Health Equity in Action: CORE
Health equity is when everyone has the opportunity to be as healthy as possible. As an agency, CDC is transforming its public health research, surveillance, and implementation science efforts to shift from simply listing the markers of health inequities to identifying and addressing the drivers of these disparities.

CDC has offices in four Central Asia countries and partners with ministries of health in each to address COVID-19 and HIV, and to strengthen public health emergency management, laboratory, surveillance, and workforce capacity to respond to disease outbreaks. Credit: Sharakhmedov Hamdam, Golden Ministries.
Published in 2022, CDC’s Global Health Equity Strategy commits the agency for the first time to advance health equity through a comprehensive approach. CDC’s Global Health Equity Strategy applies the CORE framework to the agency’s global health functions to drive health equity into CDC’s global programs. This includes coordinating efforts to promote CORE implementation and accelerate innovative improvements.
CDC’s Global Health Equity Strategy builds upon a human-rights based approach to specifically address the availability, accessibility, acceptability, and quality of global health programs. It acknowledges that the right to health can be pursued by numerous and complementary approaches. Specific programmatic and cross-cutting goals in CDC’s Global Health Equity Strategy help countries eliminate health disparities and highlights determinants of health that negatively impact historically, socially, or geographically excluded or marginalized groups.
Cultivating Comprehensive Health Equity Science
CDC embeds health equity principles into the design, implementation, and evaluation of its research, data surveillance, and intervention strategies. CDC aims to build health equity data science capacity to conduct, translate, and disseminate analysis or statistical studies and use multi-level modelling and predictive analytical approaches. This includes prioritizing science agendas that build the evidence base for eliminating health inequities.
Health Equity in Action: How CDC Helps Those with Lymphatic Filariasis

Lymphatic filariasis (LF) is a leading cause of permanent disability worldwide. Some people with LF develop lymphedema (fluid collection and swelling, which often affects people's legs).
Lymphatic filariasis (LF), often known as elephantiasis, is a neglected tropical disease (NTD) caused by microscopic, thread-like worms spread by the bite of an infected mosquito. LF affects more than 50 million people throughout Asia, Africa, the Western Pacific, and parts of the Caribbean and South America. CDC collaborates with United States Agency for International Development’s NTD Program, ministries of health and in-country partners, and other global health organizations to leverage $26 billion in donated drugs to accelerate elimination of LF and other NTDs.
Nevertheless, millions of people already suffer from the debilitating effects of NTDs and need ongoing treatment and care. CDC continues to work with partners to eliminate new LF infections, including supporting mass drug administration campaigns in Haiti and American Samoa. CDC also develops tools and guidance, generates data, and administers trainings to help people who already have LF.
In Kolondiéba, Mali, a 47-year-old mother of eight named Mia has suffered with the painful symptoms of LF for more than 30 years. Because of her LF infection, Mia’s lymphatic system does not function properly, and she frequently deals with painful fluid build-up and episodes of skin infection that leave her bed-ridden and her children without care.
Several years ago, Mia participated in a morbidity management and disability prevention program offered by Mali’s Ministry of Health, with technical expertise from CDC and CDC Foundation. She learned essential lymphedema management, and since going through the training, her acute episodes have dwindled and the pain in her legs has become manageable. She is proud of how she is able to care for her own health and children again.

