Social Determinants of Health among Adults with Diagnosed HIV Infection, 2019: National Profile
National SDH Profile
The statements in this section, unless otherwise indicated, are based on stable numbers (i.e., based on 12 or more diagnoses). All rates are per 100,000 population. SDH data are estimates for the period 2015–2019, and HIV surveillance data are based on case information from 2019 diagnoses of HIV infection among adults in the 50 states, the District of Columbia, and Puerto Rico. Data on linkage to HIV medical care and viral suppression within 6 months of HIV diagnosis are based on data from 45 jurisdictions with complete reporting of HIV-related laboratory results (including CD4+ T-lymphocyte [CD4] and viral load results) to CDC (see Technical Notes for list of jurisdictions).
Data presented in this report are a snapshot of the environment in which people lived at the time of HIV diagnosis, and some SDH indicators and selected characteristics may be correlated. For example, lack of education is associated with both poverty and low income in the United States [7, 8]. However, correlations of indicators and characteristics were not assessed for this report.
Important note. The statements in the sections on linkage to care and viral suppression focus on SDH extremes only (e.g., highest poverty, lowest uninsured) and not the overall values within the column unless otherwise indicated. Also, when highlighting care outcomes, the “Other” racial group is not considered when making comparisons across groups.
Please use caution when interpreting data for American Indian/Alaska Native and Native Hawaiian/other Pacific Islander adults due to most rates and/or percentages based on small numbers.
Please read all titles and footnotes carefully to ensure a complete understanding of the displayed data.
See Technical Notes for information on definitions and data specifications.
Diagnoses of HIV Infection—Overview
In the 50 states, the District of Columbia, and Puerto Rico, HIV infection was diagnosed for 29,888 adults (aged 18 years and older) whose residential address information was sufficient for geocoding to the census tract (or tract) level (Table 1). These diagnoses represent approximately 85.4% of all diagnoses of HIV infection in 2019 among adults in these areas. The overall rate of diagnoses of HIV infection was 11.8. The rate was 19.6 for males and 4.4 for females (Table 1).
Linkage to HIV medical care was based on data for adults with infection diagnosed during 2019 in 45 jurisdictions that reported complete CD4 and viral load test results to CDC. Of the 27,376 adults whose infection was diagnosed during 2019 in the 45 jurisdictions, 81.6% (22,345) were linked to HIV medical care ≤ 1 month after diagnosis (Table 9).
Viral suppression within 6 months of HIV diagnosis was measured for adults whose infection was diagnosed during 2019 and who resided in the 45 jurisdictions at time of diagnosis. Of the 27,376 adults whose infection was diagnosed during 2019 in the 45 jurisdictions, 69.9% (19,124 adults) had a suppressed viral load within 6 months (Table 9).

Federal Poverty Status
Poverty is not a single factor but rather is characterized by multiple physical and psychosocial stressors [9]. Poverty places individuals from lower income households at increased risk for HIV due to economic disadvantages that may lead to increased risk behaviors [10]. Poverty and wealth can be viewed in relation to one another as follows: poverty is defined as lacking a usual or socially acceptable amount of money or material possessions; whereas, wealth is defined as having an abundance of valuable material possessions or resources [11, 12].
In 2019, adults who lived in census tracts with the highest level of poverty (i.e., lowest level of wealth; where 18% or more of the residents lived below the federal poverty level) accounted for
- the highest HIV diagnosis rates or percentages (diagnoses),
- the lowest percentages of adults linked to HIV medical care ≤ 1 month after receiving a diagnosis (linkage), and
- the lowest percentages of adults with suppressed viral load within 6 months of receiving an HIV diagnosis (viral suppression) among groups by selected characteristics:
Sex at birth:
- Diagnoses—rates: males, 34.4; females, 9.2 (Table 1).
- Linkage—males, 80.7%; females, 79.8% (Table 9).
- Viral suppression—males, 67.4%; females, 67.6% (Table 9).
Age group:
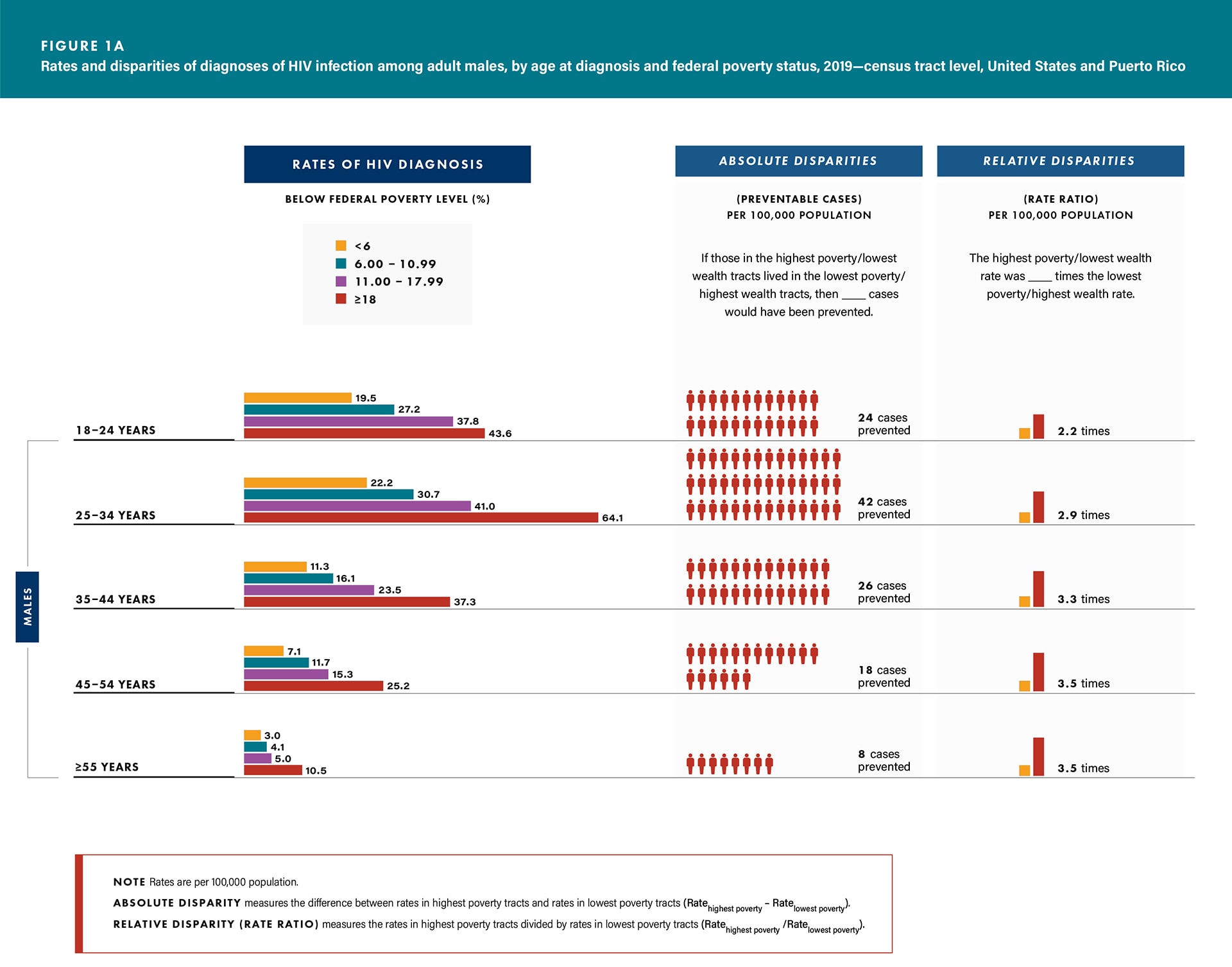
- Diagnoses—all age groups for both sexes (Figures 1a/b and Table 1).
- Linkage—all age groups for both sexes (except males aged 35–44 and ≥ 55 years and females aged 25–34 and ≥ 55 years) (Table 9).
- Viral suppression—all age groups for both sexes (except females ≥ 55 years) (Table 9).
Race/ethnicity:
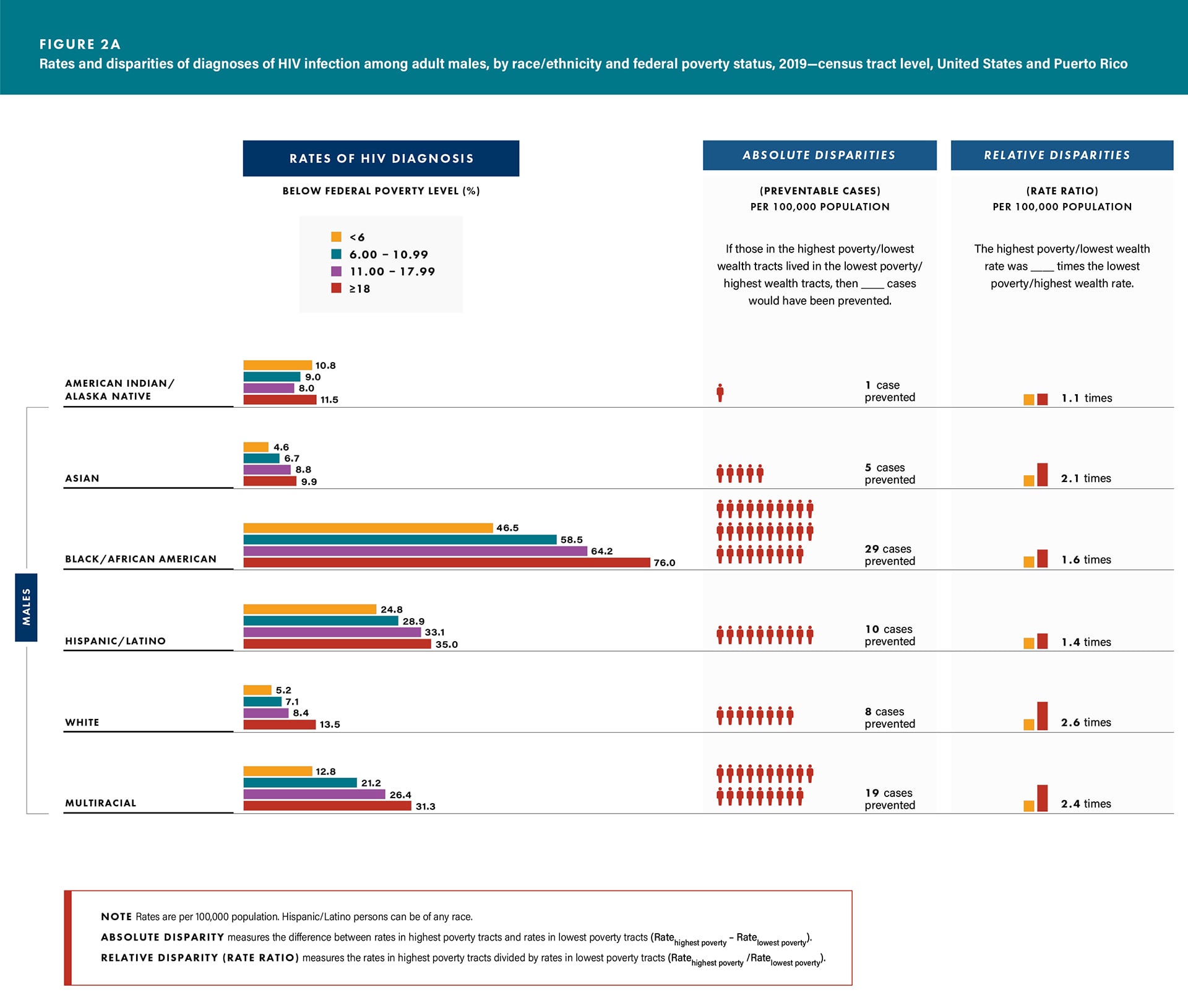
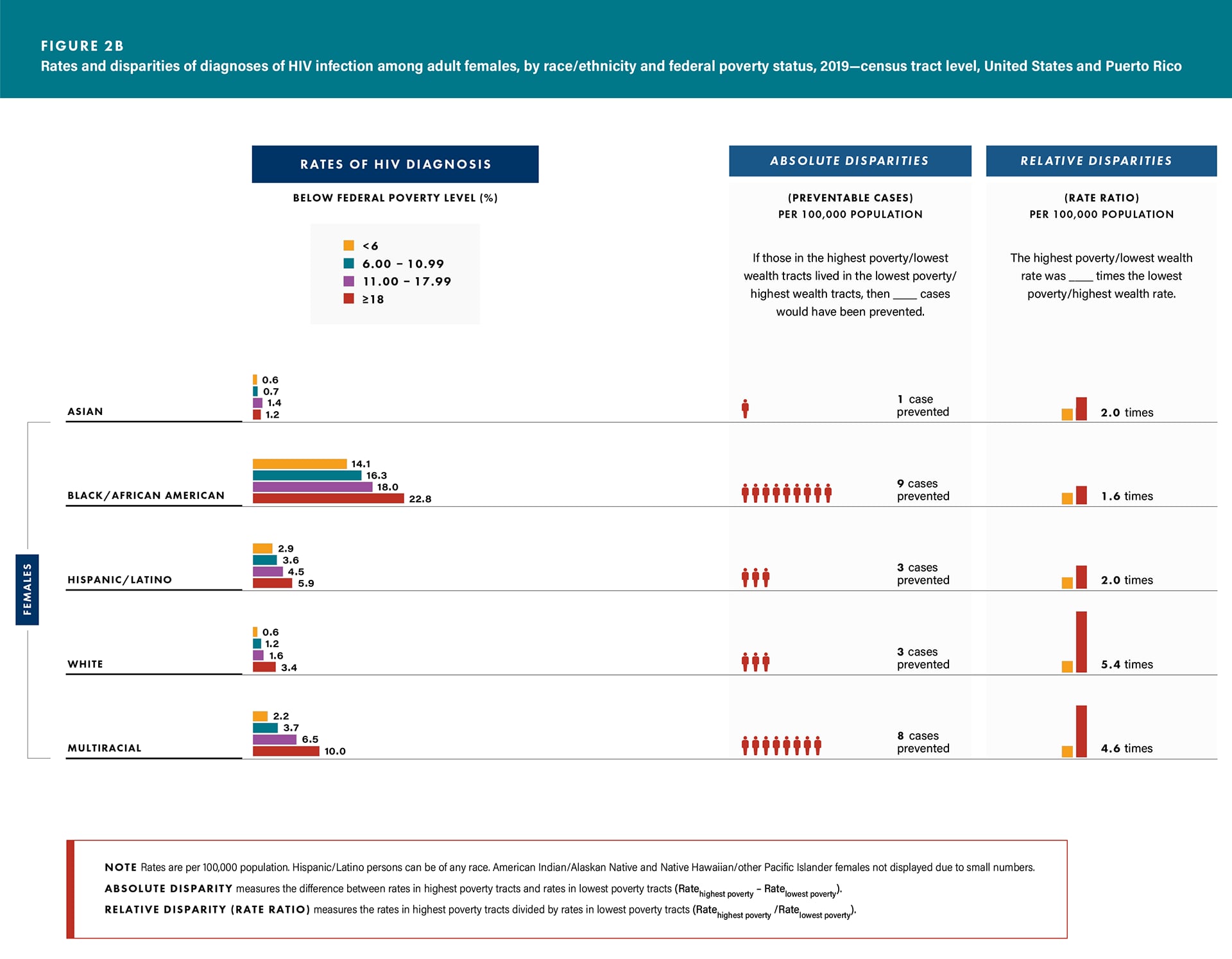
- Diagnoses—all racial/ethnic groups among both sexes (except Asian females) (Figures 2a/b and Table 2).
