Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data—United States and 6 Dependent Areas, 2021: National Profile

NHSS data presented in this report are based on case data reported to CDC through December 31, 2022, and allow for a 12-month reporting delay and assessment of diagnoses, deaths, and prevalence for the year 2021. The statements in this section, unless otherwise indicated, are based on numbers of 12 or more. Please use caution when interpreting data on diagnosed HIV infection (see Technical Notes for additional information on definitions and data specifications).
Important notes
- Jurisdictions (47 states and the District of Columbia) that reported complete CD4+ T-lymphocyte (CD4) and viral load laboratory results to CDC were included for the analyses that require laboratory data (Tables 1a–4b).
- Data from the 50 states, the District of Columbia, and 6 U.S. dependent areas (where indicated) were used for analyses of prevalence-based HIV care continuum (Table 5); stage 3 (AIDS) at the time of diagnosis of HIV infection (Tables 6a–6d); deaths and survival of persons with diagnosed HIV infection (Tables 7a–8f); and persons with diagnosed, perinatally acquired HIV infection (Tables 10a/b).
- For tables that include data by transmission category, the data were statistically adjusted to account for missing transmission category and the percentages are presented based on ASAB as reported in the tables.
- Please use caution when interpreting data for transgender men, additional gender identity (AGI), American Indian/Alaska Native persons, and Native Hawaiian/other Pacific Islander persons as the percentages and/or rates are based on small numbers.
- Please read all titles and footnotes carefully to ensure a complete understanding of the displayed data. Percentages, not rates, are calculated for the care outcomes. Please note that important points are highlighted with the magnifying glass icon
 and important findings are called to attention with the exclamation icon
and important findings are called to attention with the exclamation icon  in the graphic.
in the graphic.
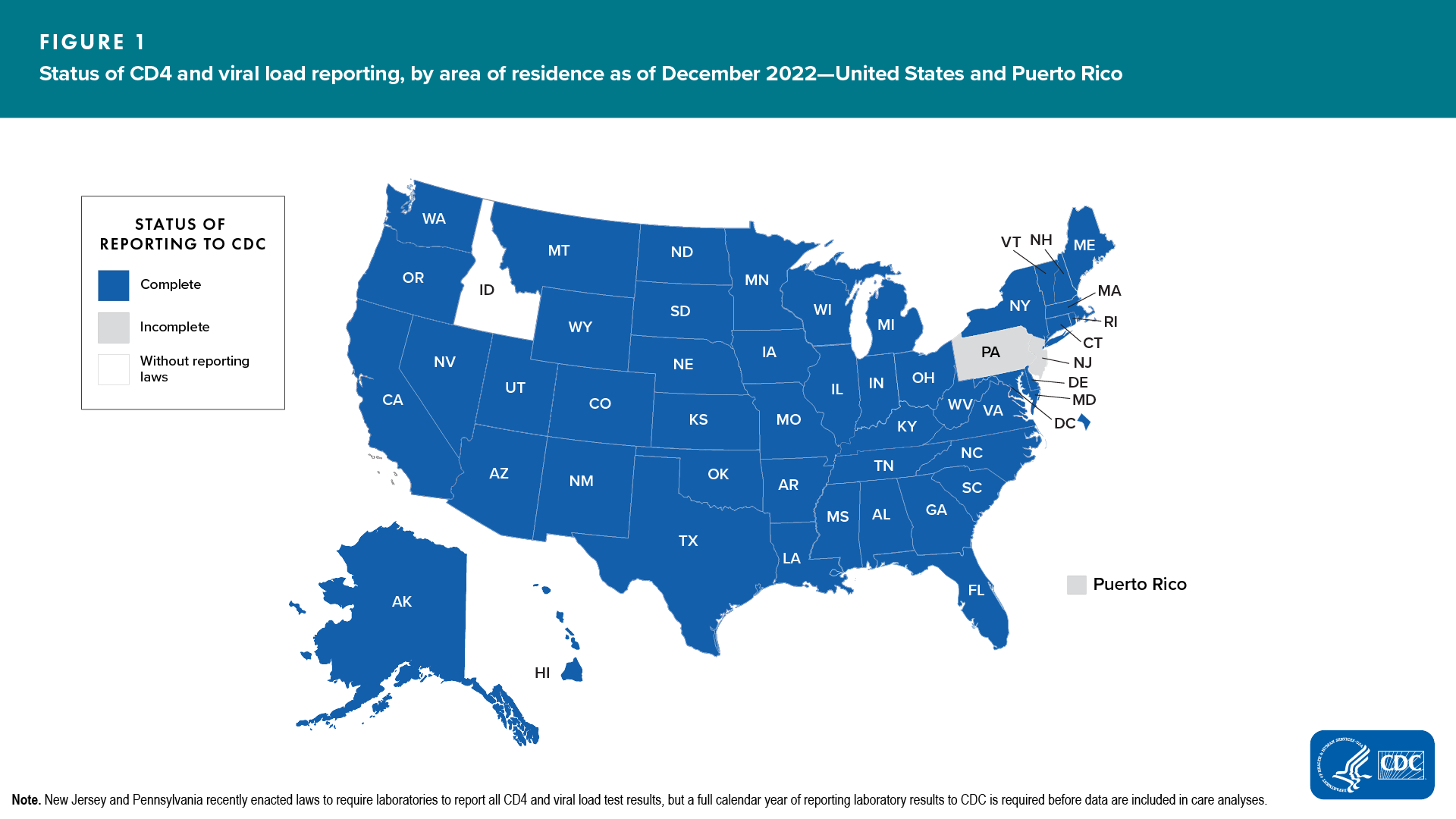
Status of Laboratory Reporting
Monitoring stage of disease at time of diagnosis, linkage to HIV medical care, retention in HIV medical care, and viral suppression (based on NHSS data) is dependent upon complete reporting of HIV-related laboratory results (including CD4 and viral load results; see Technical Notes) to HIV surveillance programs and CDC. Although most jurisdictions have regulations that require laboratories and providers to report at least a subset of CD4 and viral load test results to health departments, not all jurisdictions have mandatory reporting of all levels of CD4 and viral load (i.e., detectable and undetectable) results.
As of December 2022, 48 jurisdictions (47 states and the District of Columbia) had complete laboratory reporting for all data years examined and specimens collected from at least January 2020 through September 2022 (Figure 1). In comparison with the 2020 report, the 2021 report includes data from 2 additional states (Kentucky and Vermont) that met the criteria. Please note that due to incomplete reporting of deaths for the year 2021, data for Mississippi, Guam, U.S. Virgin Islands, and West Virginia should be interpreted with caution.
Diagnosis-Based HIV Care Continuum—Overview
The diagnosis-based HIV care continuum describes each step of the continuum as a percentage of the number of people living with diagnosed HIV. The denominator is the number of persons aged ≥ 13 years living with diagnosed HIV infection at year-end 2021.
Note. Denominator for stage of disease, linkage to care within 1 month, and viral suppression within 6 months of diagnosis is limited to people with HIV diagnosed in a single year.
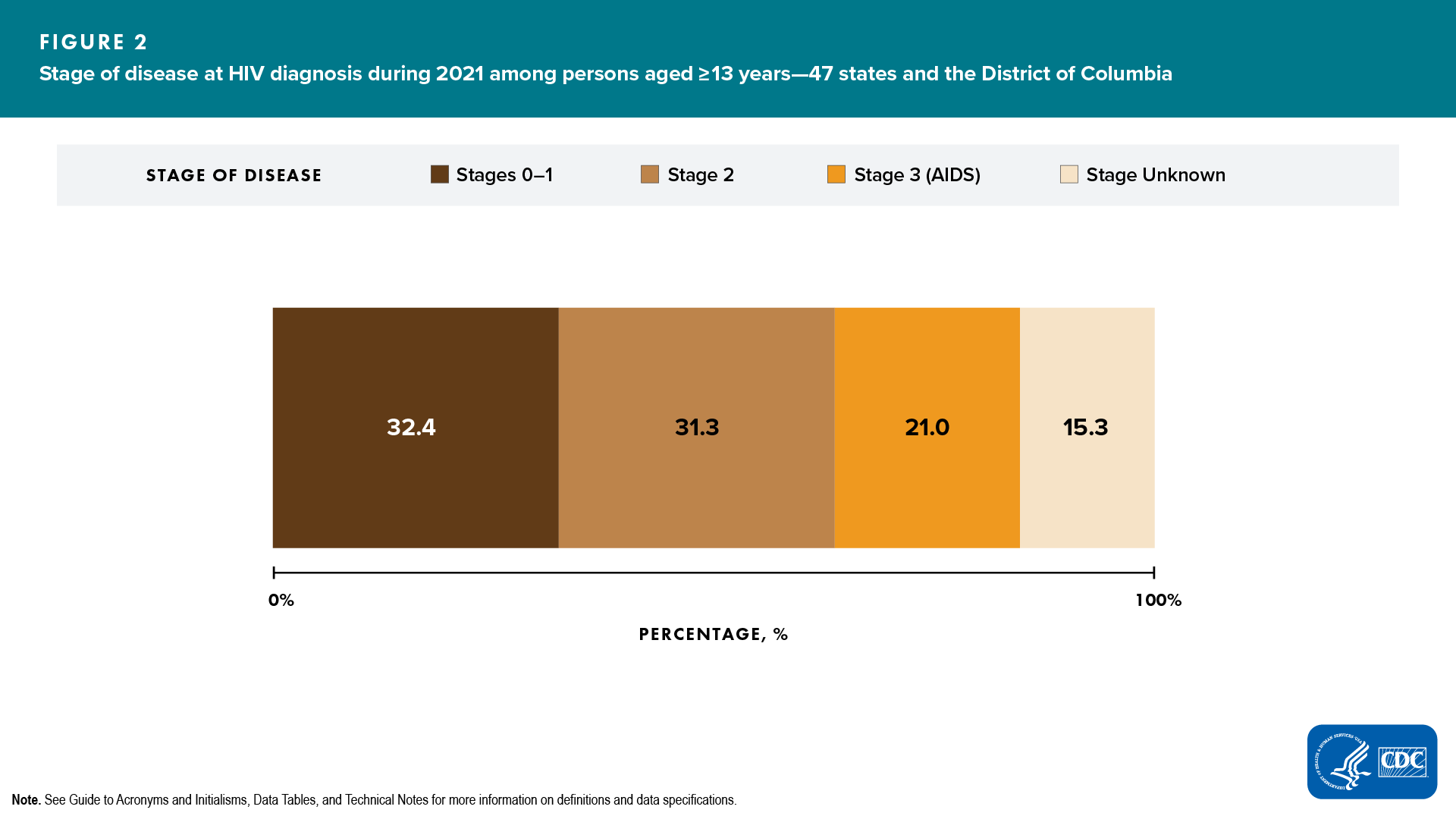
Stage of disease at time of diagnosis of HIV infection
Among 33,606 persons aged ≥ 13 years with HIV infection diagnosed during 2021 in 48 jurisdictions with complete reporting of laboratory data to CDC, the stage of disease at time of diagnosis was classified as follows: stage 0 (7.1%), stage 1 (25.3%), stage 2 (31.3%), stage 3 (AIDS) (21.0%), and stage unknown (15.3%). Overall, a higher percentage of persons had HIV diagnosed at an earlier stage (stages 0 or 1, 32.4%) than at the late stage (stage 3 [AIDS]: 21.0%) (Figure 2, Table 1a).
