 1 year old, followed by a second peak in adolescence. Among adolescents and young adults, those 16 through 23 years old have the highest rates of meningococcal disease). The proportion of cases caused by each serogroup varies by age group (See Figure 2).
Meningococcal disease is also seasonal: the number of cases generally peaks each year in January, February, and March.
Figure 2 shows incidence rates (per 100,000 persons) of meningococcal disease caused by serogroup B compared to serogroups C, W, and Y by age group from 2011 through 2021. Serogroup B caused approximately 60% of cases among children less than 5 years old. Serogroups C, Y, or W caused approximately three in five cases of meningococcal disease among persons 11 years old or older during this time period. View data for this chart.
Surveillance systems

Analyze and visualize ABCs N. meningitidis data using Bact Facts Interactive.
Meningococcal disease is a reportable condition in all states, with cases immediately reported to the local and state health departments. CDC closely tracks meningococcal disease through the National Notifiable Diseases Surveillance System and Active Bacterial Core surveillance.
In 2015, CDC implemented enhanced meningococcal disease surveillance. The goals for this surveillance are to:
- Collect more complete data on key variables for monitoring meningococcal disease epidemiology
- Inform vaccine policy decisions
- Collect meningococcal isolates from a broad and representative population
The health departments of all 50 states and several large jurisdictions now routinely collect enhanced meningococcal disease data and isolates.
The most recent Council of State and Territorial Epidemiologists (CSTE) case classification (2015) for meningococcal disease is:
Suspected
- Clinical purpura fulminans in the absence of a positive blood culture; or
- Gram-negative diplococci, not yet identified, isolated from a normally sterile body site (e.g., blood or cerebrospinal fluid [CSF])
Probable
- Detection of Neisseria meningitidis antigen
- In formalin-fixed tissue by immunohistochemistry (IHC); or
- In CSF by latex agglutination
Confirmed
- Detection of N. meningitidis-specific nucleic acid in a specimen obtained from a normally sterile body site (e.g., blood or CSF), using a validated polymerase chain reaction (PCR) assay; or
- Isolation of N. meningitidis
- From a normally sterile body site (e.g., blood or CSF, or less commonly, synovial, pleural, or pericardial fluid); or
- From purpuric lesions.
Enhanced meningococcal disease surveillance reports
View meningococcal disease data, including case counts and incidence by serogroup and age. Reports also include vaccination history of cases, meningococcal related deaths, incidence by serogroup and college attendance, and HIV status.
- 2022 final surveillance report [2 pages]
- 2021 final surveillance report [2 pages]
- 2020 final surveillance report [2 pages]
- 2019 final surveillance report [2 pages]
- 2018 final surveillance report [2 pages]
- 2017 final surveillance report [2 pages]
- 2016 final surveillance report [2 pages]
- 2015 final surveillance report [2 pages]
- Surveillance manual’s chapter on meningococcal disease
- Active Bacterial Core surveillance reports
(see Neisseria meningitidis)
- Bact Facts interactive
- Health advisory: Ciprofloxacin-resistant, β-lactamase-producing Neisseria meningitidis serogroup Y, United States, 2019–2020