- Linkage—Black/African American males (77.5%) and females (79.1%), Hispanic/Latino males (84.9%) and females (82.7%), and White females (78.6%) (Table 10).
- Viral Suppression—Black/African American males (63.8%) and females (67.8%), Hispanic/Latino males (71.1%), and White females (59.8%) (Table 10).
Transmission category:
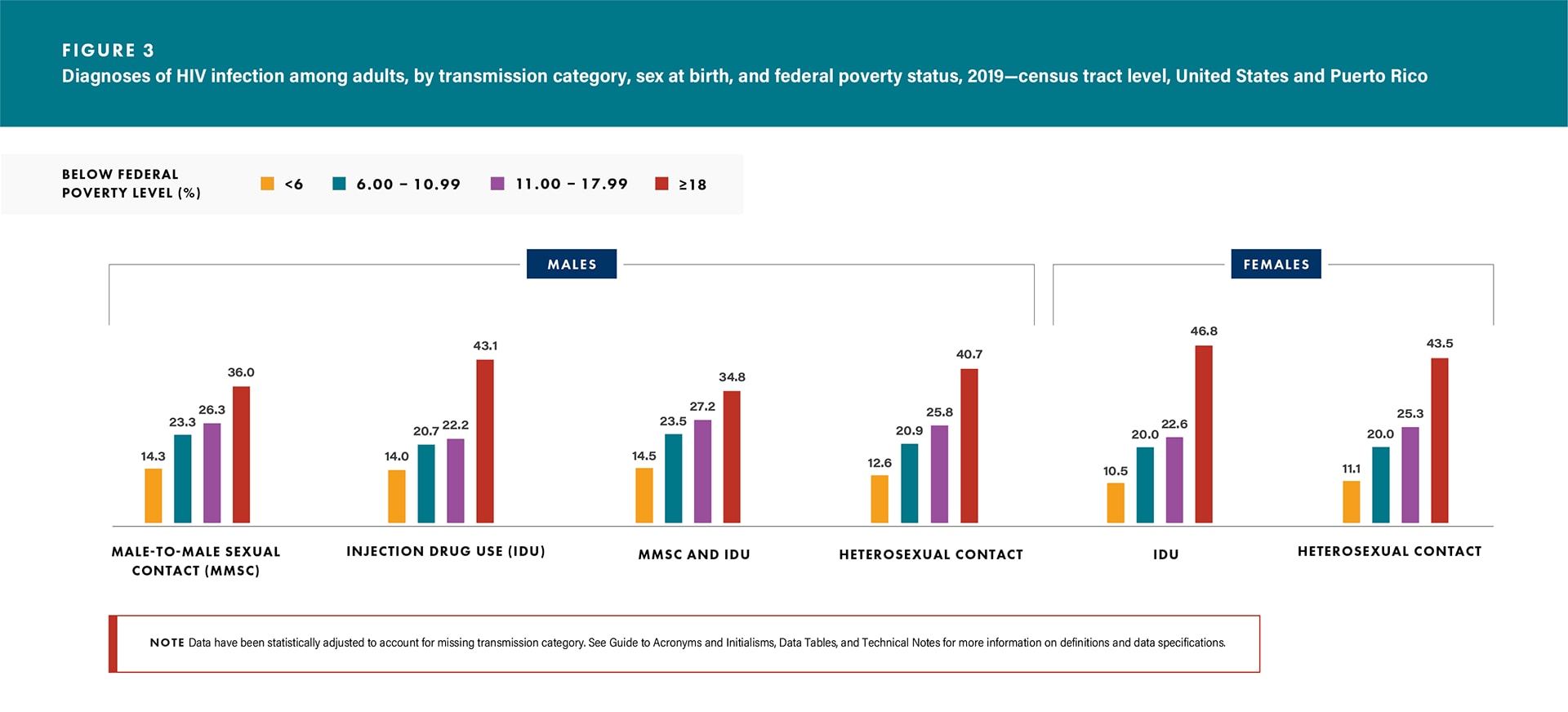
- Diagnoses—all transmission categories for both sexes (Figure 3 and Table 3).
- Linkage—all transmission categories for both sexes (except males with infection attributed to injection drug use [IDU] and to male-to-male sexual contact and injection drug use [MMSC and IDU] and females with infection attributed to IDU) (Table 11).
- Viral suppression—all transmission categories for both sexes (except males with infection attributed to MMSC and IDU) (Table 11).
- Among males with infection attributed to MMSC:
- Linkage—Black/African American (77.9%), and
- Viral suppression—Black/African American (64.6%) and Hispanic/Latino (72.2%) (Table 12).
Area of residence: Diagnoses—rates: District of Columbia (total, 60.9; males, 93.2; females, 34.1), followed by Florida (total, 45.7; males, 70.2) and Maryland for females (24.4) (Table 4). Use caution when comparing the rates of diagnoses for the District of Columbia to the rates for states.
A Look at Disparities in Diagnoses of HIV Infection by Poverty
In 2019, the disparities of HIV diagnosis by poverty for adults were as follows:
- Absolute disparities (rate difference): If males or females in the highest poverty/lowest wealth tracts lived in the lowest poverty/highest wealth tracts, then 25 cases and 7 cases per 100,000 population, respectively, would have been prevented (Table 1).
- Relative disparities (rate ratio): Among males, the rate of diagnoses in the highest poverty/lowest wealth tracts was 3.5 times the rate in the lowest poverty/highest wealth tracts, and among females, the rate in the highest poverty/lowest wealth tracts was 5.3 times the rate in the lowest poverty/highest wealth tracts (Table 1).
For absolute and relative disparities for sex at birth stratified by age group and race/ethnicity, see Figures 1a/b and 2a/b. See Technical Notes for additional information on disparity measures.
Education Level

Education plays an important role in preventing HIV; increased education reduces the social and economic circumstances that may put someone at increased risk for HIV [13]. Persons with higher levels of education typically have better health outcomes due to higher levels of income and occupational status (i.e., social position) [14].
In 2019, adults who lived in census tracts with the lowest level of education (where 17% or more of the residents had less than a high school diploma) accounted for
- the highest HIV diagnosis rates or percentages (diagnoses),
- the lowest percentages of adults linked to HIV medical care ≤ 1 month after receiving a diagnosis (linkage), and
- the lowest percentages of adults with suppressed viral load within 6 months of receiving an HIV diagnosis (viral suppression) among:
Sex at birth:
- Diagnoses—rates: males, 29.5; females, 8.3 (Table 1).
- Linkage—males, 80.8%; females, 79.5% (Table 9).
- Viral suppression—males, 67.8%; females, 67.5% (Table 9).
Age group:
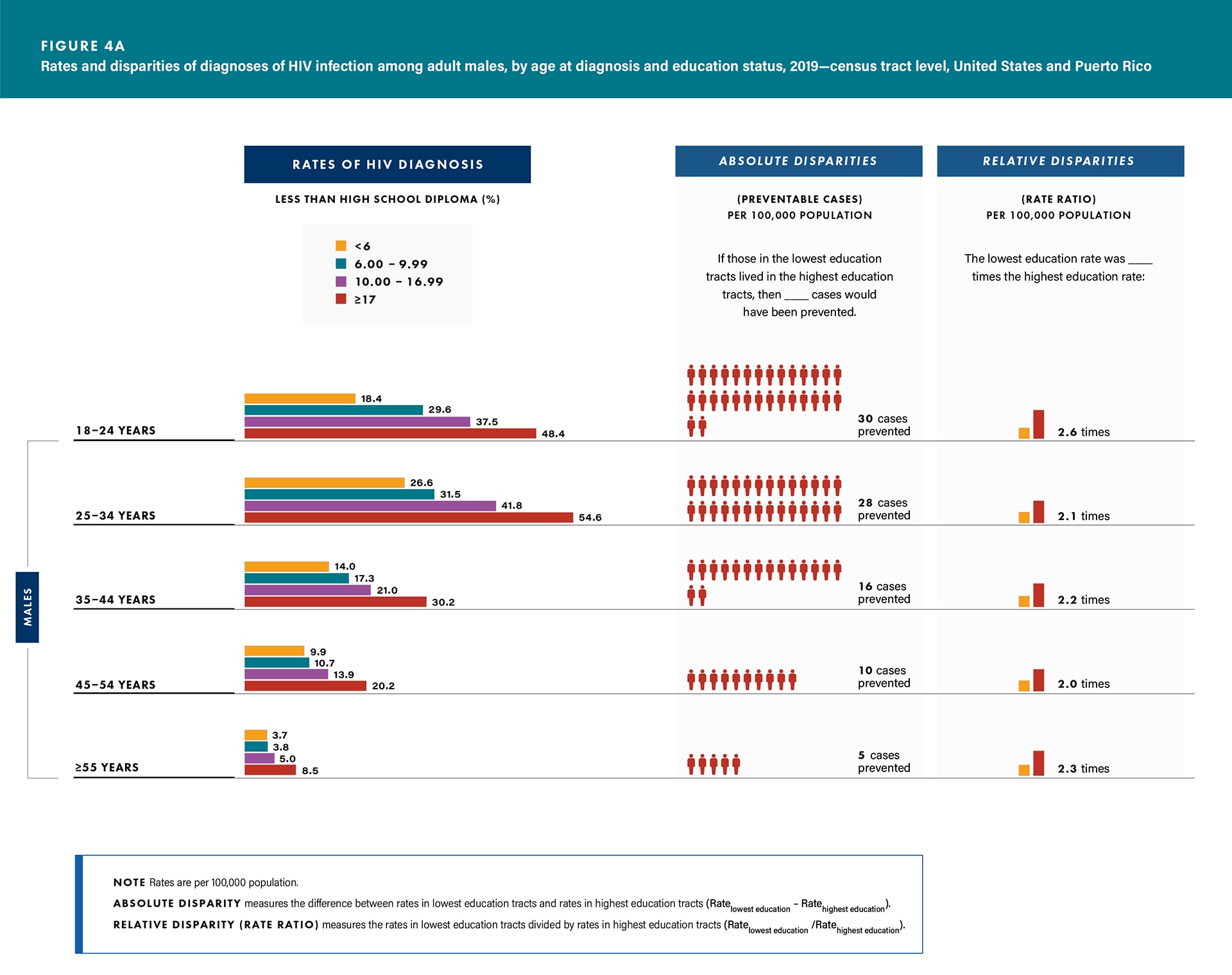
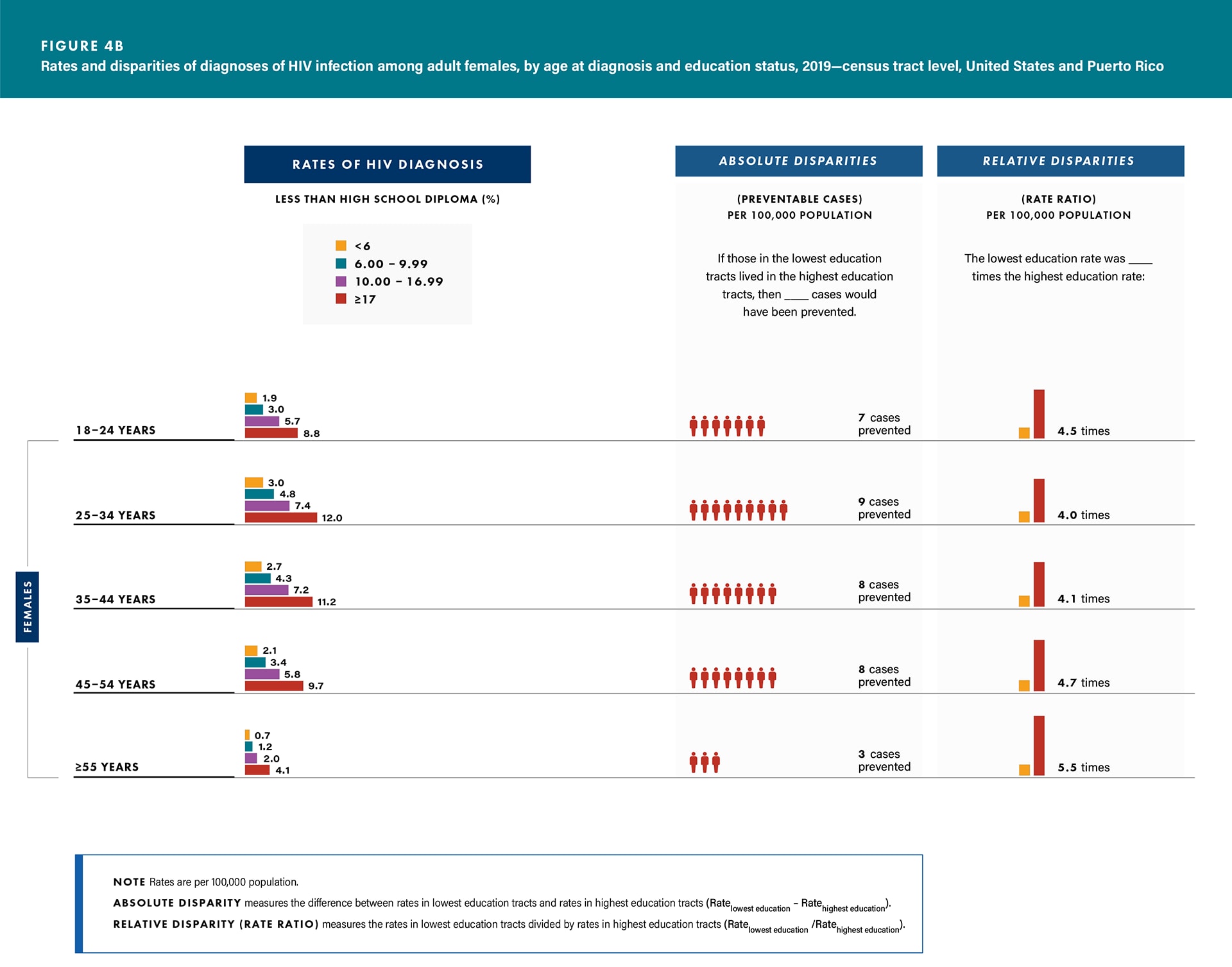
- Diagnoses—all age groups for both sexes (Figures 4a/b and Table 1).