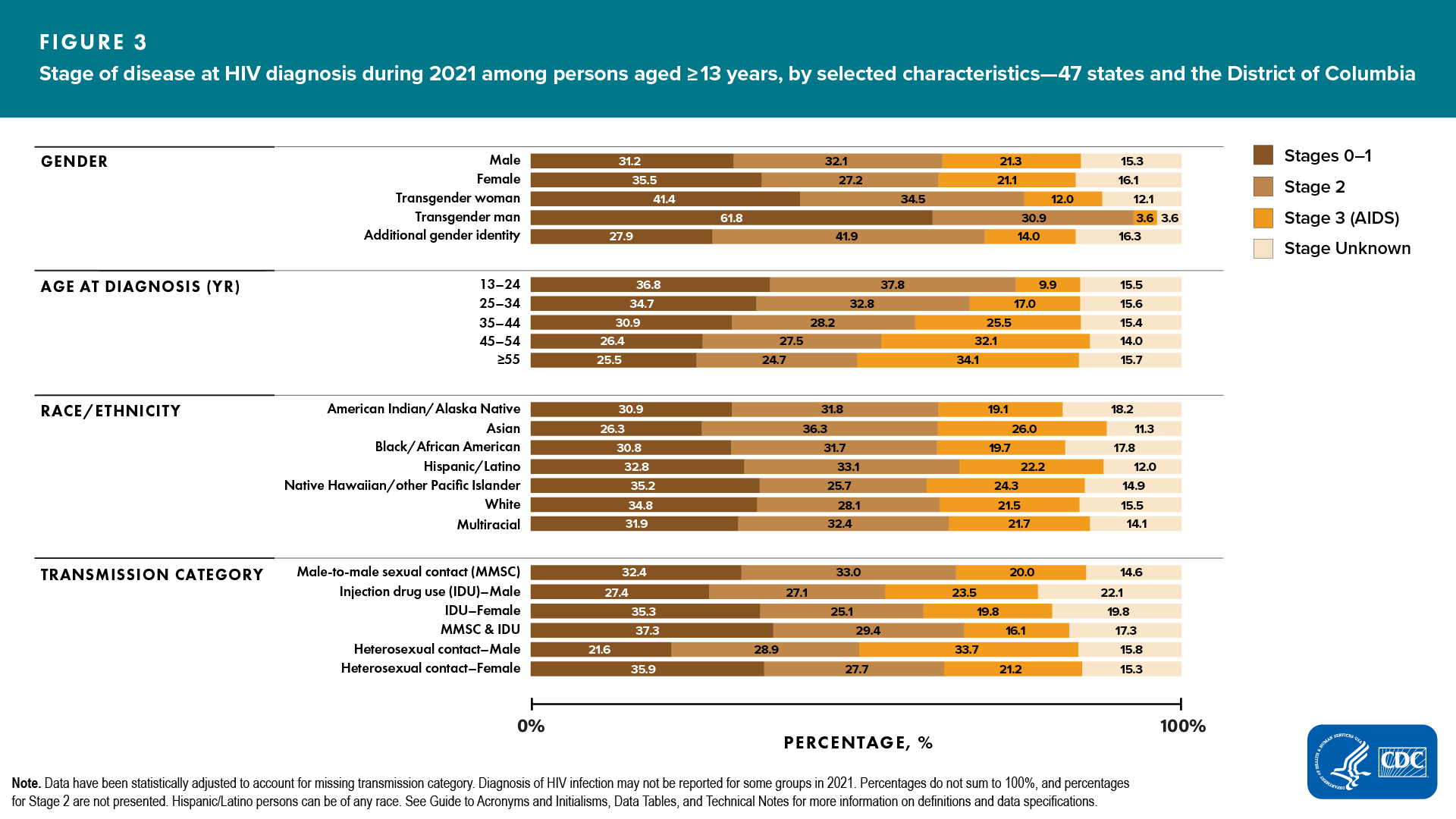
Percentage of persons with HIV diagnosed at an earlier stage (0 or 1) compared to the percentage with a late-stage diagnosis, respectively, by selected characteristics, were as follows (Figure 3, Table 1a):
Gender
- Male―31.2% vs 21.3%
- Female―35.5% vs 21.1%
- Transgender women―41.4% vs 12.0%
- Transgender men―61.8% vs 3.6%
- AGI―27.9% vs 14.0%
Age group
- 13–24 years―36.8% vs 9.9%
- 25–34 years―34.7% vs 17.0%
- 35–44 years―30.9% vs 25.5%
- 45–54 years―26.4% vs 32.1%

- ≥ 55 years―25.5% vs 34.1%

Race/ethnicity
- American Indian/Alaska Native―30.9% vs 19.1%
- Asian―26.3% vs 26.0%
- Black/African American―30.8% vs 19.7%
- Hispanic/Latino―32.8% vs 22.2%
- Native Hawaiian/other Pacific Islander―35.2% vs 24.3%
- White―34.8% vs 21.5%
- Multiracial―31.9% vs 21.7%
ASAB and transmission category
- Among males
- MMSC―32.4% vs 20.0%
- IDU―27.4% vs 23.5%
- MMSC and IDU―37.3% vs 16.1%
- Heterosexual contact―21.6% vs 33.7%

- Among females
- IDU―35.3% vs 19.8%
- Heterosexual contact―35.9% vs 21.2%
Six areas had an equivalent or higher percentage of persons who received a late-stage diagnosis compared to the percentage that received an earlier-stage diagnosis, respectively (Table 1b): ![]()
- Alaska―33.3% vs 33.3%
- Delaware―29.7% vs 30.9%
- Maine―22.6% vs 45.2%
- Mississippi―20.0% vs 20.8%
- South Dakota―38.7% vs 29.0%
- Vermont―41.6% vs 41.7%
Linkage to HIV medical care within 1 month and viral suppression within 6 months after diagnosis of HIV infection

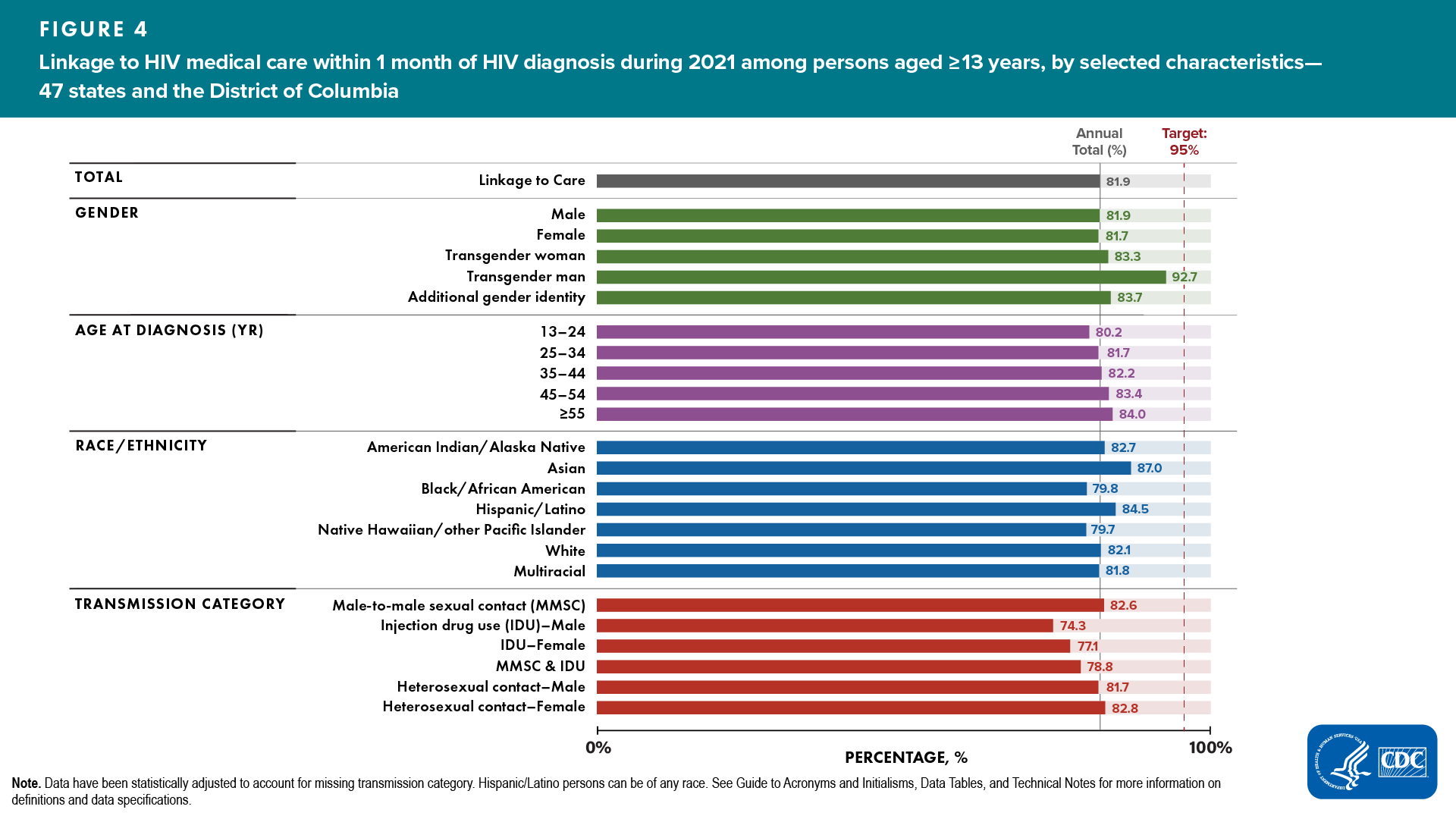
Linkage to HIV medical care
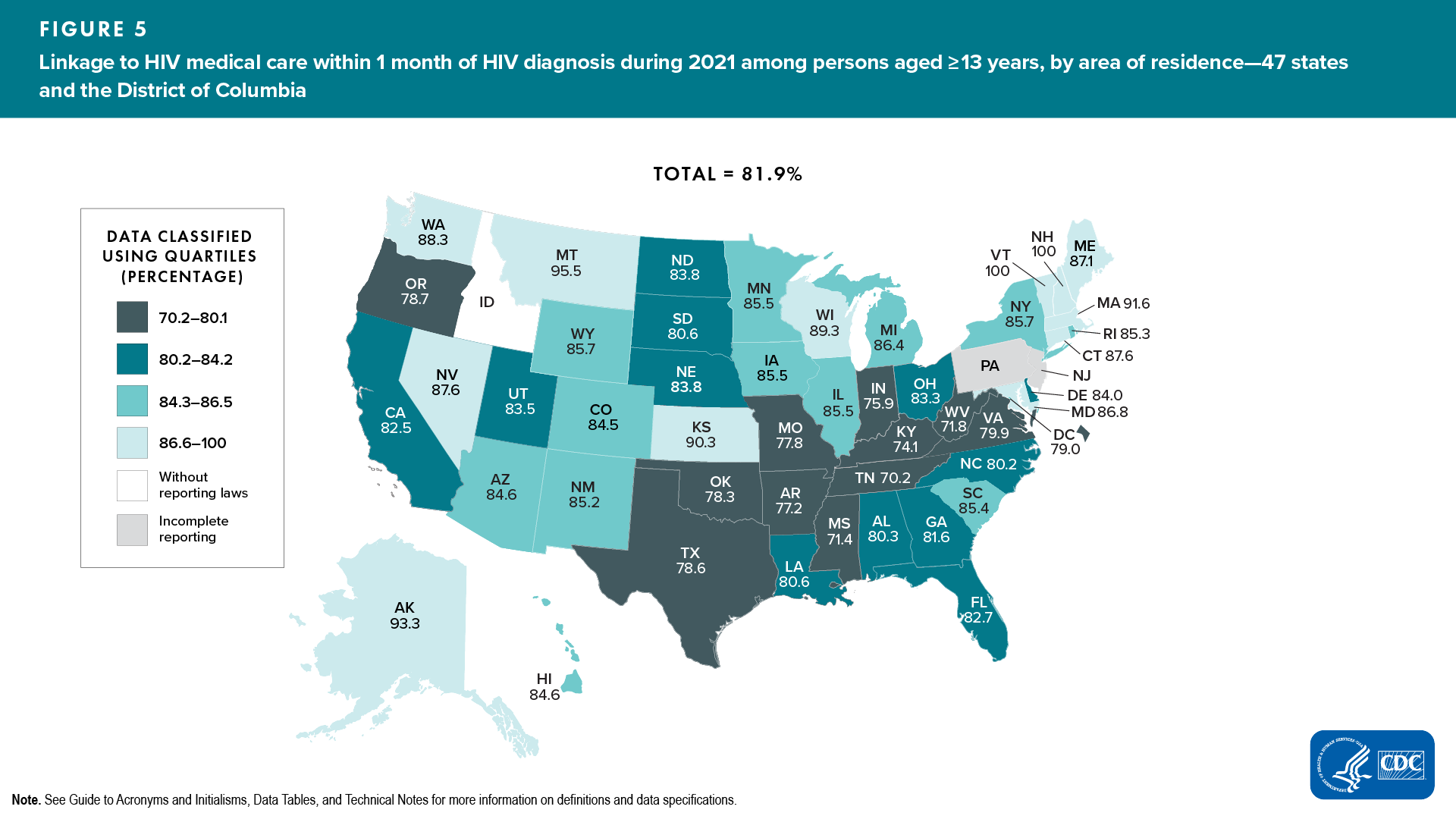
Among 33,606 persons with HIV infection diagnosed during 2021 in the 48 jurisdictions with complete reporting of laboratory data to CDC, 81.9% were linked to HIV medical care within 1 month of diagnosis (Table 2a).