Mia has suffered from the painful effects of lymphatic filariasis (LF) for decades. Morbidity management and disability prevention (MMDP) trainings have helped her learn how to better manage her symptoms. Credit: Caitlin Worrell, CDC
“Since the beginning of CDC’s lymphatic filariasis program, we have realized that we can prevent future generations from suffering the consequence of this disease without losing sight of those who already suffer from its debilitating impacts,” says Caitlin Worrell, a CDC epidemiologist. “With such a large, global focus on prevention, those who already have diseases can sometimes be forgotten. It’s definitely a big challenge to ensure everyone is cared for.”
“People with filarial lymphedema and hydrocele not only feel socially stigmatized but suffer economically,” notes Emily Toubali, the LF Technical Advisor in USAID’s NTD Division. “Bringing care and treatment to those who have morbidity associated with LF means that the most marginalized are being reached by the health system with a set of interventions that directly improve their quality of life.”
CDC collaborated with the International Organization for Migration to conduct a quality assurance review of the Guatemala Youth Survey. The survey includes data on violence and health from indigenous populations from the Northern Highlands region of Guatemala. These groups have been historically under-represented in statistical reports in Guatemala, leading to inequities and disenfranchisement. The quality assurance review provided recommendations for the Government of Guatemala regarding the analysis, interpretation, and application of survey results. Additionally, CDC provided a final report of survey findings and led a workshop in Guatemala to develop responses to address the findings. With a focus on promoting health equity of indigenous populations in Guatemala, these efforts led to a redefined national framework for building the resiliency of communities and protecting children from violence.
Health Equity in Action: Combating Hepatitis B Infections
CDC uses its Global Immunization Strategic Framework to guide investments in building global immunization program capacity and scientific expertise to advance the control, elimination, and eradication of vaccine-preventable diseases. The framework prioritizes vaccine equity and coverage and works to identify and reach under-immunized populations with tailored delivery strategies.
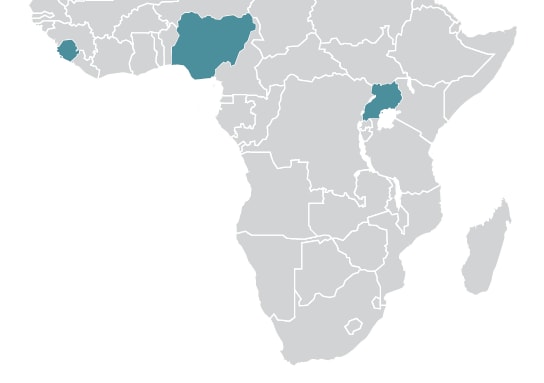
Using this framework, CDC supports several countries throughout the African region, which has the highest rates of hepatitis B virus infection in children:
- In Sierra Leone, a study conducted by CDC revealed that most of the infections among children are due to mother to child or early childhood transmission of infection due to the absence of hepatitis B birth dose vaccination (HepB-BD).
- In Uganda, CDC supported the National Immunization Technical Advisory group to compile the evidence needed to recommend the introduction of HepB-BD.
- In Nigeria, CDC is implementing interventions to improve timely HepB-Dd coverage. Nigeria has the highest number of children infected with hepatitis B globally, yet timely HepB-BD coverage is fewer than 50%.
Progress towards the elimination of mother-to-child transmission of HepB-BD continues. In 2020, 190 (98%) of 194 countries had introduced universal infant hepatitis B vaccination compared with 186 (96%) in 2016.
Optimizing Interventions
CDC uses scientific, innovative, and data-driven intervention strategies to address environmental, place-based, occupational, policy, and systemic factors that impact health outcomes to address the drivers of health disparities. This includes transforming surveillance systems to include drivers of health disparities and inequities and implementing key multi-sector policy levers to advance health equity.
Health Equity in Action: CDC Support Improves Uzbekistan’s Detection of COVID-19
Preparations to improve Uzbekistan’s ability to respond to public health emergencies were well under way before COVID-19 arrived. With support from CDC, Uzbekistan’s government and Ministry of Health were already in the process of building a public health emergency management (PHEM) program to respond to public health emergencies.
CDC recommended that the Government of Uzbekistan develop a public health emergency program that would help the government protect the health of its people. Just six months later, the Government of Uzbekistan officially opened its public health emergency operations center (PHEOC). The establishment of this PHEOC was supported by CDC’s Country Office in Uzbekistan along with partners such as Integral Global and the U.S. Civilian Research and Development Foundation. Uzbekistan’s PHEM program puts the Uzbekistani Ministry of Health in a better position to assess public health threats and take steps to ensure strong coordination and decision-making. The creation of Uzbekistan’s PHEM program, like programs in neighboring Kazakhstan, Tajikistan, and Kyrgyzstan, helps to train staff to lead public health responses and better prepare for the next public health emergency.
In the past year, 36 public health experts, including 24 epidemiologists were trained at Uzbekistan’s PHEOC on how to participate in an emergency response.
“As we grew to understand this virus [COVID-19], it really became more about figuring out how we were going to work together with health officials in Uzbekistan,” says Dr. Daniel Singer, U.S. CDC’s Central Asia director at the time. “It was important for us to understand what capabilities Uzbekistan already had in place to limit the spread of COVID-19 so we could determine how to best assist them.”