- Linkage—all age groups for both sexes (except males aged 35–44 and 45–54 years) (Table 9).
- Viral suppression—all age groups for both sexes (Table 9).
Race/ethnicity:
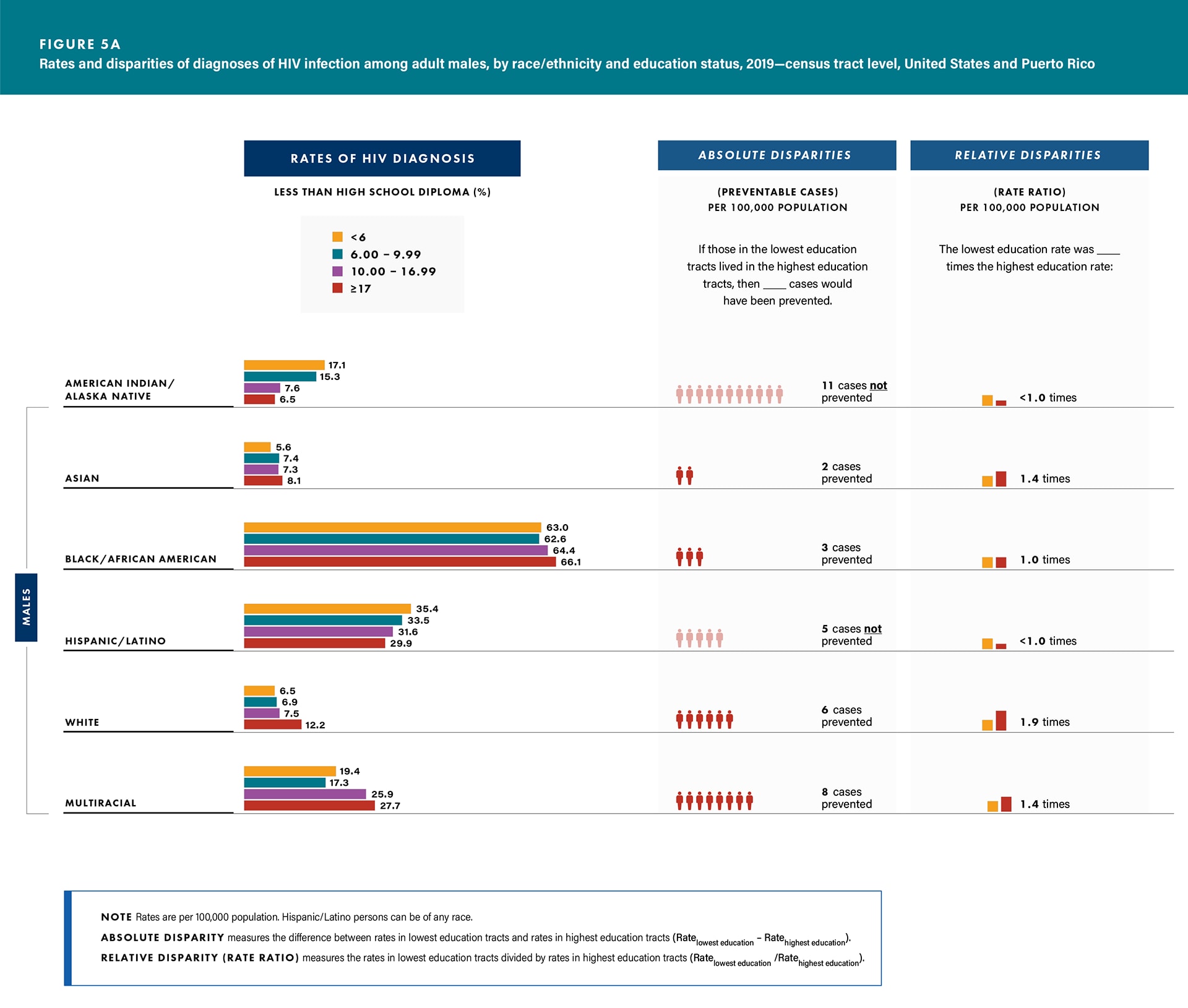
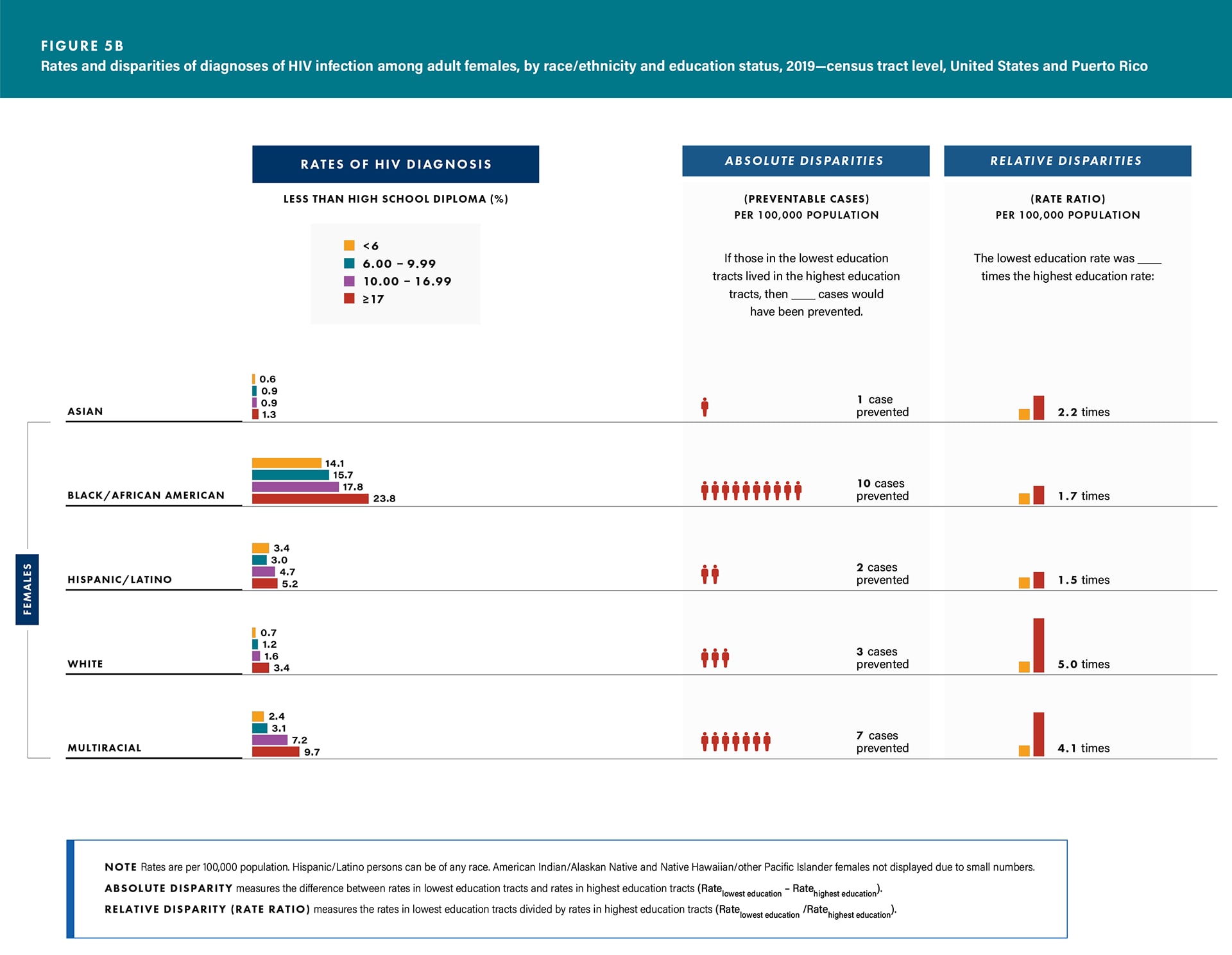
- Diagnoses—all racial/ethnic groups for both sexes (except American Indian/Alaska Native and Hispanic/Latino males) (Figures 5a/b and Table 2).
- Linkage—all racial/ethnic groups for both sexes (except American Indian/Alaska Native males, Hispanic/Latino males, and Asian females) (Table 10).
- Viral suppression—Black/African American males (64.1%) and females (67.2%), Hispanic/Latino males (71.4%), White males (68.6%), and multiracial males (66.7%) and females (69.6%) (Table 10).
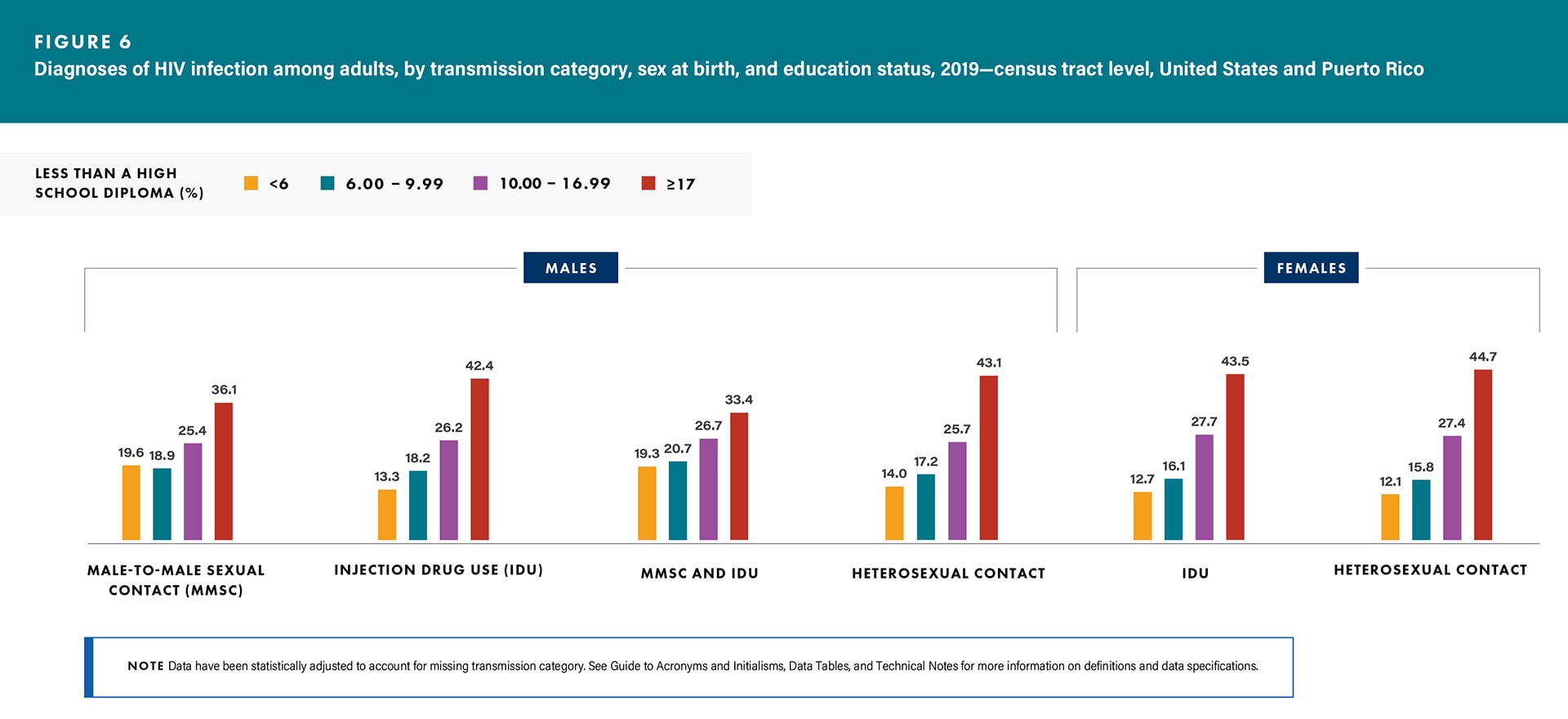
Transmission category:
- Diagnoses—all transmission categories for both sexes (Figure 6 and Table 3).
- Linkage—all transmission categories for both sexes (except males with infection attributed to IDU) (Table 11).
- Viral suppression—all transmission categories for both sexes (except males with infection attributed to IDU and to MMSC and IDU) (Table 11).
- Among males with infection attributed to MMSC,
- Linkage—Asian (85.3%), Black/African American (77.6%), and White (82.1%), and
- Viral suppression—Black/African American (64.8%), Hispanic/Latino (72.5%), and White (70.1%) (Table 12).