Lowest percentages of persons linked to HIV medical care, by selected characteristics, were as follows (Figure 4, Table 2a):
- Gender—females (81.7%)
- Age group—aged 13–24 years (80.2%)
- Race/ethnicity—Native Hawaiian/other Pacific Islander (79.7%) and Black/African American (79.8%)

- ASAB and transmission category
- Male—IDU (74.3%)

- Female—IDU (77.1%)

- Male—IDU (74.3%)
![]() A closer look at linkage to HIV medical care within 1 month of diagnosis reveals that among 33,606 persons with HIV infection diagnosed during 2021, no demographic group or group with infection attributed to any of the transmission categories met the forthcoming EHE target of 95% by 2025 (Figure 4, Table 2a).
A closer look at linkage to HIV medical care within 1 month of diagnosis reveals that among 33,606 persons with HIV infection diagnosed during 2021, no demographic group or group with infection attributed to any of the transmission categories met the forthcoming EHE target of 95% by 2025 (Figure 4, Table 2a).
Areas with the lowest percentages of persons linked to HIV medical care were as follows (Figure 5, Table 2b):
- Quartile ≤ 80.1%―Arkansas, Indiana, Kentucky, Mississippi, Missouri, Oklahoma, Oregon, Tennessee, Texas, Virginia, West Virginia, and the District of Columbia
Viral suppression within 6 months