Public health specialists work on Uzbekistan’s COVID-19 response in the new PHEOC. The CDC team in Uzbekistan trained the national PHEOC core staff in and will continue training staff in health departments throughout the country. Credit: Hamdam Sharakhmedov, Golden Ministries
Health Equity in Action: Training Youth Mentors
U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) implements the DREAMS (Determined, Resilient, Empowered, AIDS-Free, Mentored, and Safe) program aimed at reducing the high rate of HIV infection among girls and young women. CDC supports implementation of DREAMS in Haiti and 12 sub-Saharan African countries where girls and young women are five to 14 times more likely to be infected with HIV than their male peers. They are also more likely to experience gender-based violence — putting them at increased risk of HIV infection while impacting their ability to access HIV prevention and response services. Grounded in equity, DREAMS focuses on the economic, social, cultural, behavioral, and biomedical factors that put adolescent girls and young women at risk for HIV by empowering them to make informed choices about their health.
DREAMS mentors are older peers and support the implementation of programming by serving as confidants to DREAMS participants and assisting them in building positive relationships within their support networks. Mentors also work to promote active linkages to needed services.
“I was chosen and trained to be a DREAMS mentor and to represent other girls. Here I built my circle and impacted the lives of many girls and changing their stories with my life story, being a voice for the voiceless girls, and identifying the most vulnerable girls to benefit from DREAMS services.” – Mozambique DREAMS Mentor

CDC’s implementing partners train mentors to respond to disclosures of violence through an adapted first-line support approach called LOVES (Listen, Ongoing Connection, Validate, Encourage Safety, Support). Through LOVES, mentors gain hands on skills on how to validate and support participants and refer them to appropriate services. In 2022, CDC conducted four virtual LOVES trainings with 275 implementing partner staff in 15 countries.
As a result of DREAMS and LOVES training, the most marginalized adolescent girls and young women are now receiving support from trained and skilled mentors, along with improved access to needed post-violence care and sexual and reproductive health resources and services. DREAMS continues to prioritize empowering girls and young women and reducing gender health disparities.
Health Equity in Action: Measles Vaccinations During Humanitarian Crisis in Ethiopia
The ongoing humanitarian crisis in Tigray that began in 2020 led to interruptions in most health services and major increases in internally displaced persons (IDPs). In early January 2022, the Government of Ethiopia, with support from the Measles and Rubella Initiative (MRI), conducted an integrated vaccination and nutrition screening campaign in Tigray.
Prior to the conflict, Tigray had relatively low routine immunization coverage and frequently reported outbreaks of measles. The disruption of immunization services combined with an influx of IDPs created an increased risk of vaccine preventable diseases outbreaks, particularly measles. A rapid nutrition assessment showed high levels of acute malnutrition, which leads to higher rates of severe measles disease and deaths. In close partnership with the MRI Outbreak Response Working Group and MRI Management Team, CDC worked with the World Health Organization, UNICEF, and other partners to vaccinate over 760,000 children under 5 against measles in 52 woredas (Ethiopian administrative divisions). The integrated campaign also included nutrition screenings, vitamin A distribution, and deworming.
Health Equity in Action: Shifting to Virtual Laboratory Trainings
When all but CDC’s mission-critical activities were postponed due to the COVID-19 pandemic, CDC staff saw the need to continue to help countries strengthen their laboratory diagnostics and capacity within national reference laboratories. The agency’s Bacterial Meningitis Laboratory and Pertussis and Diphtheria Laboratory pivoted from on-site trainings for outbreak response and preparedness to an innovative series of live virtual trainings. These trainings helped over 24 countries in Africa, Central America, and South America to be better equipped to tackle the seasonal epidemics of bacterial meningitis and sporadic outbreaks of diphtheria that continue to occur globally. CDC’s real-time response to a global health need provided state-of-the-art, culturally appropriate, laboratory trainings with simultaneous translations in English, Spanish, French, and Portuguese. CDC enhanced in-country capacity to diagnose and respond to outbreaks that disrupt the lives of thousands of people annually by providing trainings that were not restricted by geographic distance or financial constraints.