Area of residence: Diagnoses—rates: District of Columbia (total, 88.9; males, 125.4; females, 55.7), followed by Florida (total, 42.1; males, 63.2) and Maryland for females (32.0) (Table 5). Use caution when comparing the rates of diagnoses for the District of Columbia to the rates for states.
A Look at Disparities in Diagnoses of HIV Infection by Education
In 2019, the disparities of HIV diagnosis by education for adults were as follows:
Absolute disparities (rate difference): If males or females in the lowest education tracts lived in the highest education tracts, then 17 cases and 7 cases per 100,000 population, respectively, would have been prevented.
Relative disparities (rate ratio): Among males, the rate of diagnoses in the lowest education tracts was 2.4 times the rate in the highest education tracts, and among females, the rate in the lowest education tracts was 4.6 times the rate in the highest education tracts (Table 1).
For absolute and relative disparities for sex at birth stratified by age group and race/ethnicity, see Figures 4a/b and 5a/b.
See Technical Notes for additional information on disparity measures.
Median Household Income

HIV has a direct and indirect cost on household income. Lower income households, when compared to higher income households, may require a greater proportion of expenditures for essential household items. HIV, like other chronic diseases, leads to economic hardship when resources (particularly, limited resources) are shifted from household necessities to costs incurred related to HIV morbidity and mortality [15]. Additionally, decreased median household income is related to a lower probability of survival after an HIV diagnosis [16].
In 2019, adults who lived in census tracts with the lowest median household income (where the median household income was less than $44,000 a year) accounted for
- the highest HIV diagnosis rates or percentages (diagnoses),
- the lowest percentages of adults linked to HIV medical care ≤ 1 month after receiving a diagnosis (linkage), and
- the lowest percentages of adults with suppressed viral load within 6 months of receiving an HIV diagnosis (viral suppression) among:
Sex at birth:
- Diagnoses—rates: males, 34.4; females, 9.2 (Table 1).
- Linkage—males, 80.2%; females, 79.6% (Table 9).
- Viral suppression—males, 66.8%; females, 67.0% (Table 9).
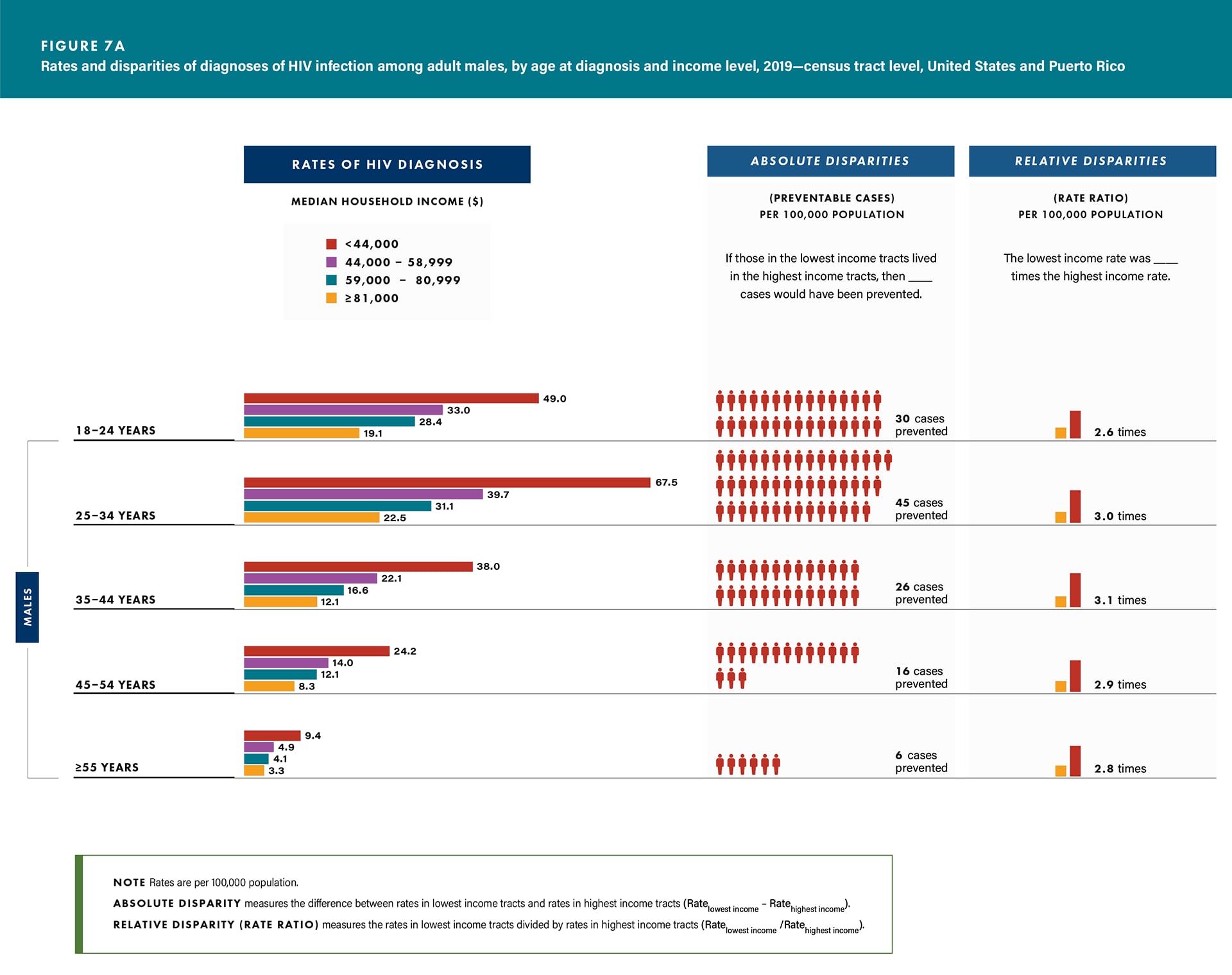
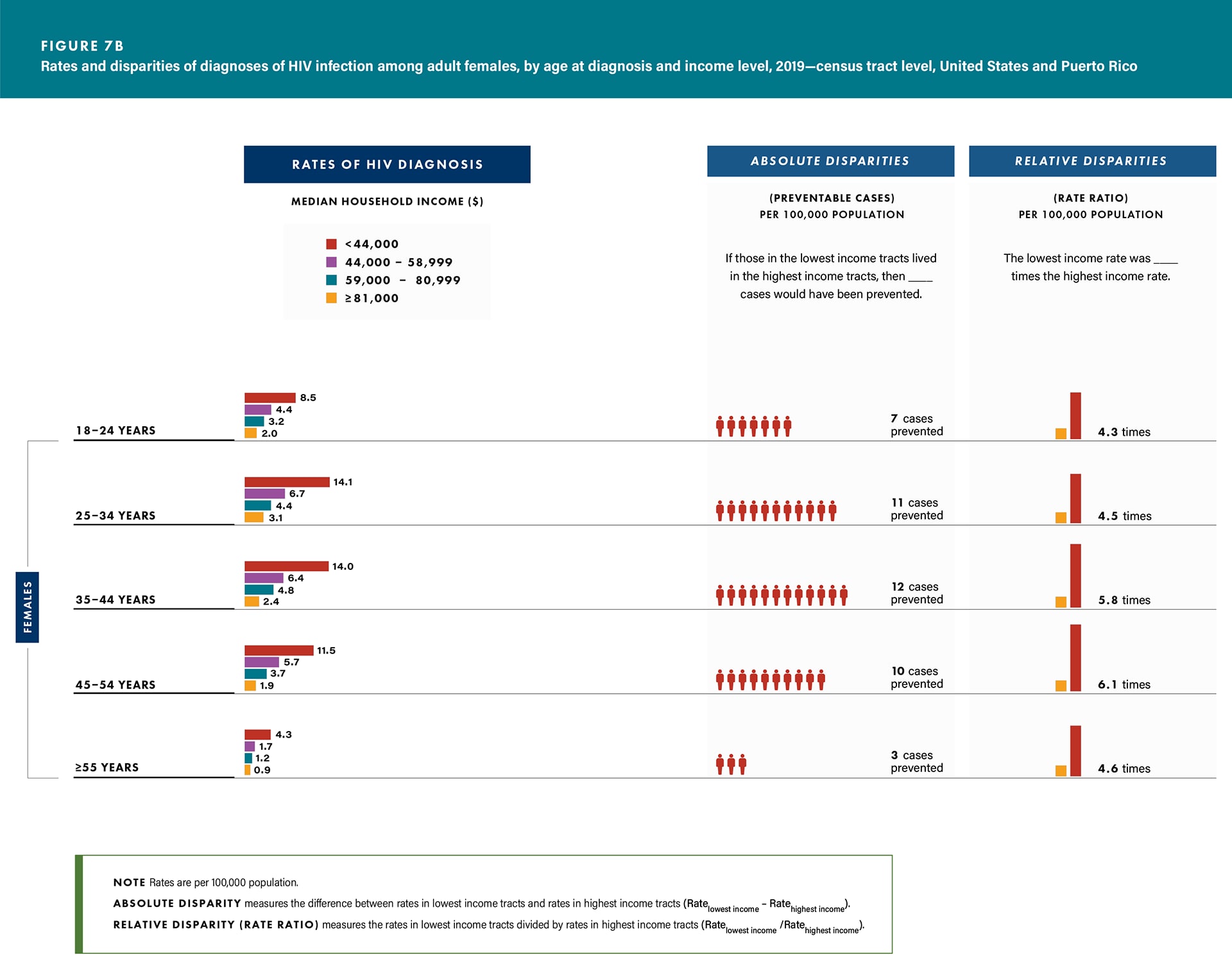
Age group:
- Diagnoses—all age groups for both sexes (Figures 7a/b and Table 1).
- Linkage—all age groups for both sexes (except males aged 18–24 years, males and females aged ≥ 55 years, and females aged 25–34 and 45–54 years) (Table 9).
- Viral suppression—all age groups for both sexes (except females aged 45–54 and ≥ 55 years) (Table 9).
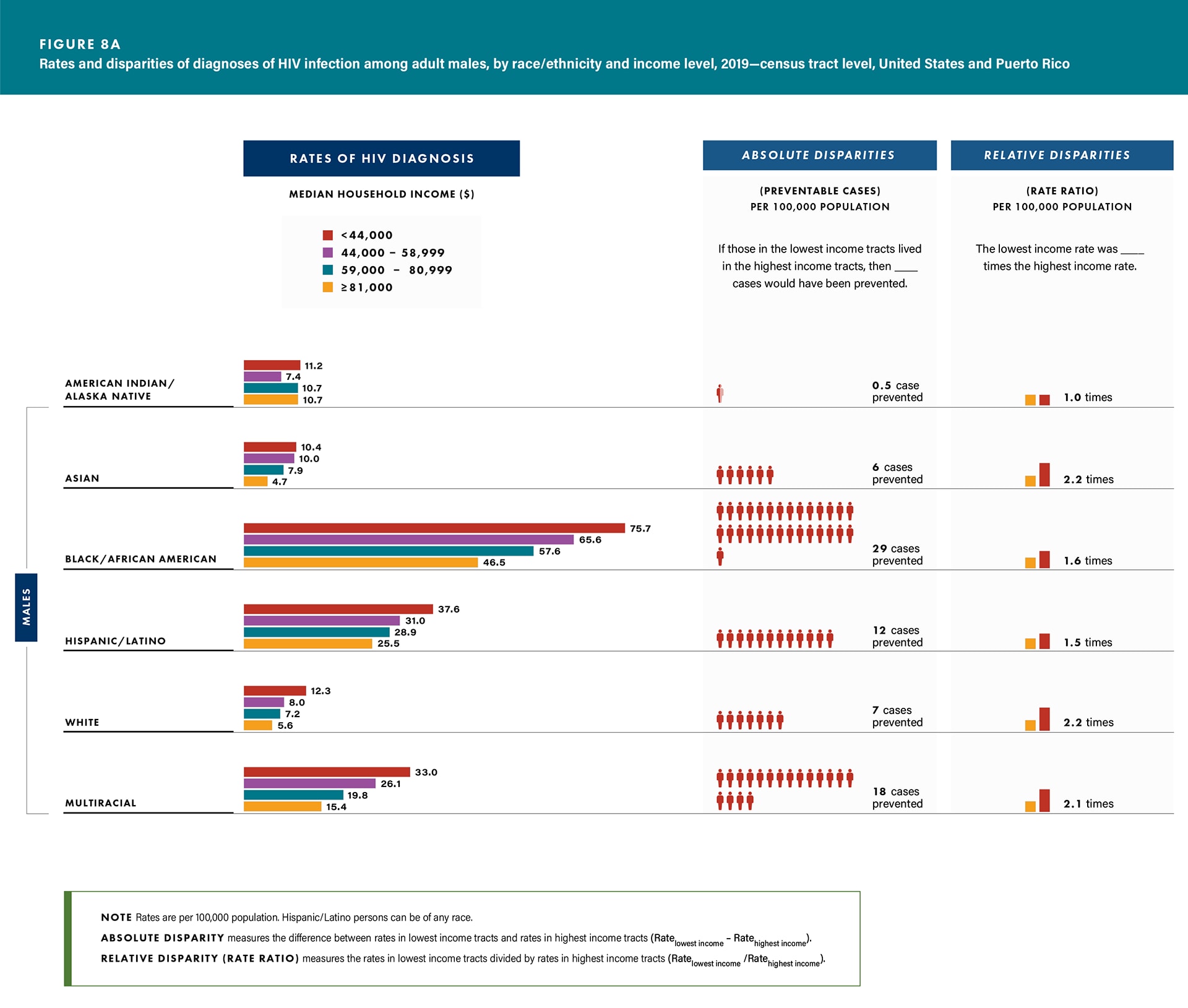
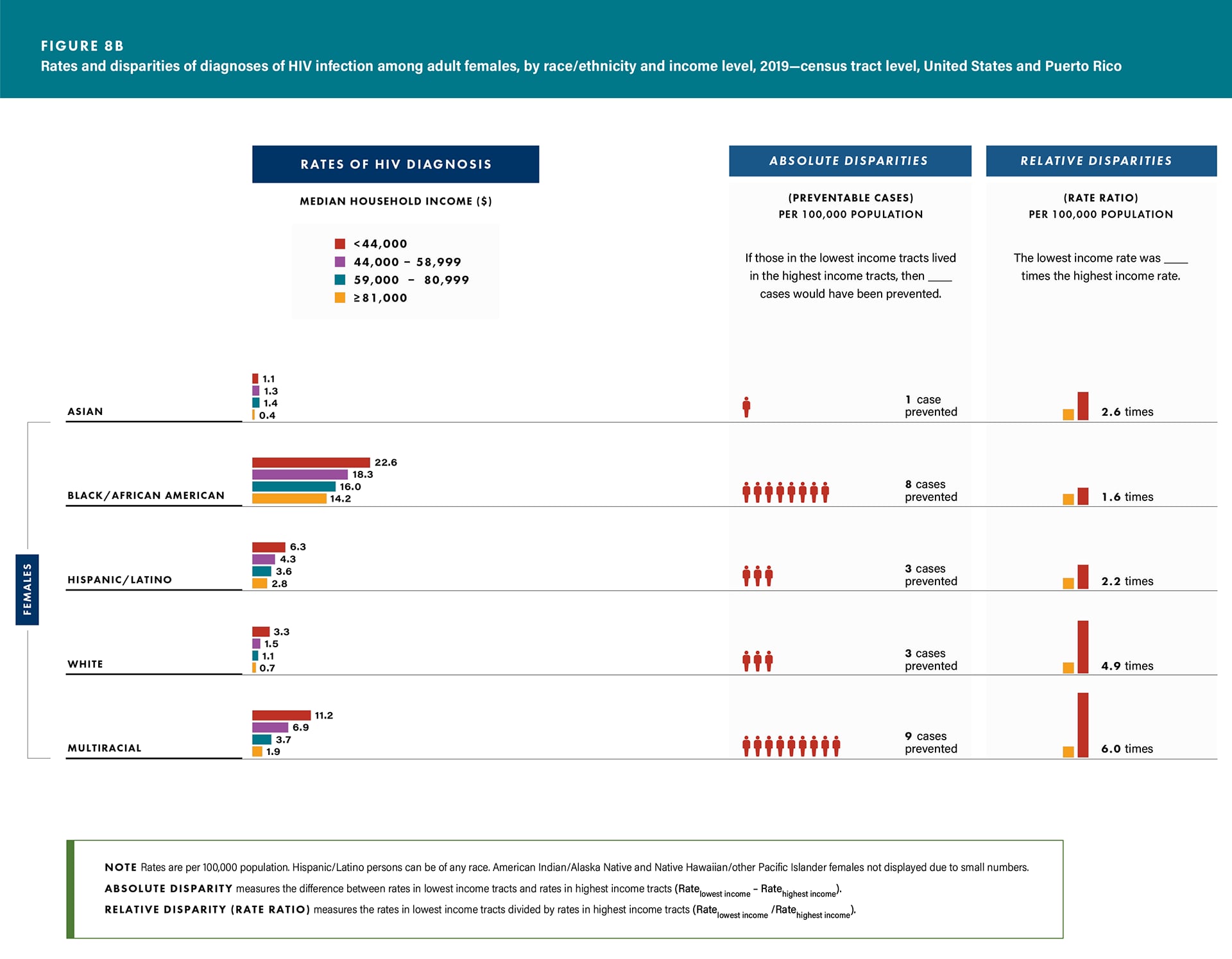
Race/ethnicity:
- Diagnoses—all racial/ethnic groups for both sexes (except Asian females) (Figures 8a/b and Table 2).