Among 33,606 persons with HIV infection diagnosed during 2021 in the 48 jurisdictions with complete reporting of laboratory data to CDC, viral load was suppressed in 69.0% of persons within 6 months of HIV diagnosis (Table 2a).
Lowest percentages of viral suppression ≤ 6 months after HIV diagnosis were as follows (Table 2a):
- Gender—AGI (67.4%)
- Age group—aged ≥ 55 years (66.7%)
- Race/ethnicity—American Indian/Alaska Native (65.5%)
- ASAB and transmission category
- Male—IDU (51.2%)
- Female—IDU (53.8%)
Areas with the lowest percentages of persons with viral suppression were as follows (Table 2b):
- Quartile ≤ 68.3%—Alabama, Arkansas, California, Georgia, Kentucky, Maryland, Mississippi, Oklahoma, South Dakota, Tennessee, Texas, West Virginia, and the District of Columbia
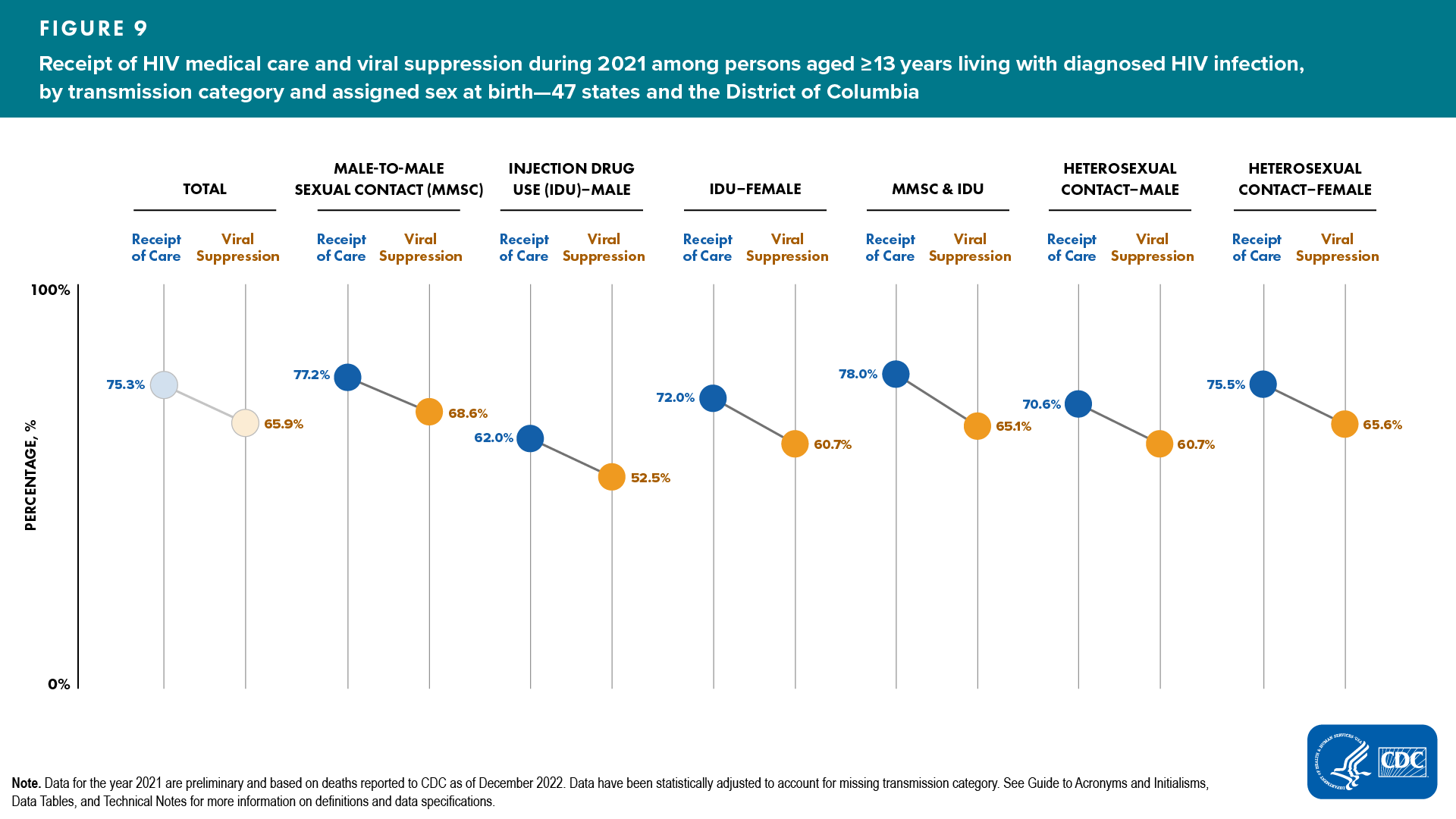
Receipt of HIV medical care and viral suppression

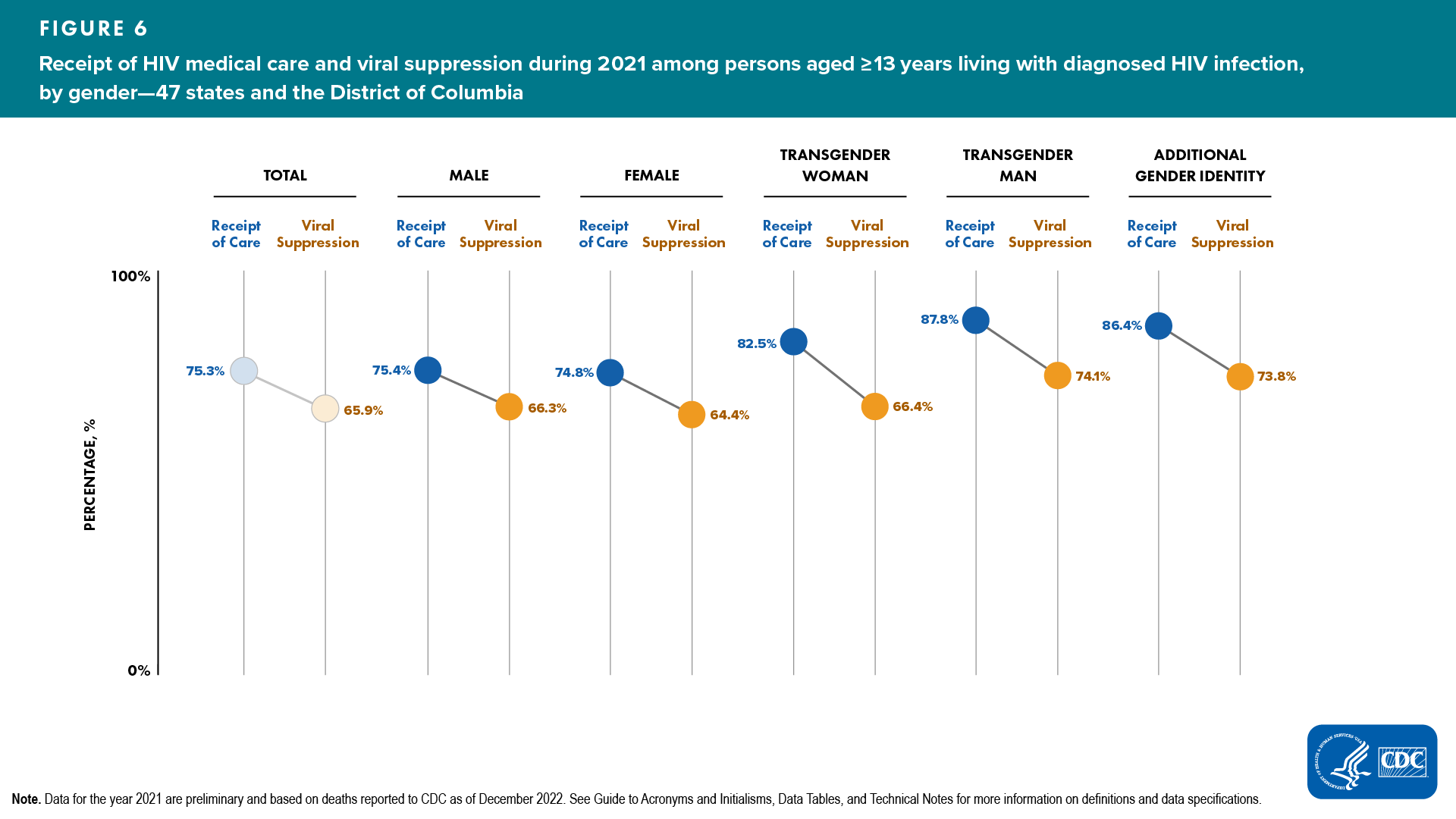
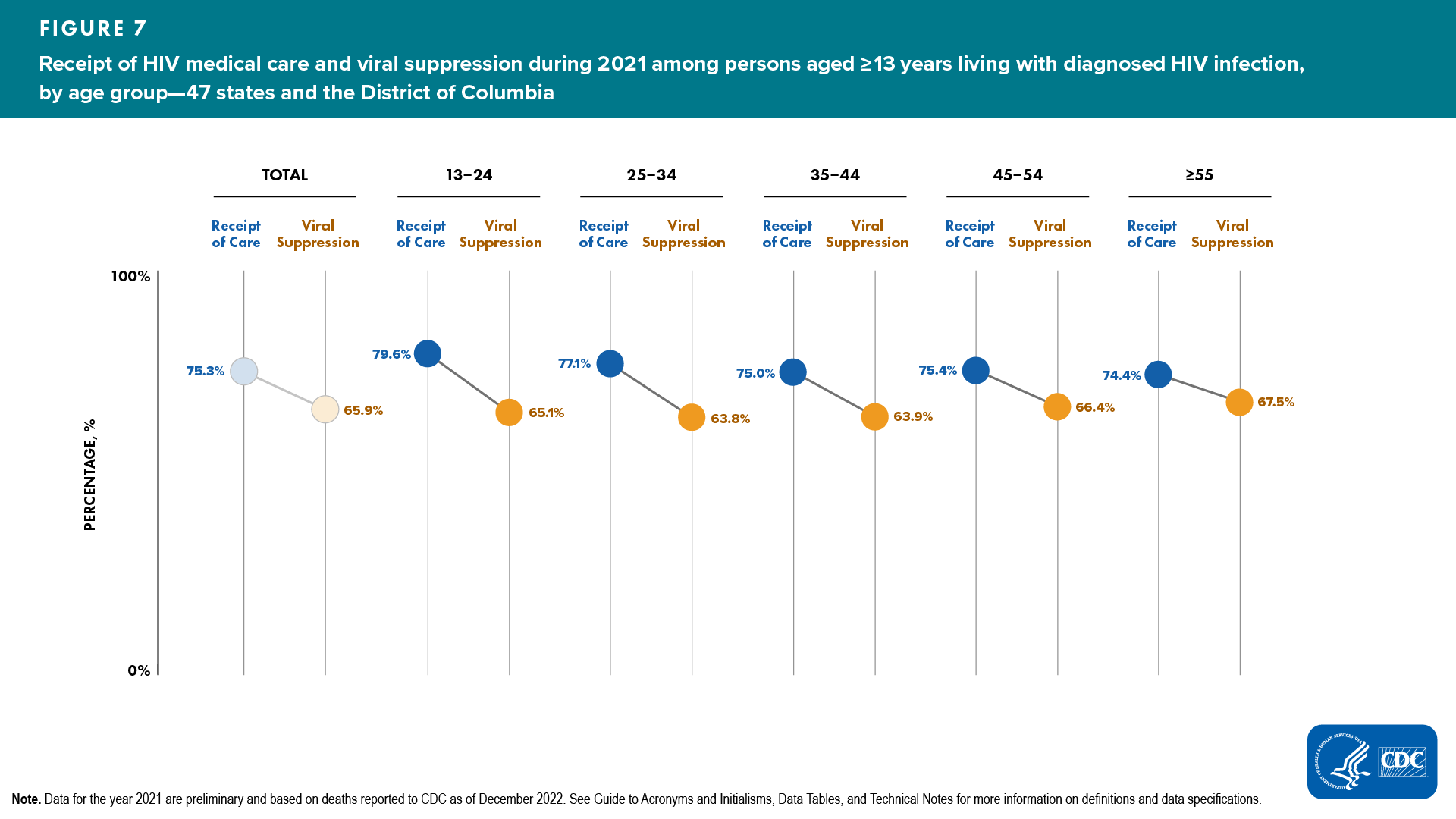
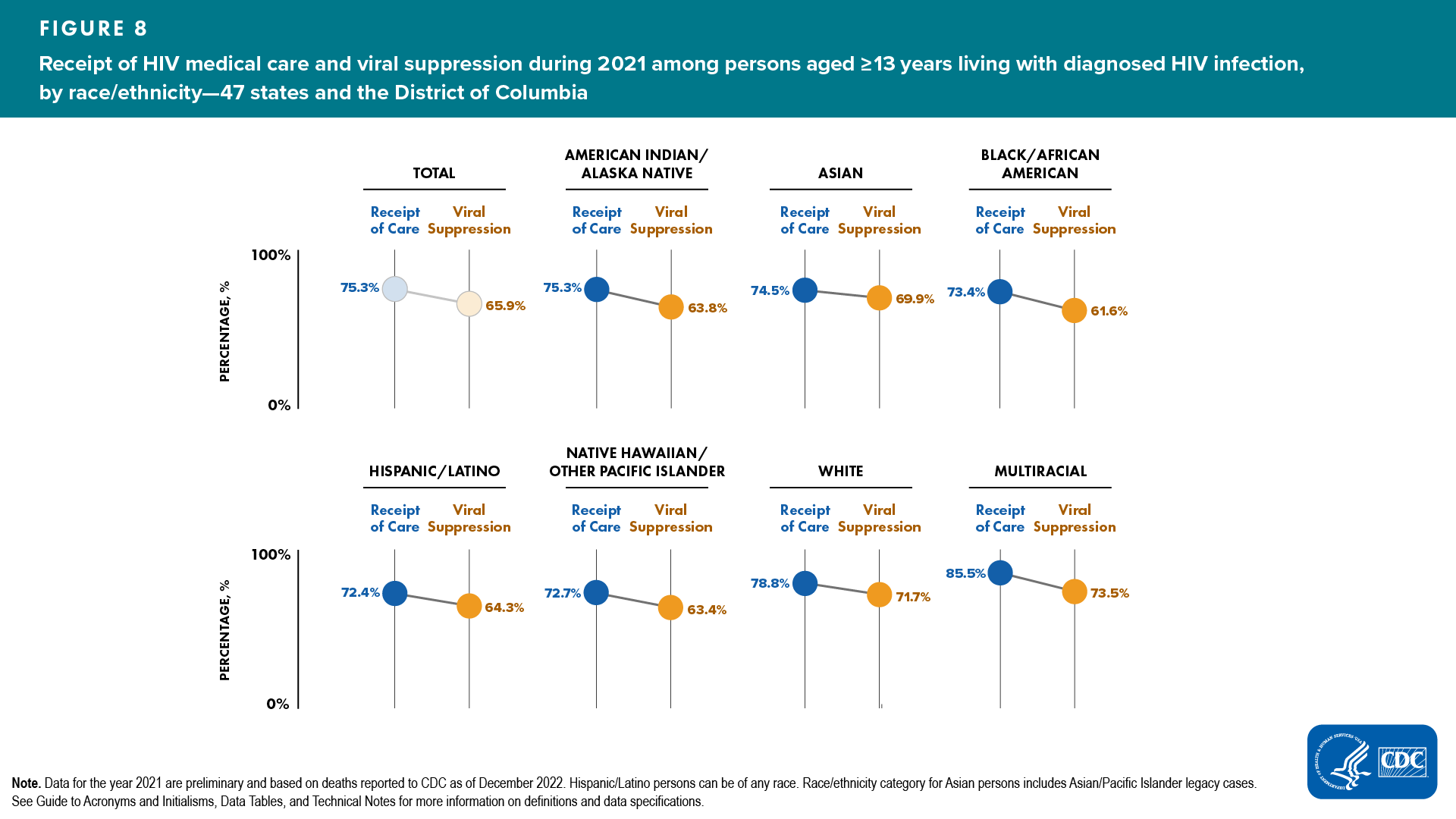
During 2021, 75.3% of 964,002 persons alive at year-end 2021 received any HIV medical care (at least 1 CD4 or viral load test), 53.9% of persons were retained in HIV medical care (at least 2 CD4 or viral load test), and 65.9% of persons had viral suppression at the most recent viral load test in 48 jurisdictions with complete reporting of laboratory data to CDC (Tables 3a and 4a).