- Linkage—Black/African American males (76.8%) and females (79.4%) and White females (77.1%) (Table 10).
- Viral suppression—all racial/ethnic groups for both sexes (except multiracial males and Asian and Hispanic/Latino females) (Table 10).
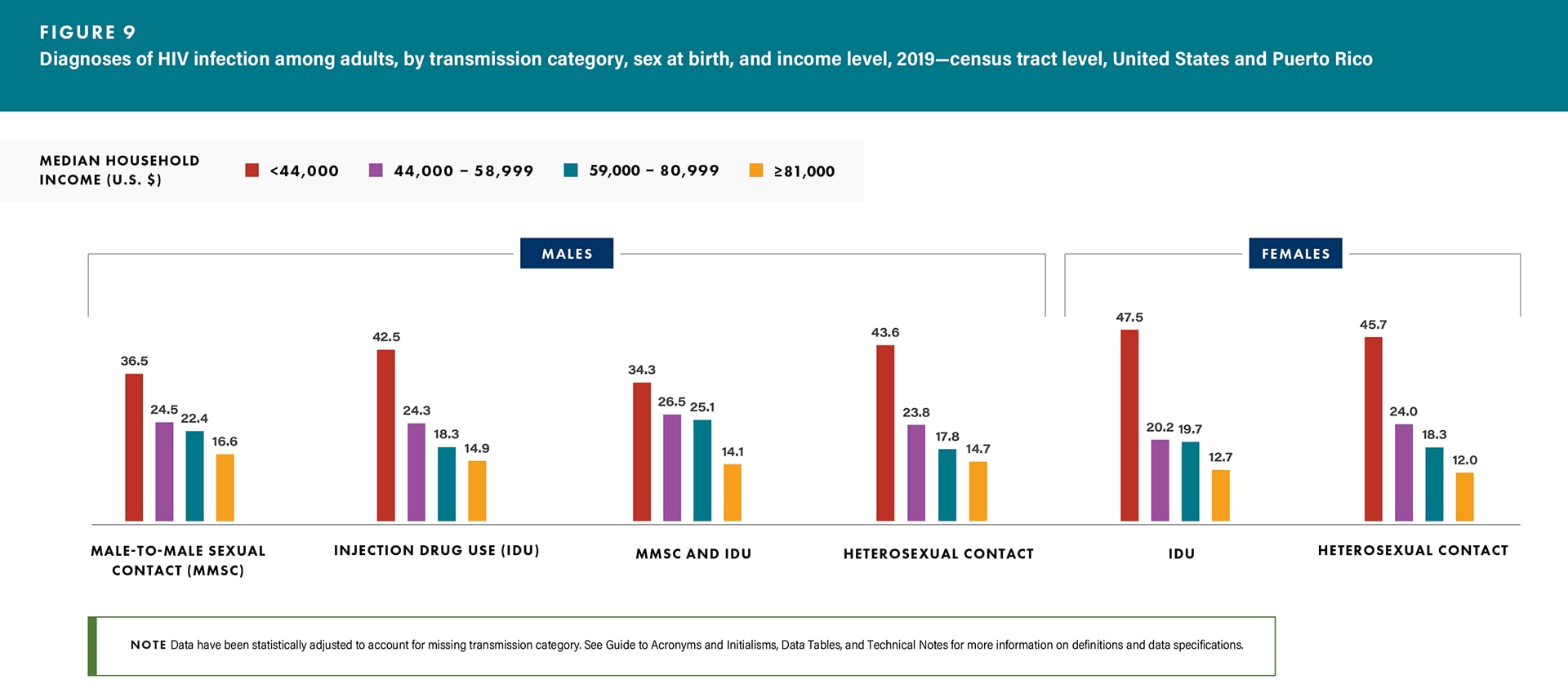
Transmission category:
- Diagnoses—all transmission categories for both sexes (Figure 9 and Table 3).
- Linkage—all transmission categories for both sexes (except males with infection attributed to IDU) (Table 11).
- Viral suppression—all transmission categories for both sexes (except males with infection attributed to IDU) (Table 11).
- Among males with infection attributed to MMSC,
- Linkage—Black/African American (77.5%), and
- Viral suppression—Asian (77.8%), Black/African American (64.5%), Hispanic/Latino (71.7%), and White (72.8%) (Table 12).
A look at Disparities in Diagnoses of HIV Infection by Income
In 2019, the disparities of HIV diagnosis by income for adults were as follows:
Absolute disparities (rate difference): If males or females in the lowest income tracts lived in the highest income tracts, then 24 cases and 7 cases per 100,000 population, respectively, would have been prevented (Table 1).
Relative disparities (rate ratio): Among males, the rate of diagnoses in the lowest income tracts was 3.2 times the rate in the highest income tracts, and among females, the rate in the lowest income tracts was 5.1 times the rate in the highest income tracts (Table 1).
For absolute and relative disparities for sex at birth stratified by age group and race/ethnicity, see Figures 7a/b and 8a/b.
See Technical Notes for additional information on disparity measures.
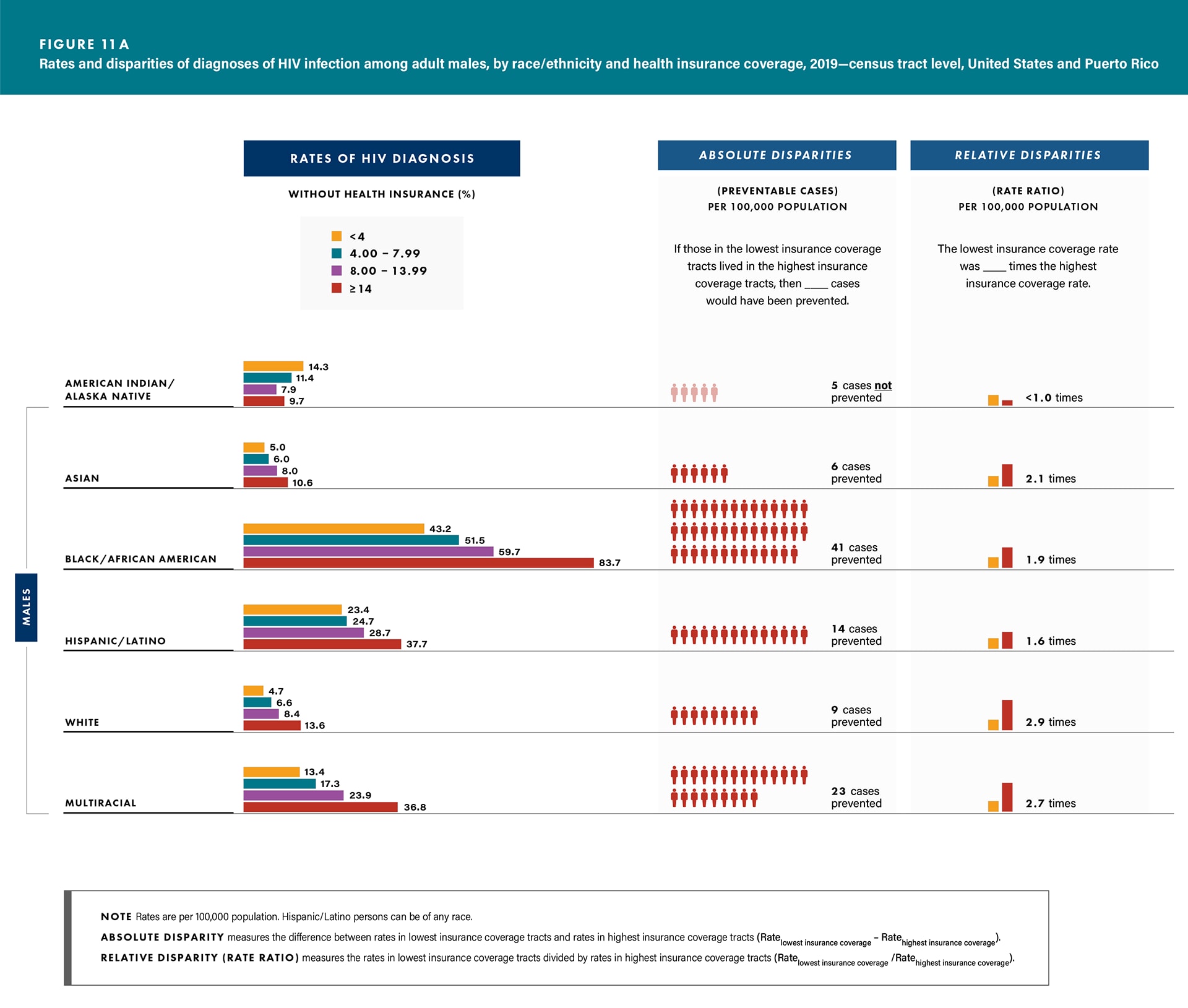
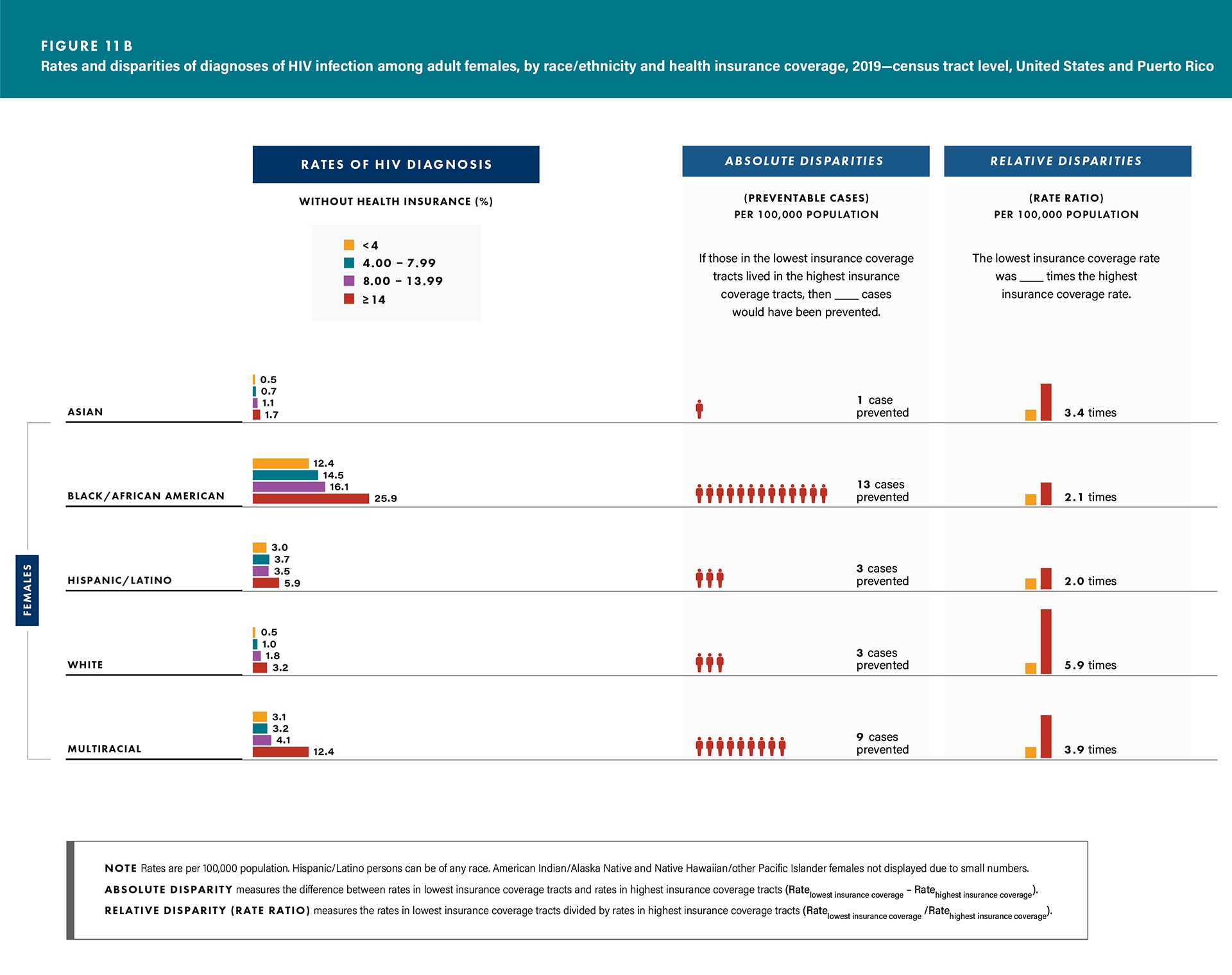
Health Insurance Coverage

Health insurance coverage is associated with the use of preventive services and better medical outcomes [17]. Additionally, insured persons with diagnosed HIV are more likely to receive HIV care and treatment, which prolongs life, increases viral suppression, and decreases mortality [18]. Limited access to health insurance and care can increase the risk for HIV and affect health and well-being.
In 2019, adults who lived in census tracts with the lowest health insurance or health coverage plan (hereafter referred to as health insurance coverage) (where 14% or more of the residents did not have health insurance coverage) accounted for
- the highest HIV diagnosis rates or percentages (diagnoses),
- the lowest percentages of adults linked to HIV medical care ≤ 1 month after receiving a diagnosis (linkage), and
- the lowest percentages of adults with suppressed viral load within 6 months of receiving an HIV diagnosis (viral suppression) among:
Sex at birth:
- Diagnoses—rates: males, 35.2; females, 8.9 (Table 1).
- Linkage—males, 79.8%; females, 79.6% (Table 9).
- Viral suppression—males, 67.5; females, 67.6% (Table 9).
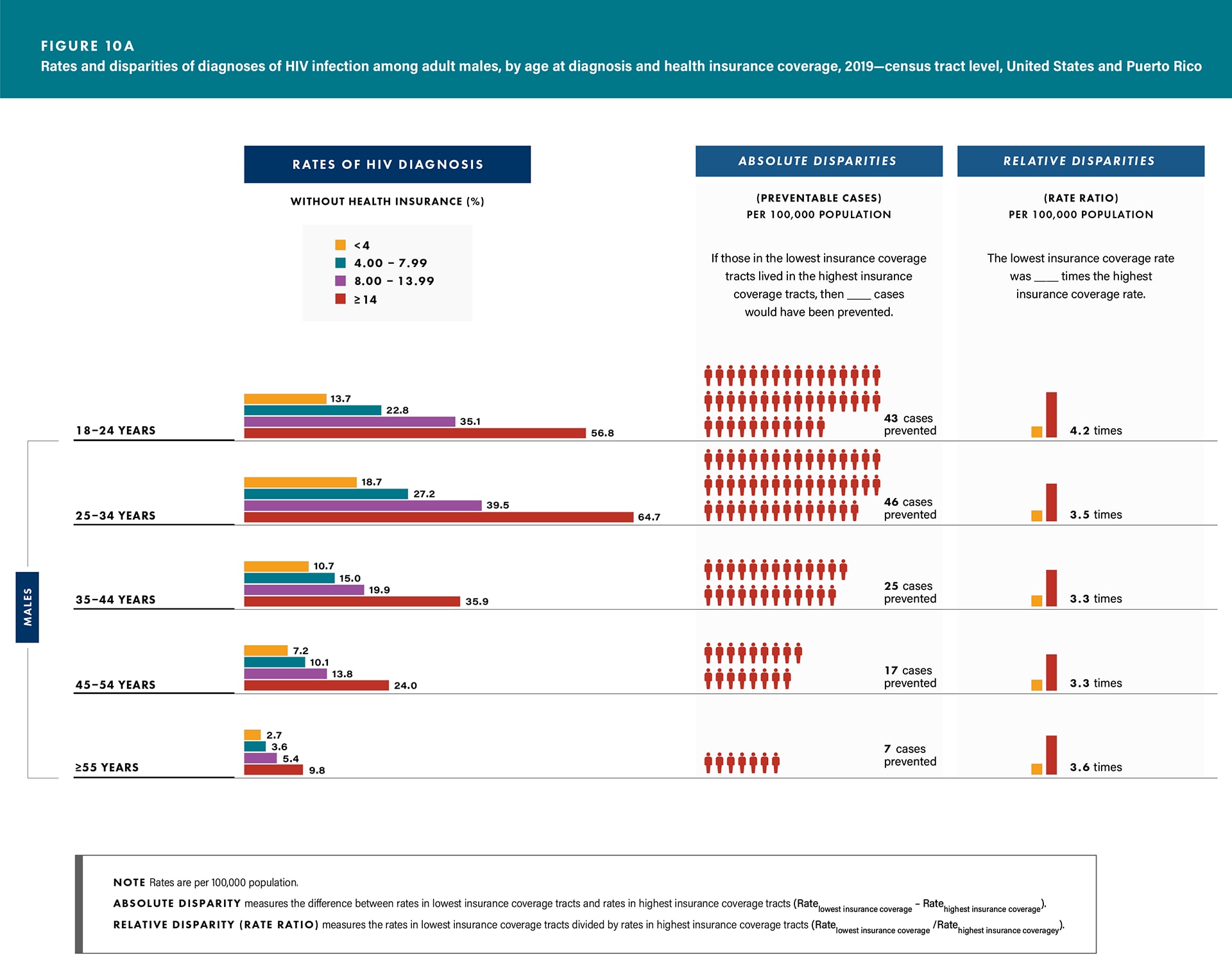
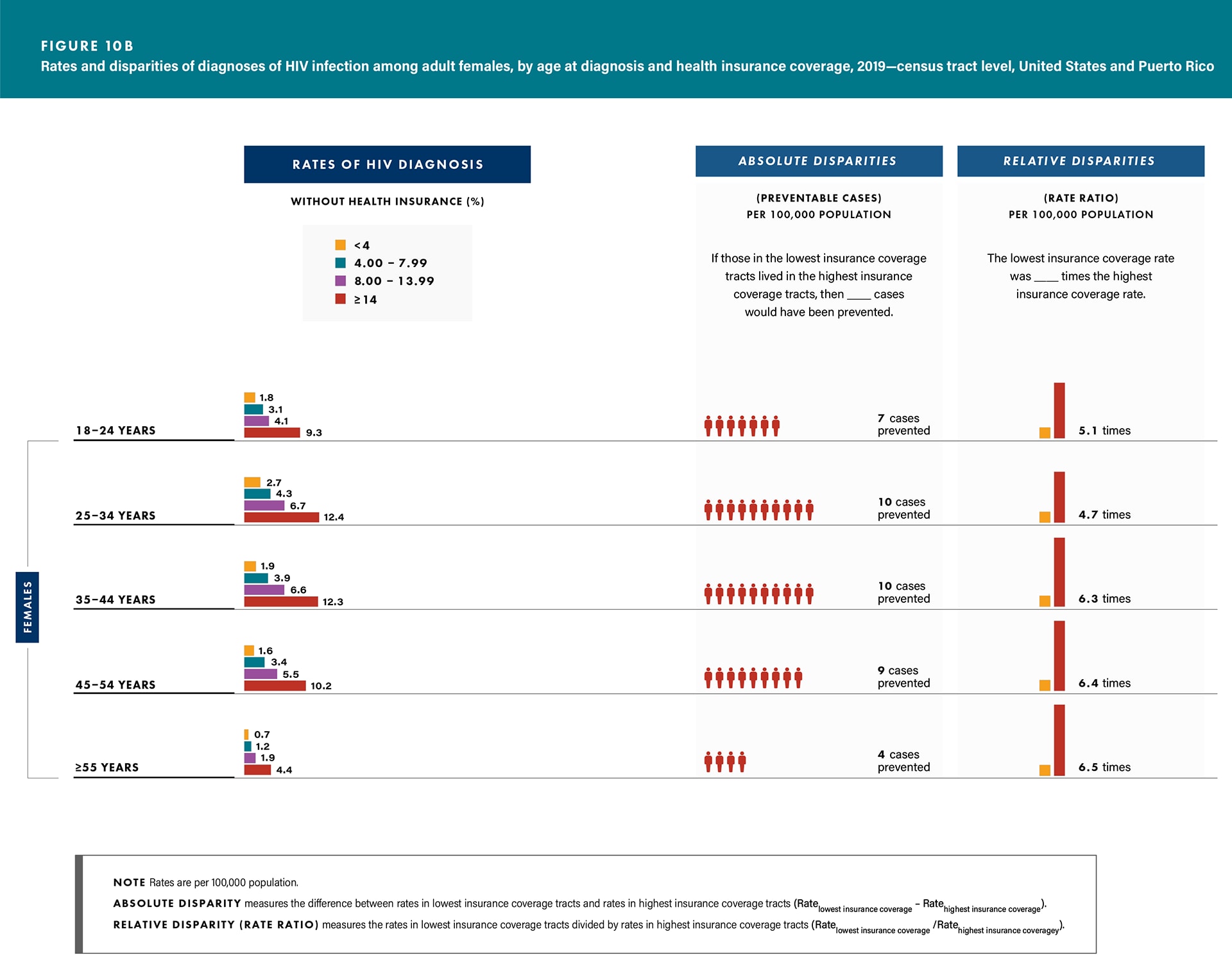
Age group:
- Diagnoses—all age groups for both sexes (Figures 10a/b and Table 1).
- Linkage—all age groups for both sexes (except females aged 25–34 years) (Table 9).
- Viral suppression—all age groups for both sexes (Table 9).
Race/ethnicity:
- Diagnoses—all racial/ethnic groups for both sexes (except American Indian/Alaska Native males) (Figures 11a/b and Table 2).
- Linkage—all racial/ethnic groups for both sexes (except American Indian/Alaska Native males and Asian females) (Table 10).
- Viral suppression—all racial/ethnic groups for both sexes (except American Indian/Alaska Native males, Asian females, and multiracial males and females) (Table 10).
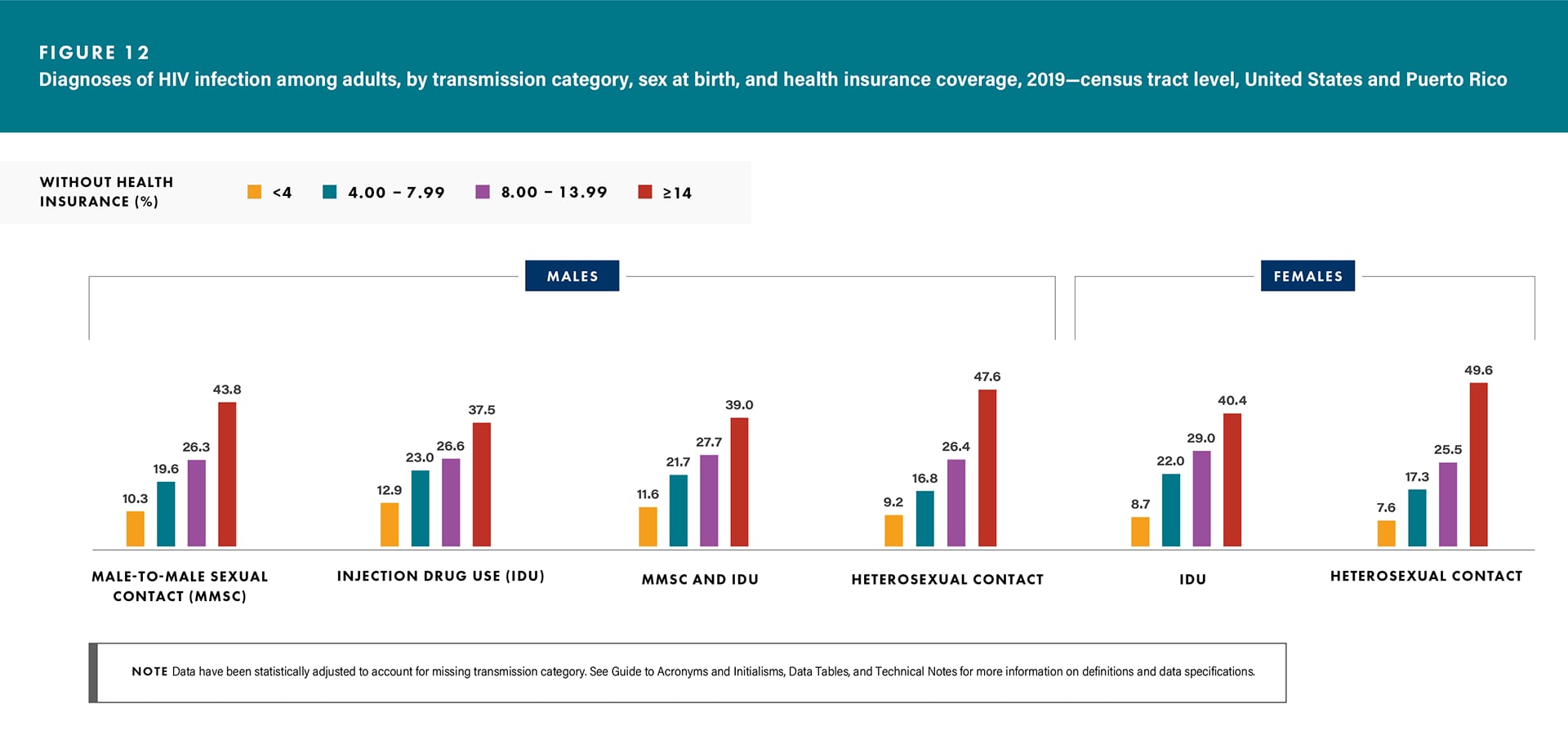
Transmission category:
- Diagnoses—all transmission categories for both sexes (Figure 12 and Table 3).