Lowest percentages of persons who received any HIV medical care among those aged ≥ 13 years living with diagnosed HIV infection, by selected characteristics, were as follows (Figures 6–9, Table 3a):
- Gender—females: 74.8%
- Age group—aged ≥ 55 years: 74.4%
- Race/ethnicity—Hispanic/Latino: 72.4%
- ASAB and transmission category
- Male—IDU: 62.0%
- Female—IDU: 72.0%
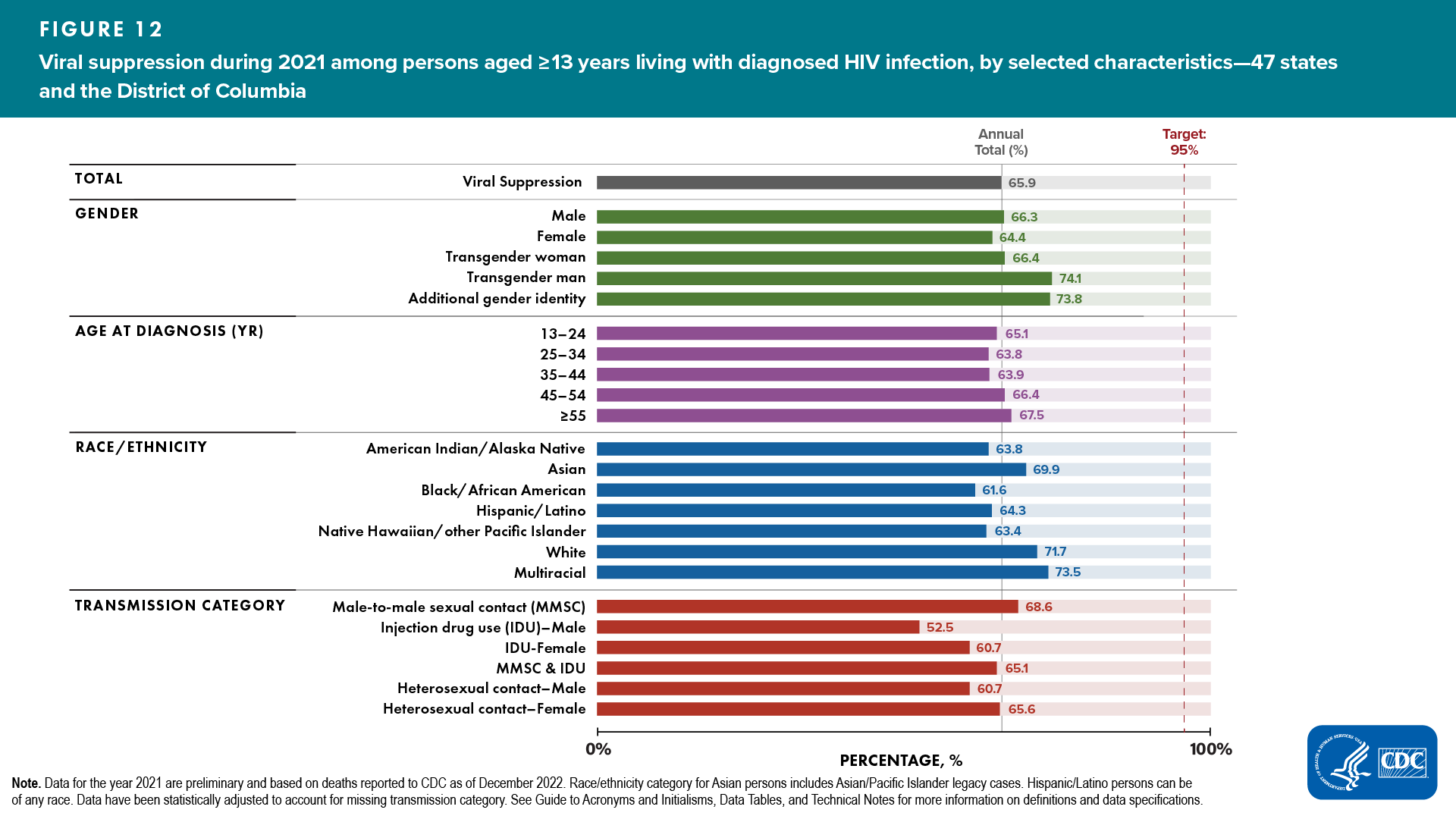
Lowest percentages of persons who had viral suppression at the most recent viral load test among those aged ≥ 13 years living with diagnosed HIV infection, by selected characteristics, were as follows (Figures 6–9, Table 3a):
- Gender—females: 64.4%
- Age group—aged 25–34 years: 63.8%
- Race/ethnicity—Black/African American: 61.6%
- ASAB and transmission category
- Male—IDU: 52.5%
- Female—IDU: 60.7%
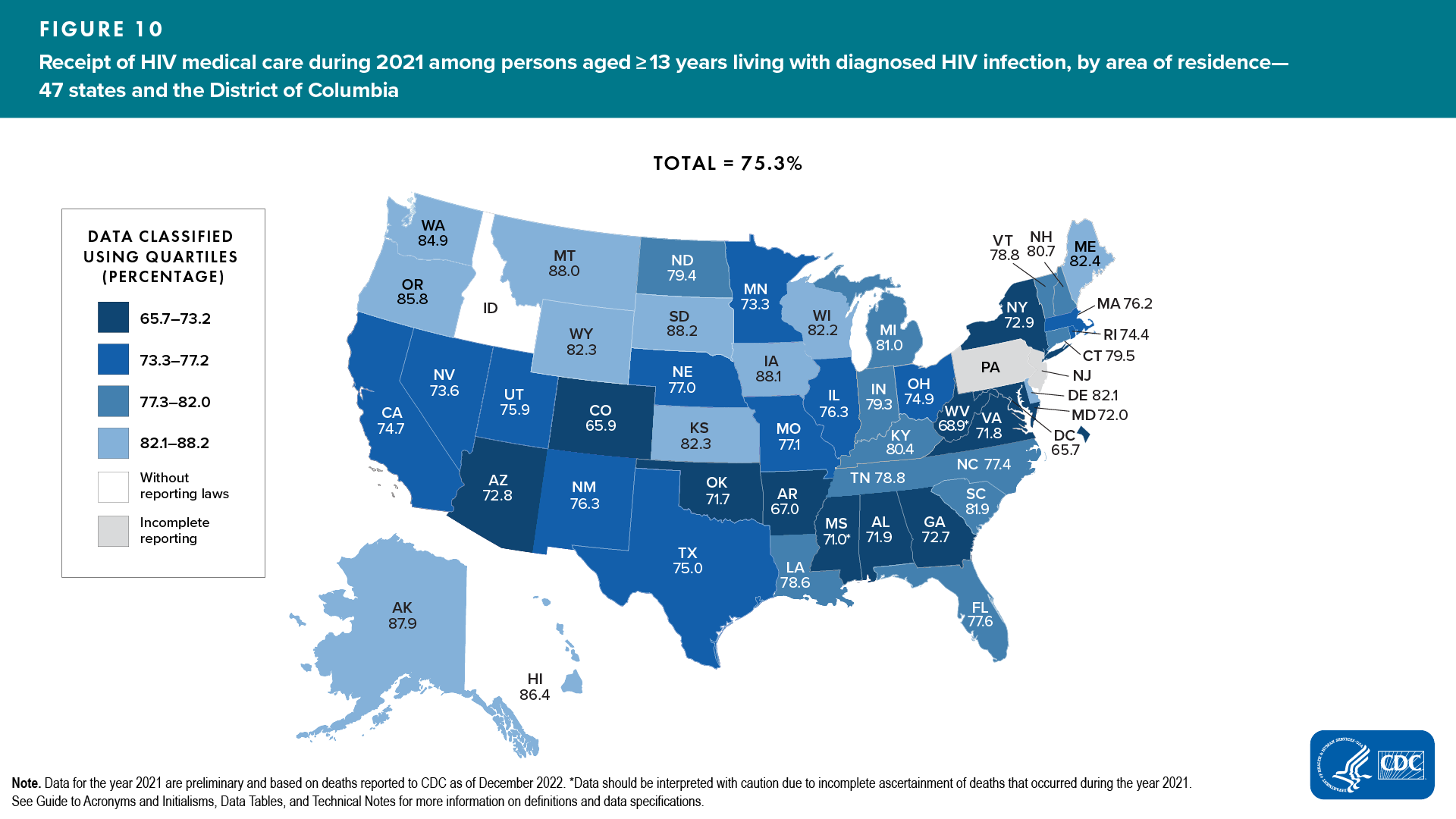
Areas with the lowest percentages of persons who received HIV medical care were as follows (Figure 10, Table 3b):
- Quartile ≤ 73.2%―Alabama, Arizona, Arkansas, Colorado, Georgia, Maryland, Mississippi, New York, Oklahoma, Virginia, West Virginia, and the District of Columbia
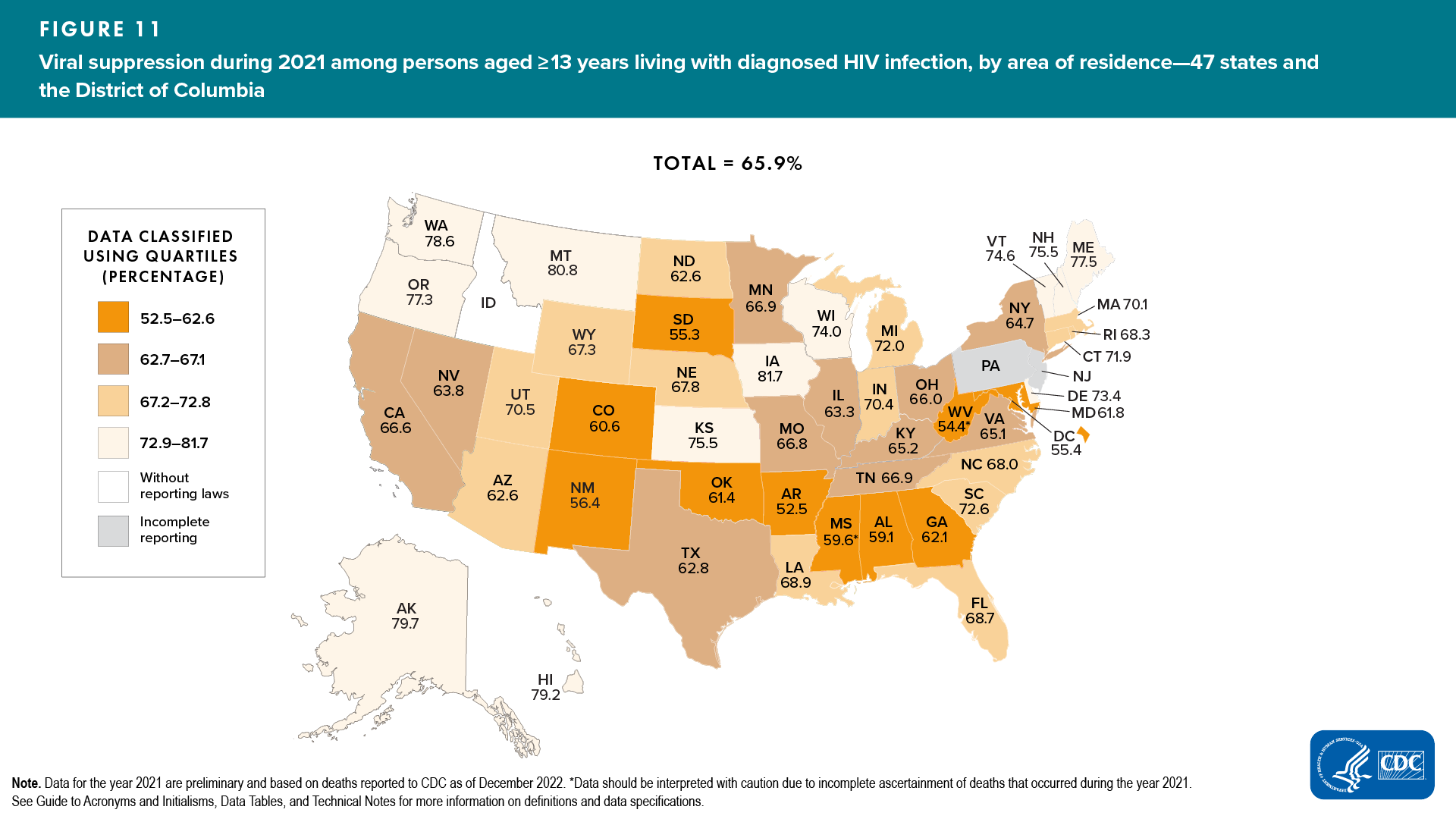
Areas with the lowest percentages of persons who had viral suppression were as follows (Figure 11, Table 3b):
- Quartile ≤ 62.6%―Alabama, Arizona, Arkansas, Colorado, Georgia, Maryland, Mississippi, New Mexico, North Dakota, Oklahoma, South Dakota, West Virginia, and the District of Columbia
![]() A closer look at viral suppression at the most recent viral load test reveals that among 964,002 persons aged ≥ 13 years living with diagnosed HIV infection at year-end 2021, no demographic group or group with infection attributed to any of the transmission categories met the forthcoming EHE target of 95% by 2025 (Figure 12, Table 4a).
A closer look at viral suppression at the most recent viral load test reveals that among 964,002 persons aged ≥ 13 years living with diagnosed HIV infection at year-end 2021, no demographic group or group with infection attributed to any of the transmission categories met the forthcoming EHE target of 95% by 2025 (Figure 12, Table 4a).