- Linkage—all transmission categories for both sexes (except males with infection attributed to MMSC and IDU) (Table 11).
- Viral suppression—all transmission categories for both sexes (except males with infection attributed to MMSC and IDU) (Table 11).
- Among males with infection attributed to MMSC:
- Linkage—Asian (82.3%), Black/African American (76.5%), Hispanic/Latino (84.5%) White (81.4%), and multiracial (76.4%), and
- Viral suppression—Asian (76.4%), Black/African American (64.7%), Hispanic/Latino (72.8%), and White (69.6%) (Table 12).
Area of residence: Diagnoses—rates: Maryland (total, 36.9; females, 29.1) and Georgia for males (58.3), followed by Florida (total, 36.0; males, 57.0; females, 16.0) (Table 7). Use caution when comparing the rates of diagnoses for the District of Columbia to the rates for states.
A Look at Disparities in Diagnoses of HIV Infection by Income Inequality
In 2019, the disparities of HIV diagnosis by health insurance coverage for adults were as follows:
Absolute disparities (rate difference): If males or females in the lowest insurance coverage tracts lived in the highest insurance coverage tracts, then 27 cases and 7 cases per 100,000 population, respectively, would have been prevented (Table 1).
Relative disparities (rate ratio): Among males, the rate of diagnoses in the lowest income tracts was 4.1 times the rate in the highest income tracts, and among females, the rate in the lowest income tracts was 6.2 times the rate in the highest income tracts (Table 1).
For absolute and relative disparities for sex at birth stratified by age group and race/ethnicity, see Figures 10a/b and 11a/b.
See Technical Notes for additional information on disparity measures.
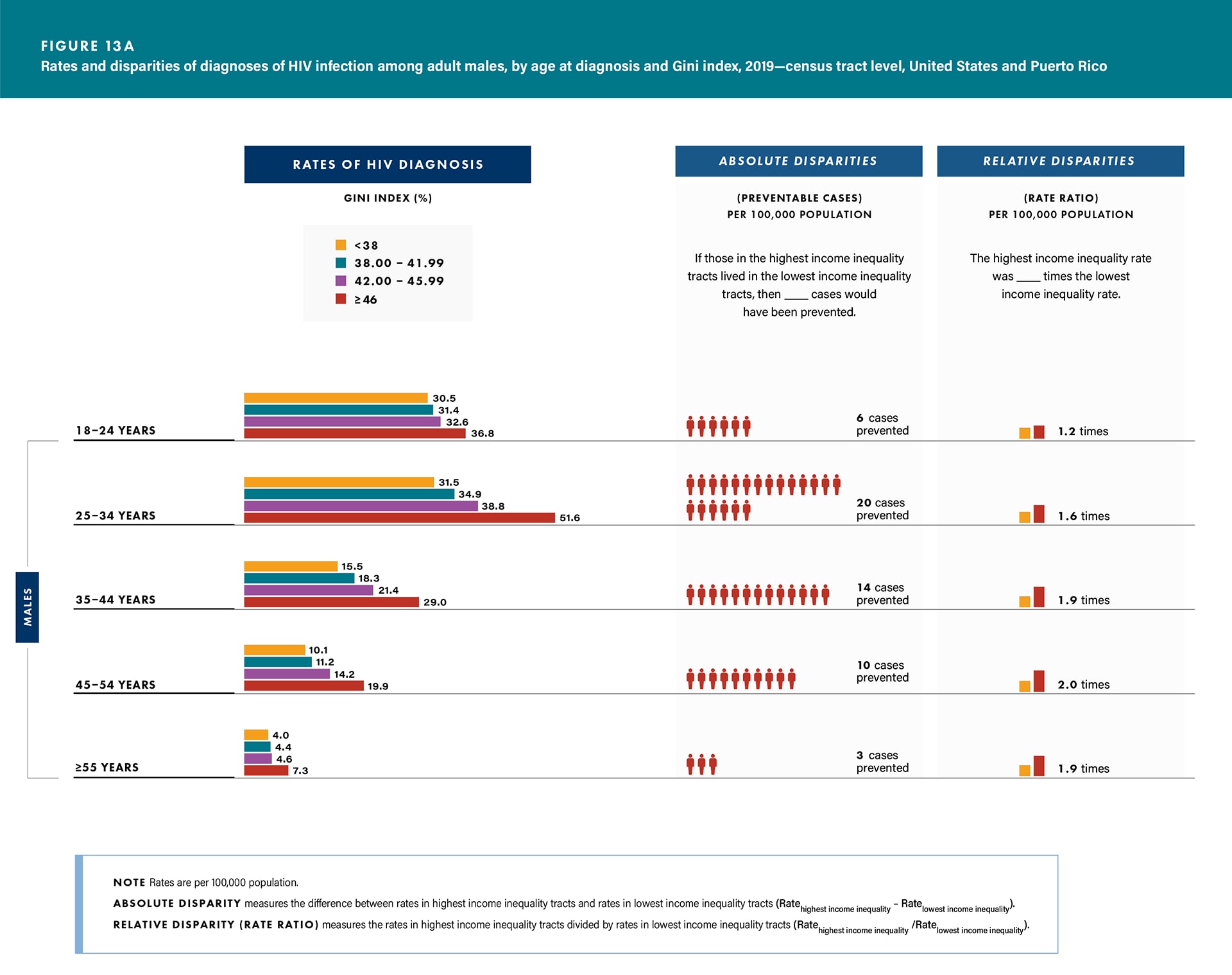
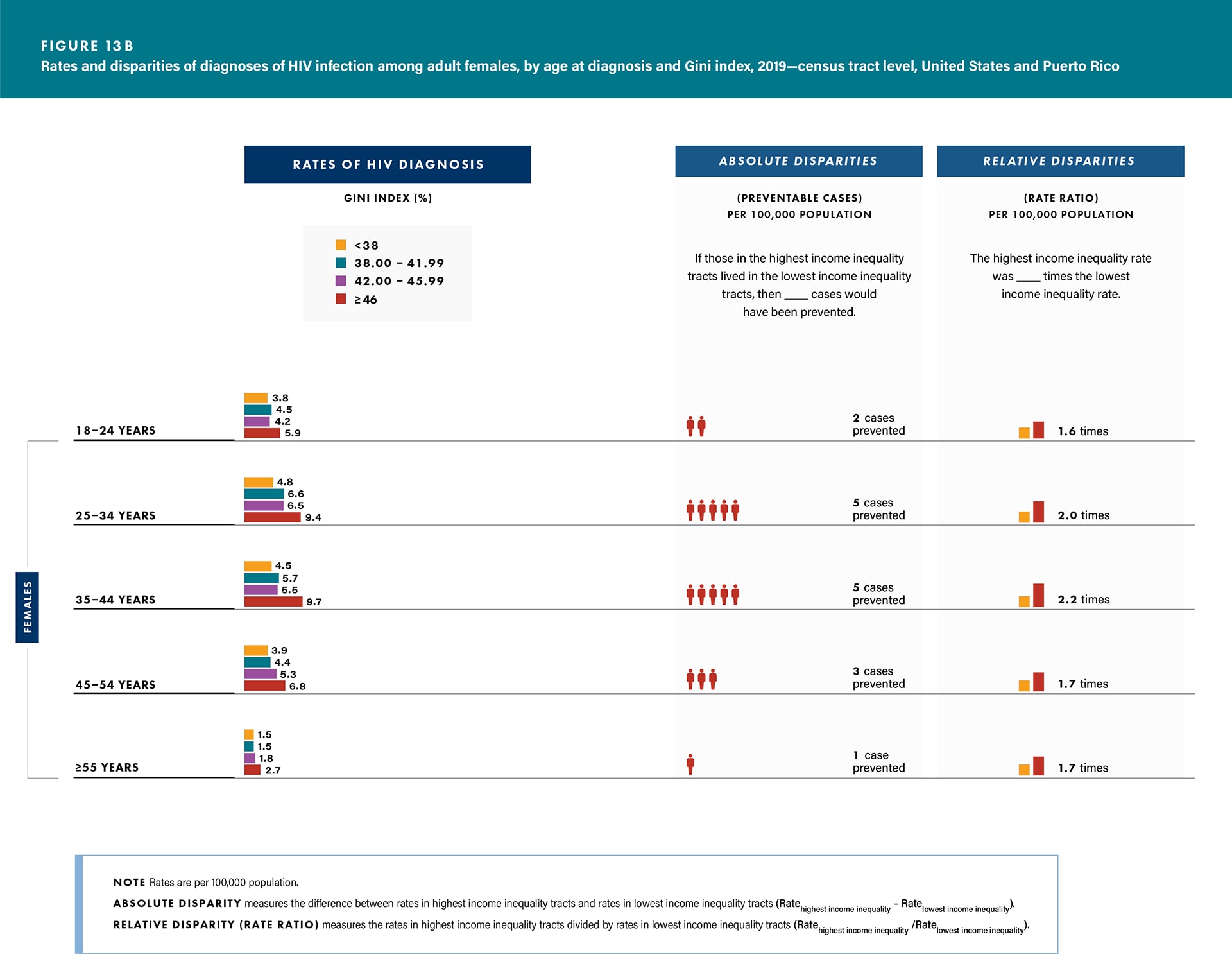
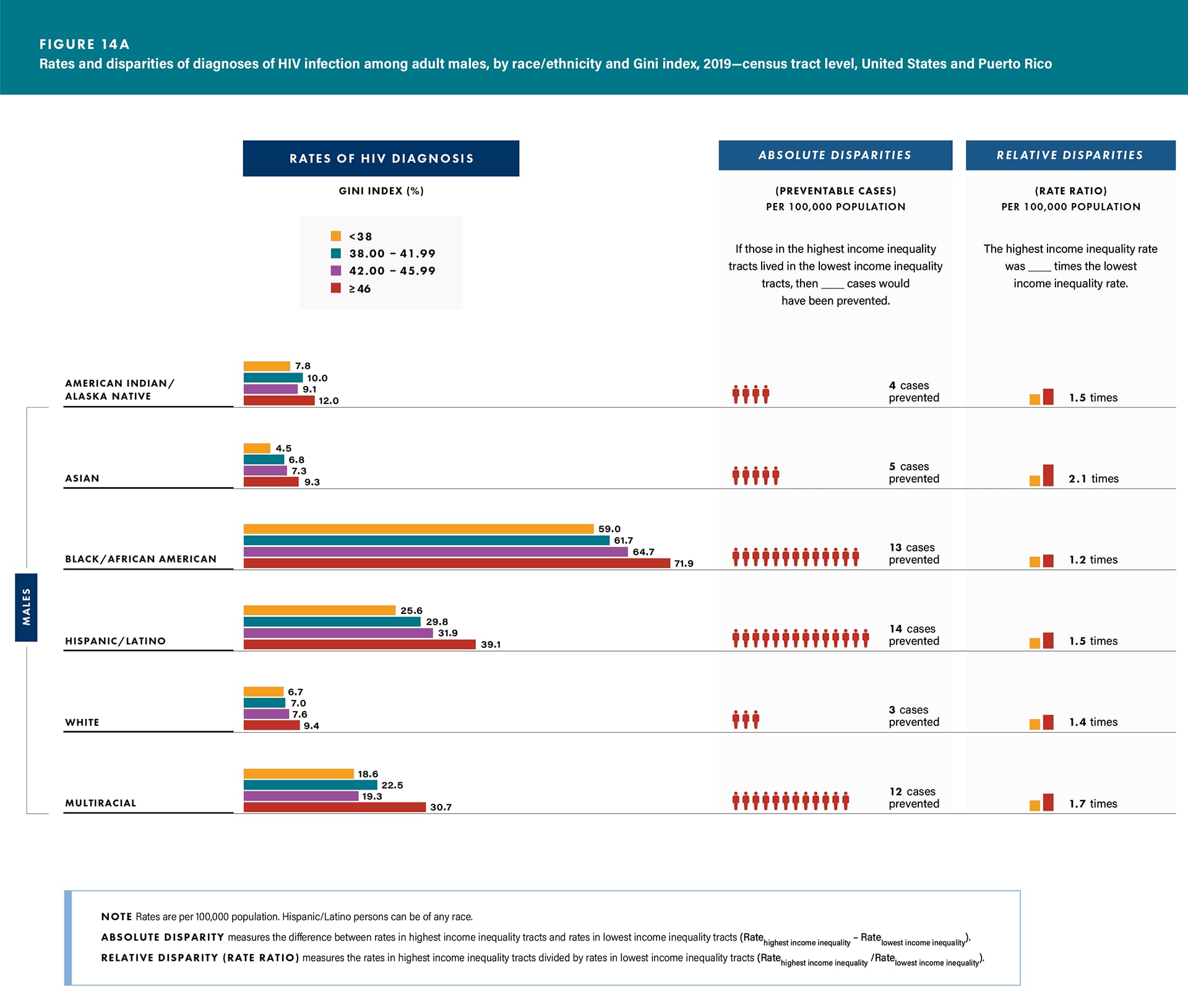
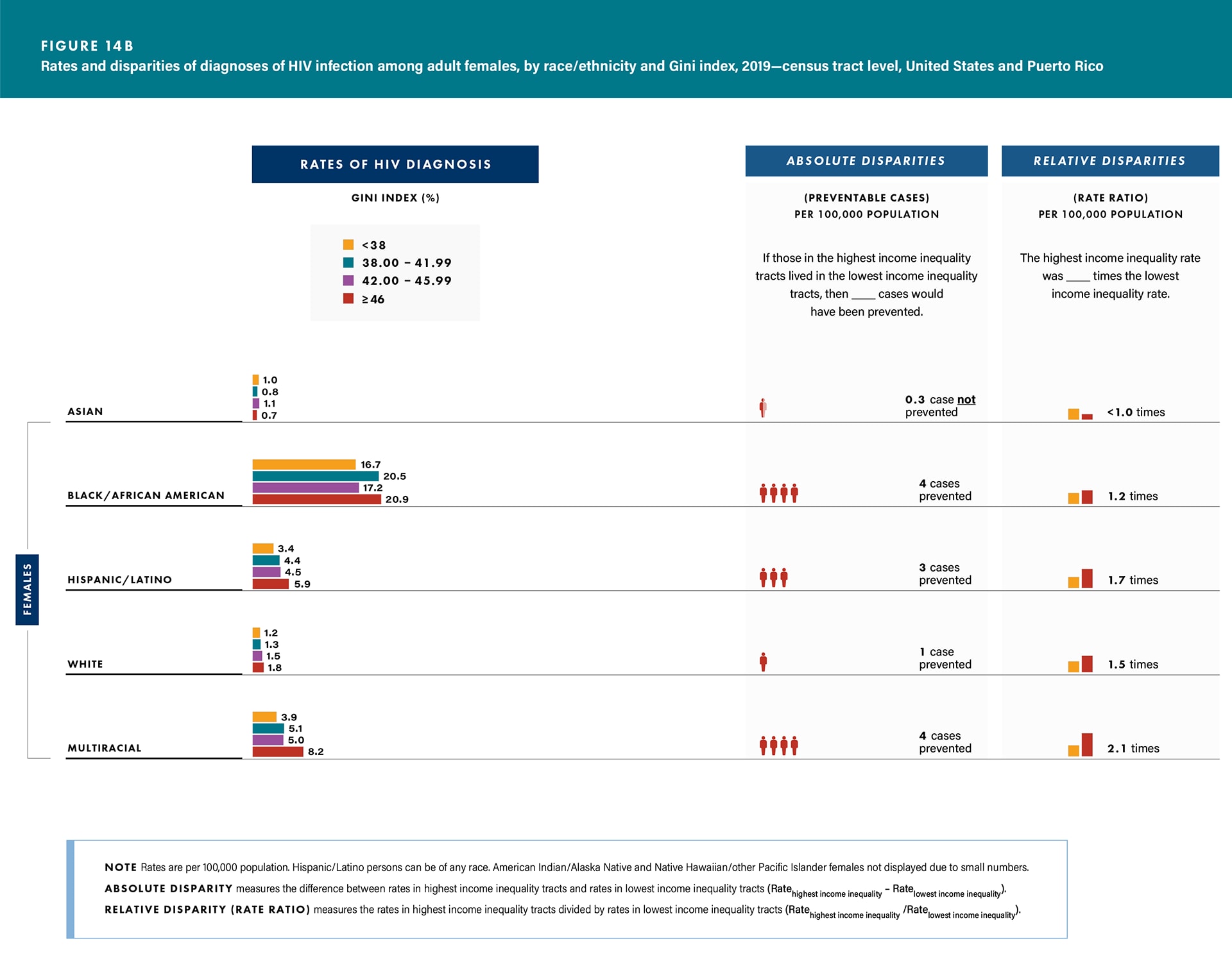
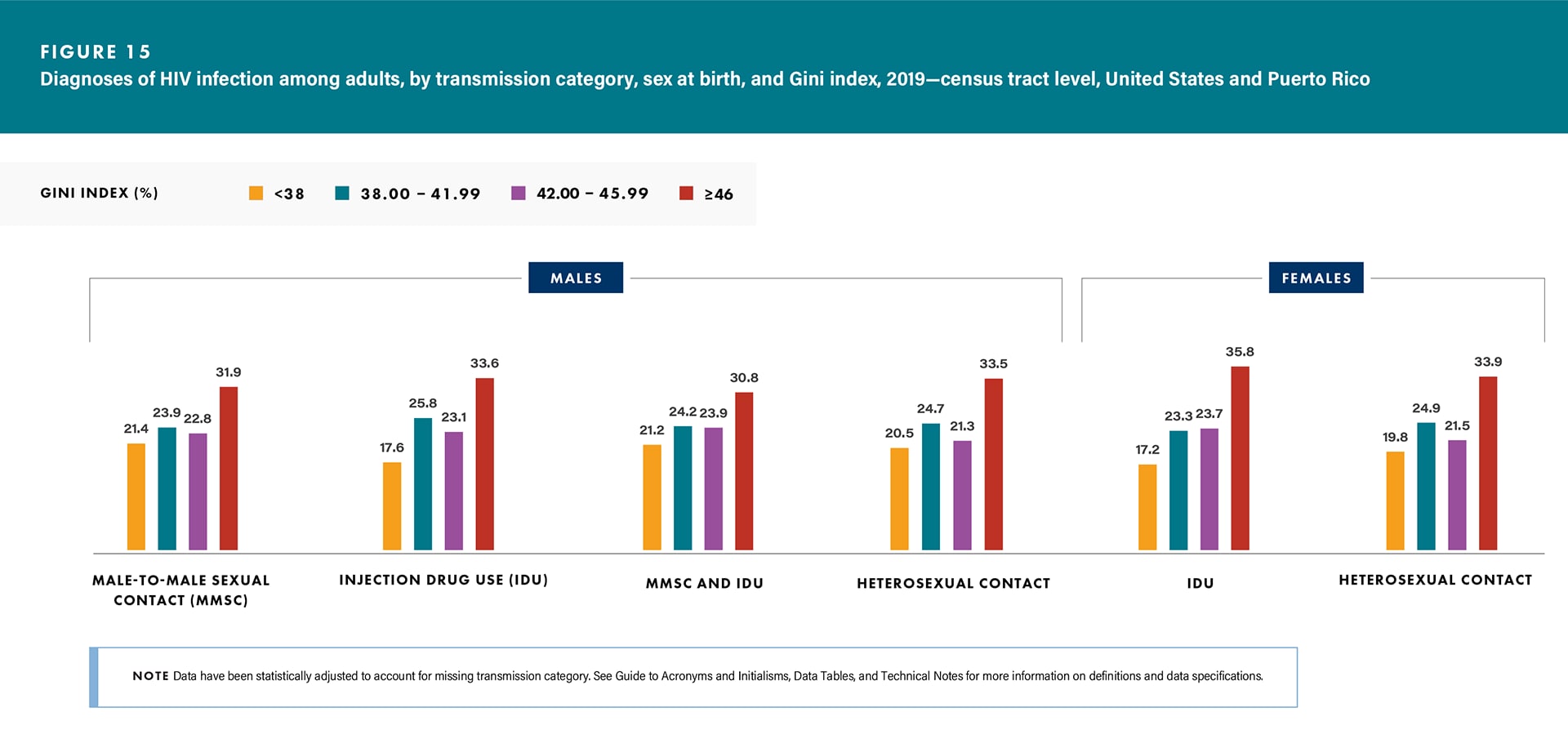
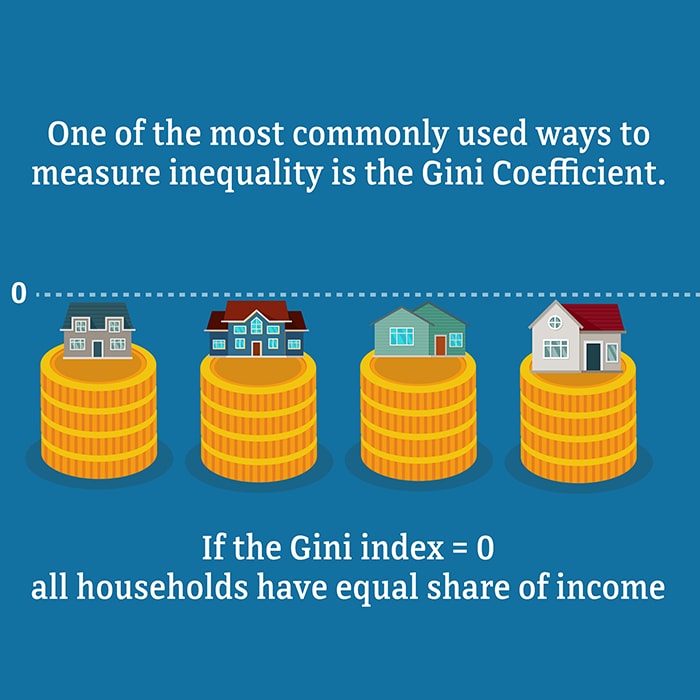
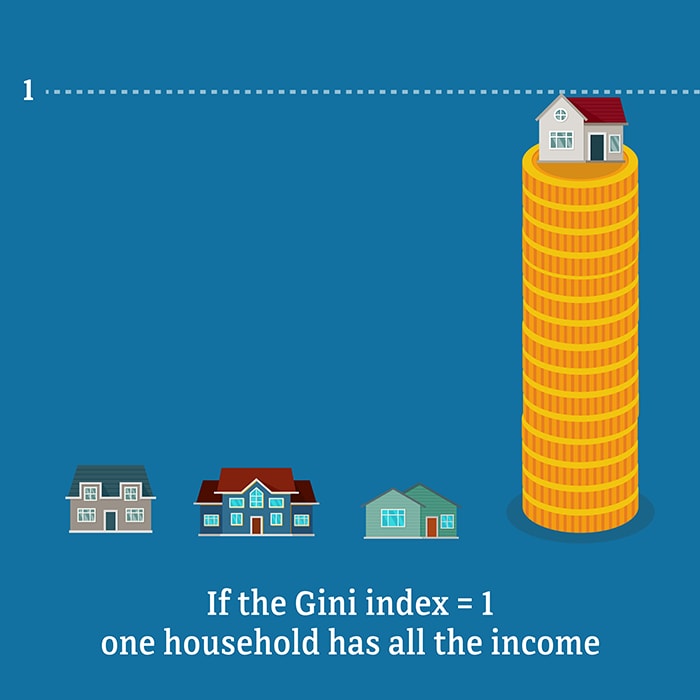
Income Inequality (Gini Index)
Poor health and income inequality are connected. Income inequality and socioeconomic deprivation are 2 key socioeconomic determinants of HIV diagnosis and care outcomes. High levels of income inequality may negatively affect the health of everyone, even the affluent, mainly because income inequality reduces social cohesion, which leads to more stress, fear, and insecurity [19]. Many factors—education and the historical legacy and impact of discrimination—are key components of income equality [20]. Many of these same factors contribute to disparities in HIV diagnoses; however, sex at birth and race/ethnicity components can also contribute to this disparity.
This report uses the Gini index, which summarizes income distribution, to measure income inequality. The Gini index ranges from 0 or 0%, indicating perfect equality (i.e., lowest income inequality—where all households have an equal share of income), to 1 or 100%, perfect inequality (i.e., highest income inequality—where only 1 household has all the income and the rest have none).
In 2019, adults who lived in census tracts with the highest income inequality (where income inequality was 46% or more) accounted for
- the highest HIV diagnosis rates or percentages (diagnoses),
- the lowest percentages of adults linked to HIV medical care ≤ 1 month after receiving a diagnosis (linkage), and
- the lowest percentages of adults with suppressed viral load within 6 months of receiving an HIV diagnosis (viral suppression) among
Sex at birth:
- Diagnoses—rates: males, 25.2; females, 5.9 (Table 1).
- Linkage—lowest percentage linked to care was not in highest income inequality group for either sex (Table 9).
- Viral suppression—males, 68.6% (Table 9).
Age group:
- Diagnoses—all age groups for both sexes (Figures 13a/b and Table 1).
- Linkage—age groups 18–24 and 45–54 years for males and age groups 35–44 and ≥ 55 years for females (Table 9).
- Viral suppression—all age groups for both sexes (except age group 18–24 years for males and age groups 25–34, 45–54, and ≥ 55 years for females) (Table 9).
Race/ethnicity:
- Diagnoses—all racial/ethnic groups for both sexes (except Asian females) (Figures 14a/b and Table 2).
- Linkage—Black/African American males (76.9%) and multiracial females (78.3%) (Table 10).
- Viral suppression—Black/African American males (63.5%) and females (69.1%), Hispanic/Latino males (72.7%), and multiracial females (65.0%) (Table 10).
Transmission category:
- Diagnoses—all transmission categories for both sexes (Figure 15 and Table 3).
- Linkage—heterosexual contact for males (Table 11).
- Viral suppression—MMSC (70.2%), IDU (56.3%), and heterosexual contact (61.4%) among males (Table 11).
- Among males with infection attributed to MMSC,
- Linkage—Black/African American (77.6%) and White (84.5%), and
- Viral suppression—Black/African American (64.5%) and Hispanic/Latino (74.5%) (Table 12).
Area of residence: rates: District of Columbia (total, 42.5; males, 66.9; females, 22.1), followed by Georgia (total, 30.9; males, 52.2) and Maryland for females (15.5) (Table 8). Use caution when comparing the rates of diagnoses for the District of Columbia to the rates for states.
A Look at Disparities in Diagnoses of HIV Infection by Income Inequality
In 2019, the disparities of HIV diagnosis by income inequality for adults were as follows:
Absolute disparities (rate difference): If males or females in the highest income inequality tracts lived in the lowest income inequality tracts, then 10 cases and 3 cases per 100,000 population, respectively, would have been prevented (Table 1).
Relative disparities (rate ratio): Among males, the rate of diagnoses in the highest income inequality tracts was 1.6 times the rate in the lowest income inequality tracts, and among females, the rate in the highest income inequality tracts was 1.8 times the rate in the lowest income inequality tracts (Table 1).
For absolute and relative disparities for sex at birth stratified by age group and race/ethnicity, see Figures 13a/b and 14a/b. See Technical Notes for additional information on disparity measures.