Prevalence-based HIV Care Continuum—Overview
The Prevalence-based HIV Care Continuum describes each step of the continuum as a percentage of the total number of people living with HIV (diagnosed or undiagnosed). The denominator is the estimated number of persons aged ≥ 13 years living with diagnosed or undiagnosed HIV infection at year-end 2021 (calculated by using the first CD4 test after HIV diagnosis and a CD4 depletion model indicating disease progression). The numerator is extrapolated from the 48 jurisdictions with complete CD4 and viral load reporting (apply the percentage from 48 jurisdictions for receipt of care, retention in care, and viral suppression to the total number of people living with diagnosed HIV in the United States). For more information on Definitions and Data Specifications, see Technical Notes.
Uses of the prevalence-based continuum include monitoring testing efforts in the United States and demonstrating the importance of diagnosing HIV infections to achieve viral suppression, monitoring how the United States is doing among all persons living with HIV, and comparing United States data to other countries who monitor the continuum among all persons living with HIV.
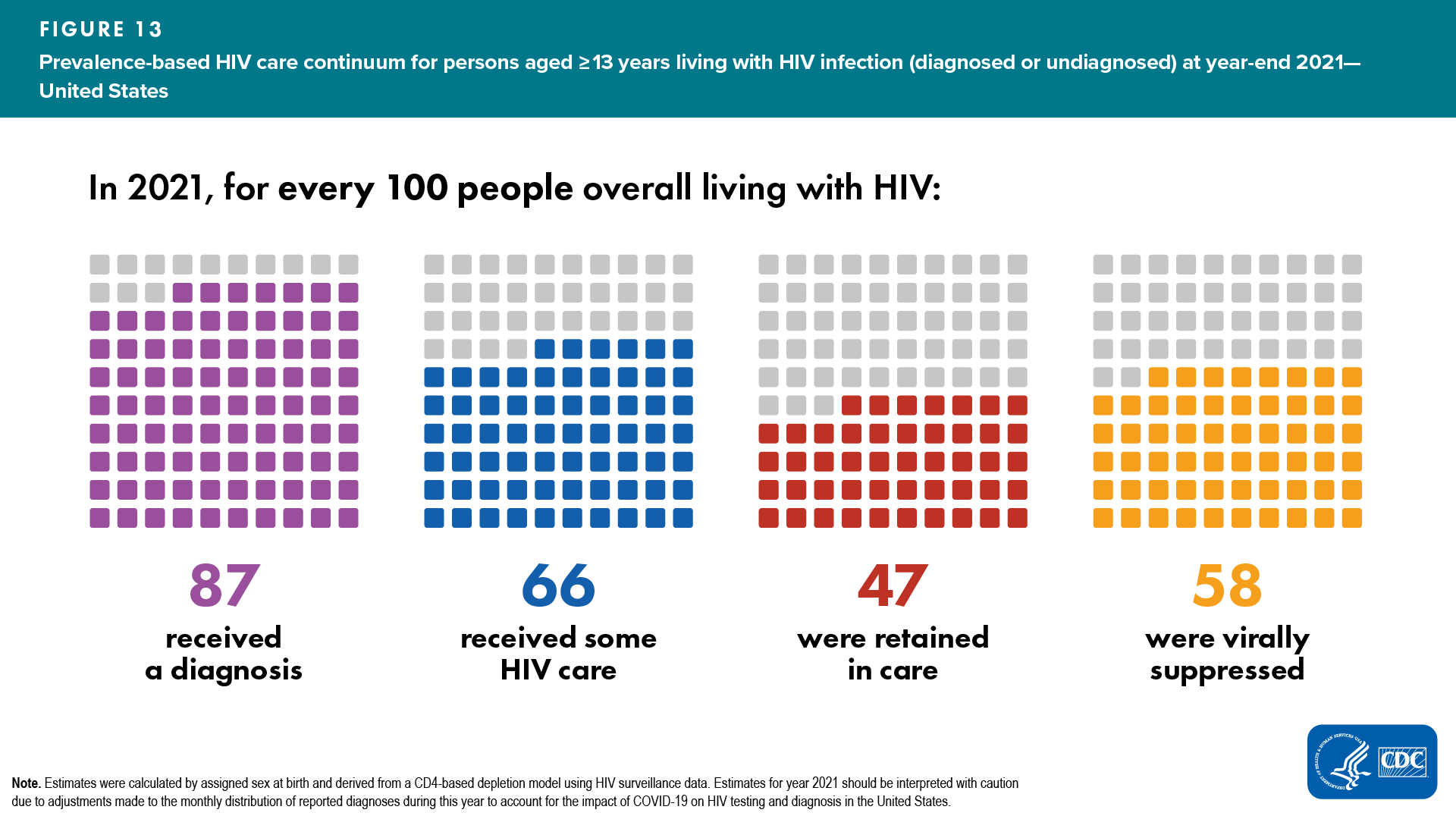
Among the estimated 1.2 million people living with HIV in the United States, 87% received a diagnosis, 66% received HIV medical care, 47% were retained in HIV medical care, and 58% were virally suppressed in 2021 (Figure 13, Table 5). A higher percentage of females received a diagnosis, received HIV medical care in 2021, were retained in HIV medical care, and were virally suppressed than males (females: 90%, 67%, 49%, 58%; males: 86%, 65%, 47%, 57%; Table 5).
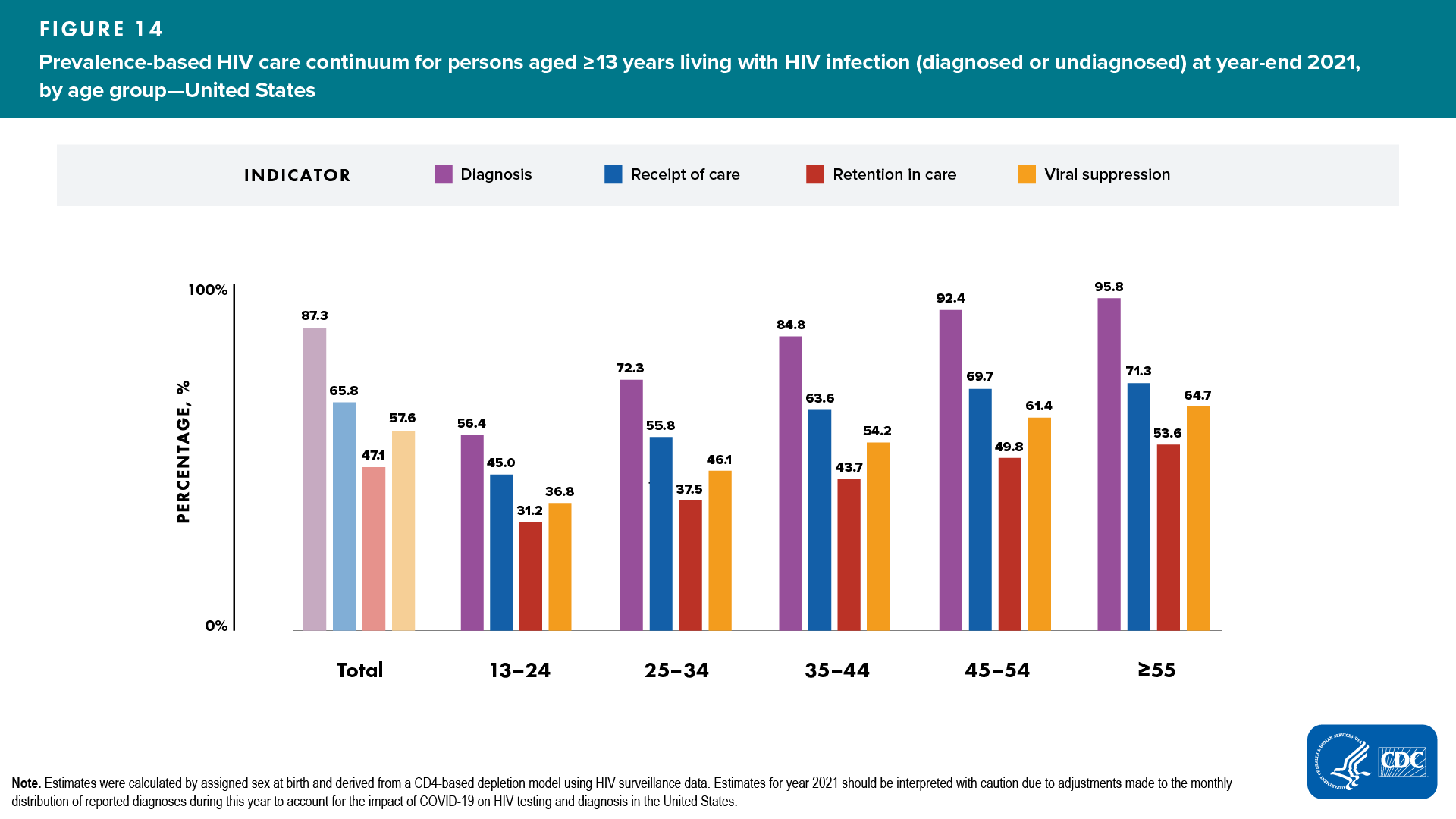
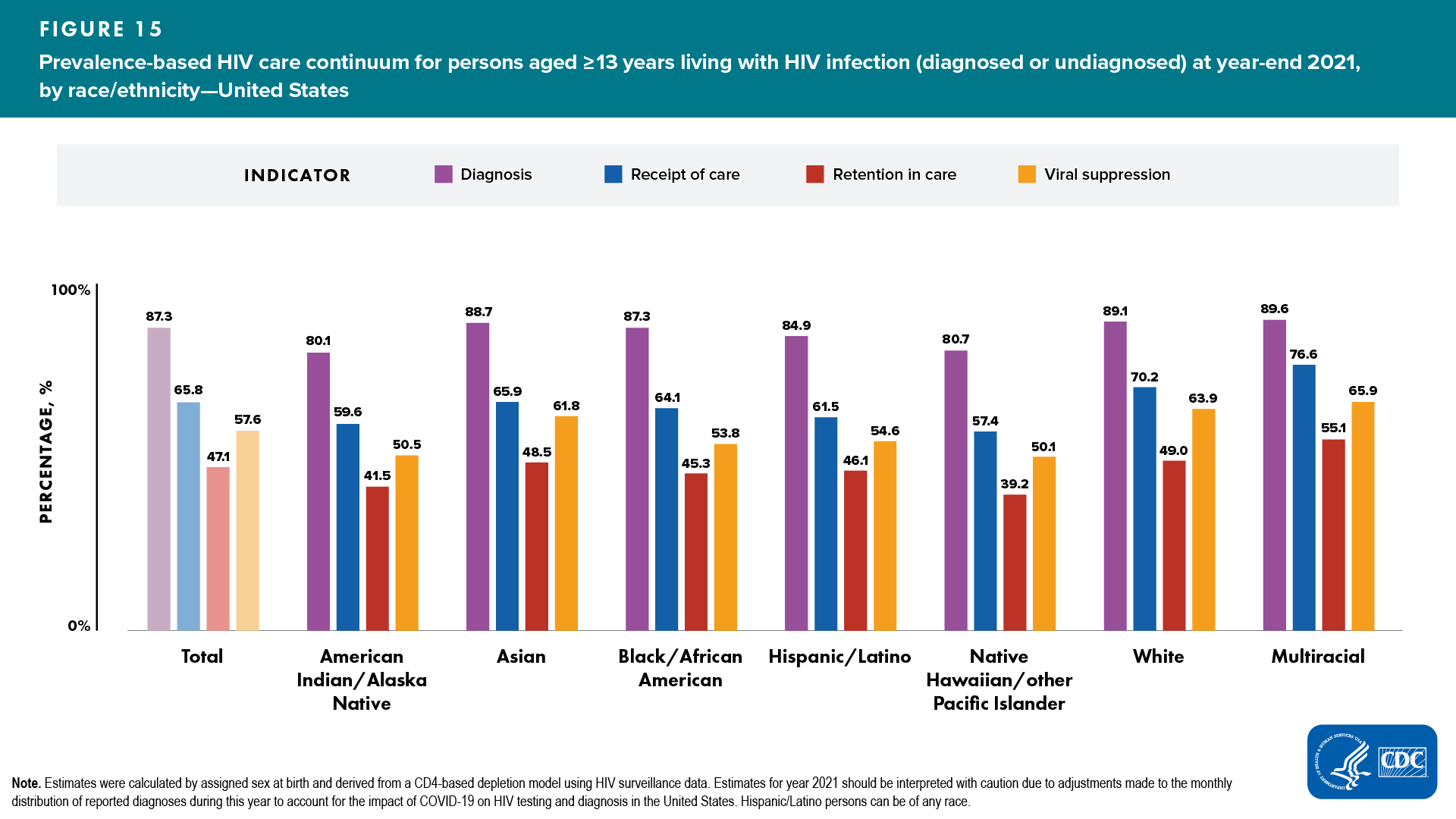
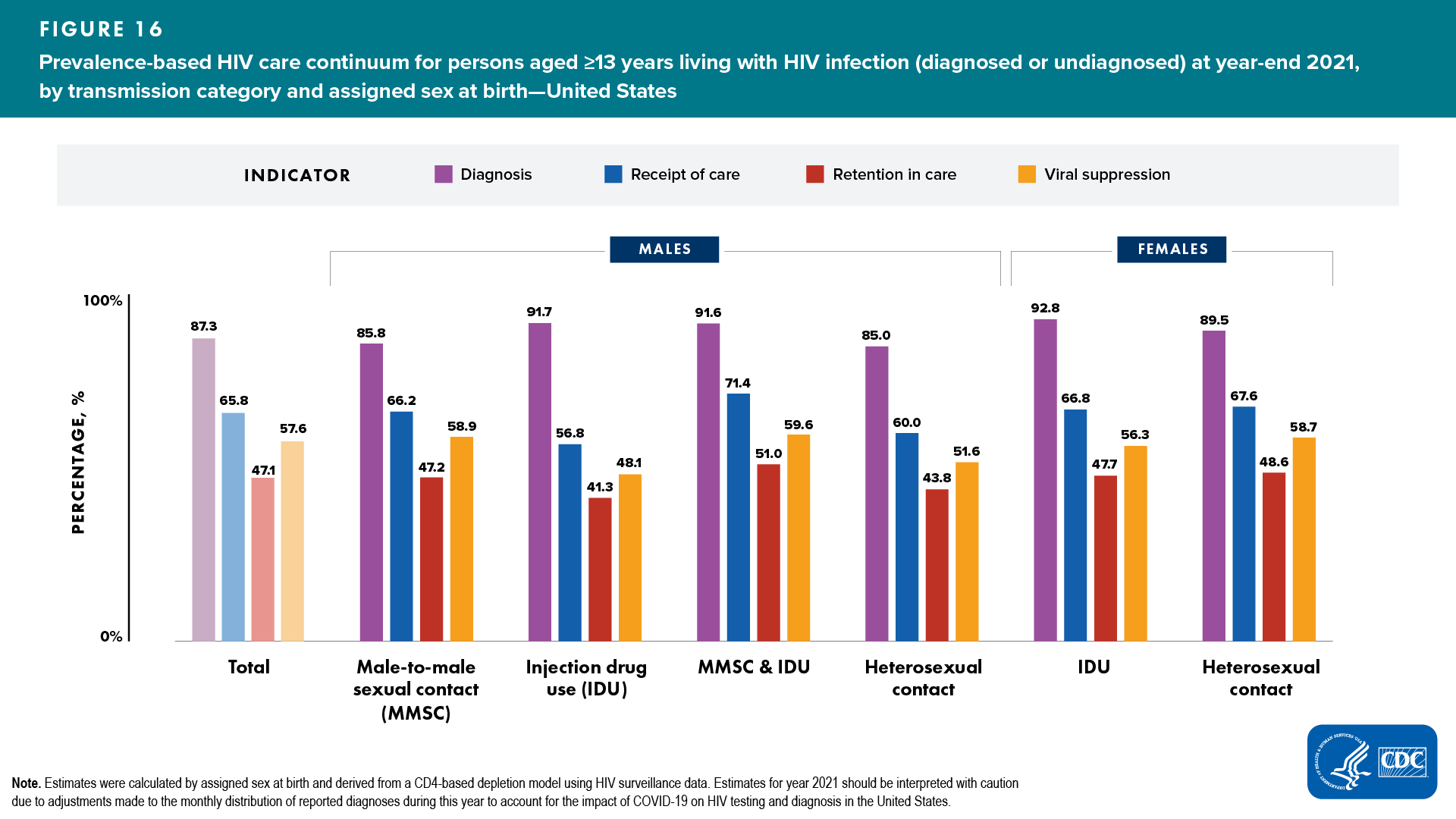
Among persons living with HIV infection (diagnosed or undiagnosed), the lowest percentages that received a diagnosis, received HIV medical care, were retained in HIV medical care, and had viral suppression, by selected characteristics, were as follows (Figures 14–16, Table 5):
Receipt of diagnosis
- Age group—aged 13‒24 years (56%)
- Race/ethnicity—American Indian/Alaska Native (80%)
- ASAB and transmission category
- Male—heterosexual contact (85%)
- Female—heterosexual contact (90%)
Receipt of care
- Age group—aged 13‒24 years (45%)
- Race/ethnicity—Native Hawaiian/other Pacific Islander (57%)
- ASAB and transmission category
- Male—IDU (57%)
- Female—IDU (67%)
Retention in care
- Age group—aged 13‒24 years (31%)
- Race/ethnicity—Native Hawaiian/other Pacific Islander (39%)
- ASAB and transmission category
- Male—IDU (41%)
- Female—IDU (48%)
Viral suppression
- Age group—aged 13‒24 years (37%)
- Race/ethnicity—American Indian/Alaska Native and Native Hawaiian/other Pacific Islander (50%)
- ASAB and transmission category
- Male—IDU (48%)
- Female—IDU (56%)
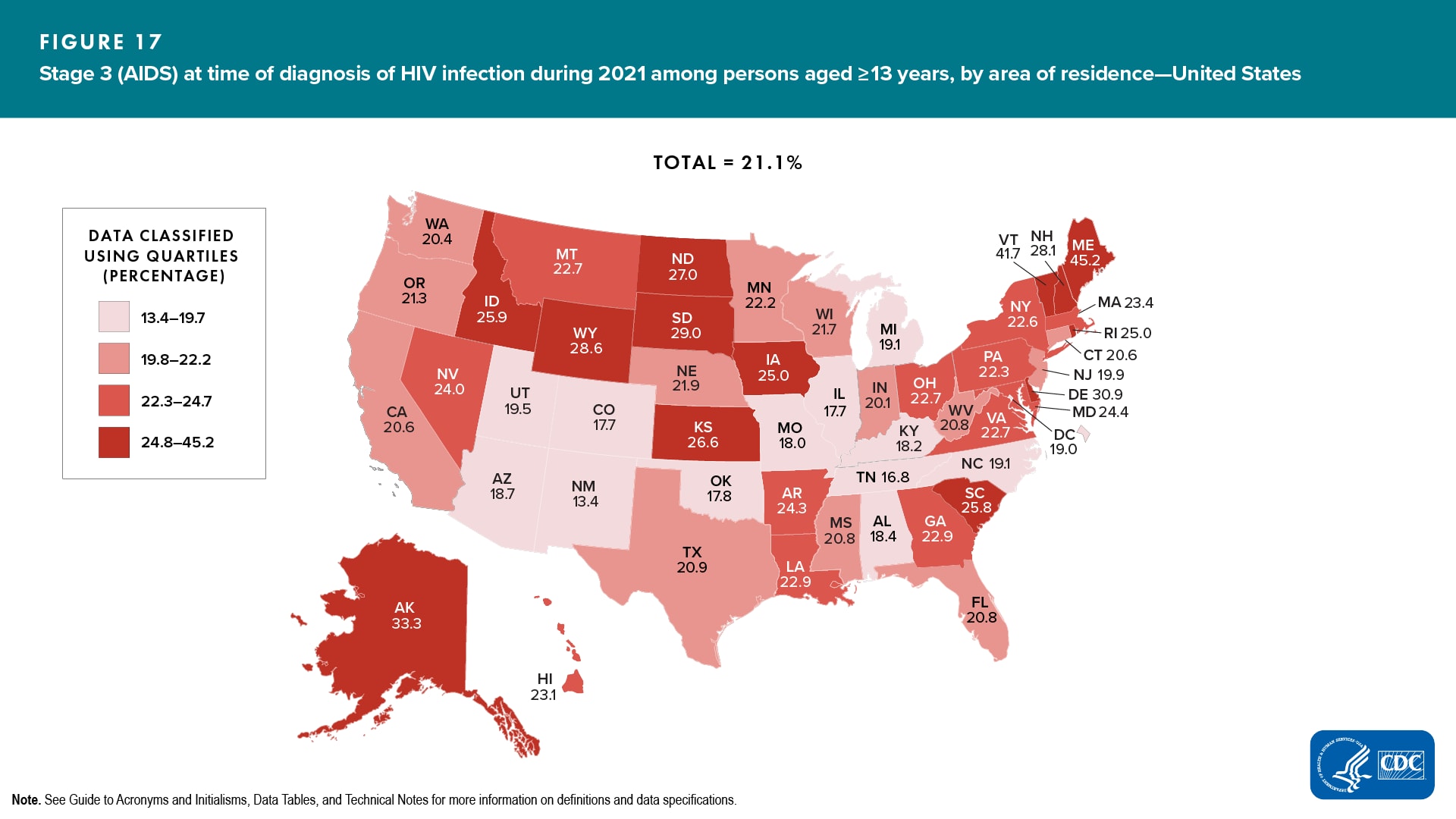
Stage 3 (AIDS) at Time of Diagnosis of HIV Infection, Deaths (Any Cause), and Survival after Diagnosis of HIV Infection
Data from the 50 states, the District of Columbia, and 6 U.S. dependent areas (where indicated) were used for analyses of stage 3 (AIDS) at the time of diagnosis of HIV infection (even when not all CD4 values are reportable), and deaths and survival of persons aged ≥ 13 years with diagnosed HIV infection.
Stage 3 (AIDS) classification at time of diagnosis of HIV infection
Among the 35,716 persons who received an HIV diagnosis during 2021 in the United States, more than 1 in 5 persons (21.1%) received a late-stage diagnosis (stage 3 [AIDS]) (Table 6a).
Highest percentages of a late-stage diagnosis were as follows (Table 6a): ![]()
- Gender—males (21.3%)
- Age group—aged ≥ 55 years (34.2%)
- Race/ethnicity—Asian (25.5%)
- ASAB and transmission category
- Male—heterosexual contact (33.5%)
- Female—heterosexual contact (21.3%)
- Region of residence—Northeast (22.2%)
- Population area of residence—Nonmetropolitan areas (26.4%)
Areas with the highest percentages of persons who received a late-stage diagnosis were as follows (Figure 17, Table 6c):
- Quartile ≥ 24.8%—Alaska, Delaware, Idaho, Iowa, Kansas, Maine, New Hampshire, North Dakota, Rhode Island, South Carolina, South Dakota, Vermont, and Wyoming
Deaths (any cause)
Annual rates of death (any cause) among persons aged ≥ 13 years were calculated per 100,000 population and per 1,000 persons with diagnosed HIV infection or with infection ever classified as stage 3 (AIDS). Age-adjusted rates per 100,000 population and per 1,000 persons with diagnosed HIV infection or with infection ever classified as stage 3 (AIDS) were also calculated and are presented by area of residence (Tables 7a–f).
In 2021, the age-adjusted rates in the United States were as follows:
- Among persons with diagnosed HIV infection―7.0 per 100,000 population and 18.0 per 1,000 persons (Table 7a)
- Among persons with stage 3 (AIDS) classification―5.3 per 100,000 population and 27.0 per 1,000 persons (Table 7d)
Survival for > 3 years after receiving a diagnosis of HIV infection or a Stage 3 (AIDS) classification
In the United States and 6 dependent areas, survival for > 3 years after receiving a diagnosis of HIV infection was 95% and remained stable for diagnoses that were made during 2013–2018 (Table 8a).
- Lowest percentages of survival (< 90%) for > 3 years after receiving diagnosis of HIV infection during 2018—persons aged ≥ 55 years and persons with infection attributed to IDU (Tables 8a/b).
In the United States and 6 dependent areas, survival for > 3 years after receiving a stage 3 (AIDS) classification was below 90% and remained stable over time for classifications that were made during 2013–2018 (Table 8d).
- Lowest percentages of survival (< 90%) for > 3 years after receiving a stage 3 (AIDS) classification during 2018—males, females, persons aged ≥ 35 years, each racial/ethnic group (except Asian persons), males and females with infection attributed to any transmission category, and all areas of residence (except Colorado and Minnesota) (Tables 8d–f).
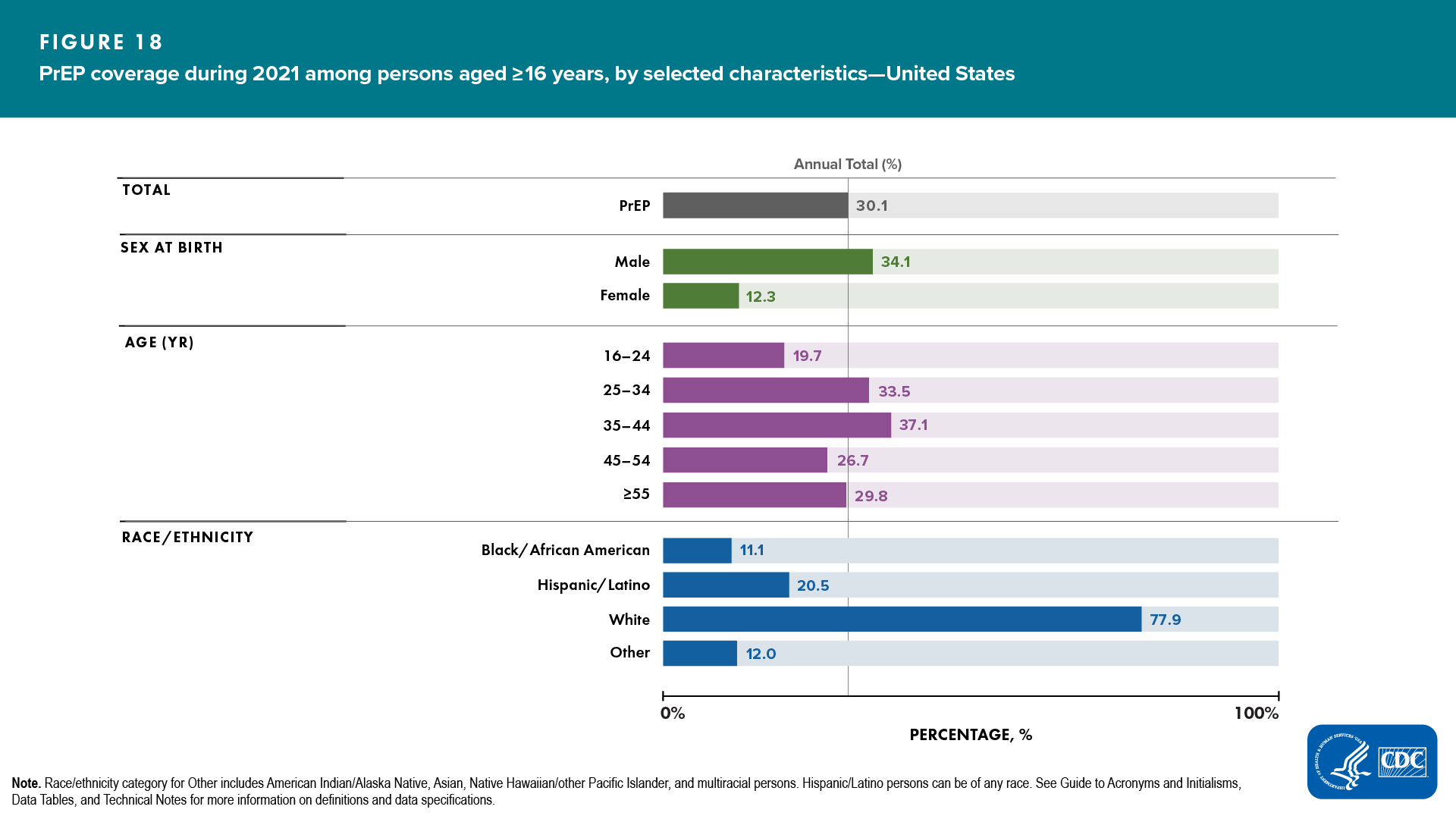
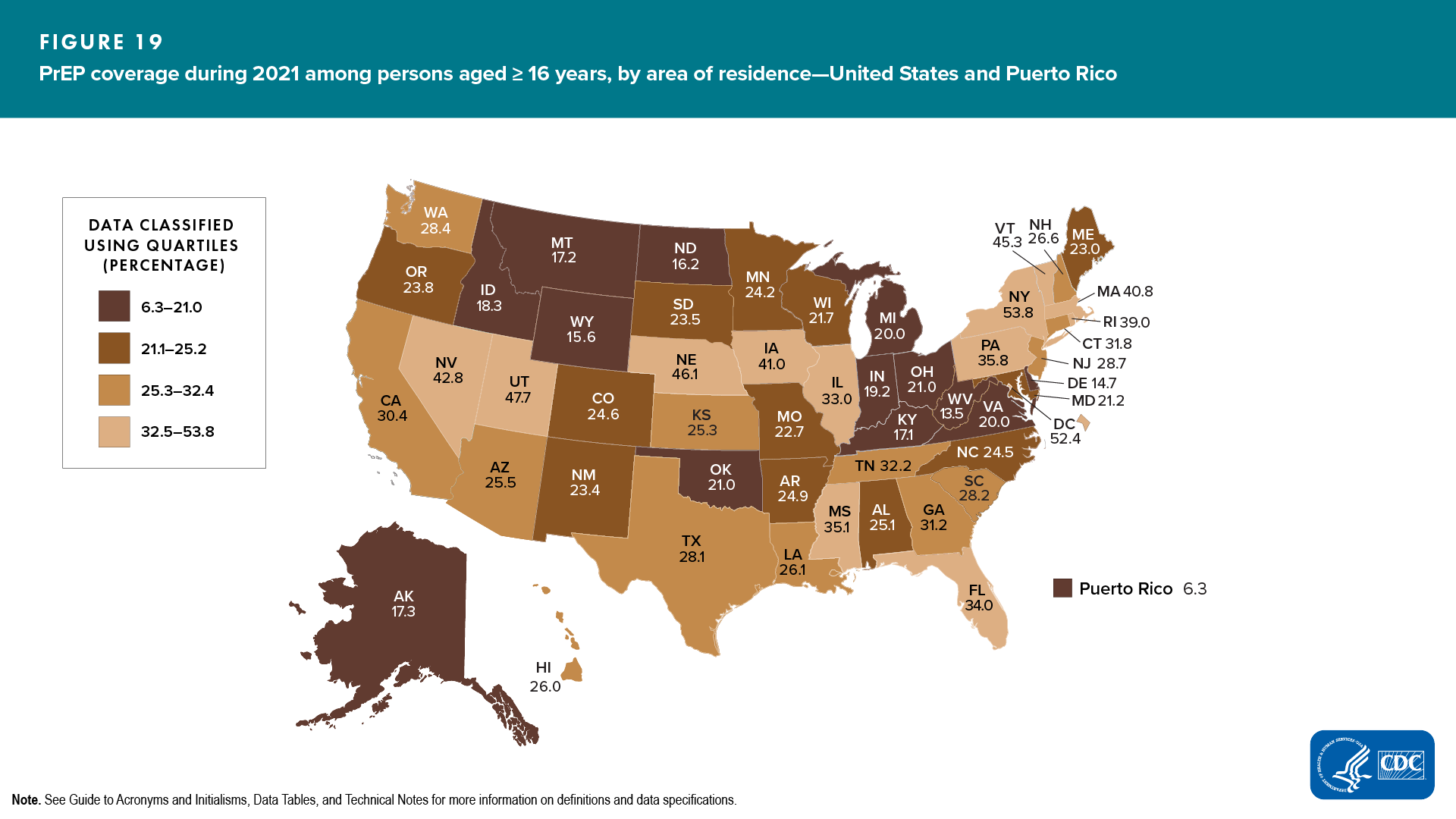
Preexposure Prophylaxis (PrEP) Coverage and Persons Prescribed PrEP
The number of persons in the United States classified as having been prescribed PrEP, the estimated number of persons with PrEP indications, and the percentage of PrEP coverage were produced by using data from several sources: the IQVIA Real-World Longitudinal Prescriptions database, NHSS, National Health and Nutrition Examination Survey (NHANES), and the U.S. Census American Community Survey (ACS). Please note that race/ethnicity data were imputed, and the data source was based on a consumer database, which might underrepresent certain populations. For more information, see Technical Notes.
By using pharmacy and other national data sources, it is estimated 1.2 million persons in the United States had indications for PrEP and 30.1% were prescribed PrEP in 2021 (Table 9a).
Lowest percentages of PrEP coverage by selected characteristics were as follows (Figure 18, Table 9a): ![]()
- ASAB—females (12.3%)
- Age group—aged 16–24 years (19.7%)
- Race/ethnicity—Black/African American (11.1%)
Areas with the lowest percentages of PrEP coverage by area of residence were as follows (Figure 19, Table 9b):
- Quartile ≤ 21.0%―Alaska, Delaware, Idaho, Indiana, Kentucky, Michigan, Montana, North Dakota, Ohio, Oklahoma, Virginia, West Virginia, Wyoming, and Puerto Rico