A lab technician operates an automated viral load testing machine at the CDC-supported National Health Laboratory and Diagnostic Services facility in Uganda. Credit: Chris Lubega, U.S. Embassy Uganda
Reinforcing and Expanding Robust Partnerships
Through worldwide collaboration, CDC enhances cross-cutting coordination on health equity through partnerships, extramural support, and external communication. This allows CDC to seek out and strengthen sustainable multi-level, multi-sectoral, and community partnerships to advance health equity.
Health Equity in Action: CDC and Tanzania Speed Up COVID-19 Vaccinations
For more than 30 years, CDC has been at the forefront of the fight against HIV and TB in the United States and around the world. Through PEPFAR, CDC provides HIV and TB treatment services in 11 districts on Tanzania’s mainland and the island of Zanzibar. By leveraging PEPFAR’s reach, more than 40% of people with HIV and 80-90% of CDC-supported partner staff, community, and health facility workers received at least one dose of COVID-19 vaccine during the six-week surge campaign.
Tanzania was one of 11 countries selected to receive additional support from the U.S. government’s Initiative for Global Vaccine Access (Global VAX) program in June, 2022. With the additional Global VAX support, CDC and partners launched a broad vaccination campaign in Dar es Salaam and other regions, including remote areas around Tanzania’s lake zones.
In many low- and middle-income countries, geographical barriers can be a major impediment for populations to access health services and life-saving prevention tools, further exacerbating inequities and health disparities. CDC staff sometimes traveled 200 miles each way to make sure COVID-19 vaccines were available to people in remote areas by setting up temporary vaccination sites with partners already engaged in HIV prevention through PEPFAR. The sites provided COVID-19 vaccinations along with other health services like blood pressure screening and reproductive health services.
With CDC Tanzania’s support, nearly half of the eligible population received the primary series of COVID-19 vaccines as of September 2022.

U.S. CDC’s Oscar Rwabiyago, MD, observes a healthcare worker as she performs all the services offered at this mobile health clinic. U.S. CDC in Tanzania and HIV-prevention partners set up a temporary clinic in the Ilemela District of the Mwanza Region. It provided access to COVID-19 vaccines and other healthcare services including HIV testing and counseling. Credit: Kokuhabwa Mukurasi, CDC Tanzania.
Health Equity in Action: Improving Healthcare Safety in East Africa
In low- and middle-income countries (LMICs), safe delivery of health services can be challenging due to lack of investment in infection prevention and control programs, leading to higher rates of healthcare-associated infections (HAIs) and antibacterial resistance (AR). HAIs and AR disproportionately impact vulnerable populations in LMICs. Establishing communities of practice in these countries provides an efficient and cost-effective method for training and mentoring healthcare workers. The communities of practice support development, implementation, and strengthening of IPC programs and prepare those on the frontlines to keep themselves and their patients safe.

Individuals and families are waiting in line to be screened for COVID-19 in Ethiopia. Credit: CDC Ethiopia
CDC supported ICAP at Columbia University to establish the East Africa Infection Prevention and Control (EA IPC) Network in 2020, a community of practice aimed at building healthcare worker capacity to improve adherence with IPC standards. The network aims to reduce the incidence of COVID-19 and healthcare-associated infections and includes 20 hospitals in Ethiopia, Kenya, Tanzania, and Uganda. Network activities include weekly case-based learning sessions, collaborative quality improvement projects, facility assessments to evaluate IPC performance for COVID-19, and tailored professional development.
When a new outbreak of Ebola caused by Sudan ebolavirus was declared in Uganda in September 2022, the EA IPC Network rapidly responded with a webinar presented by the Ugandan Ministry of Health. Almost 100 participants from across East Africa attended to share and learn about the response and preparedness activities already underway. The network will continue to leverage its existing activities to disseminate key Ebola prevention and control information.
The region of Quiché, located in northwest Guatemala, has a population of 1.6 million people – 88% of which are indigenous and 90% live in poverty. With no HIV care or treatment center in Quiché, the 305 people previously diagnosed were forced to travel an average of 2.5 hours to seek HIV care and treatment. In Quiché and other regions, indigenous communities have organizations led by a local leader called Alcalde Indígena who represents their community in a municipal and provincial organization. CDC engaged the Alcalde Indígena of Santa Cruz Del Quiché, Mr. Juan Zapeta, and the Director of the Hospital of Santa Cruz del Quiché, Dr. Salomón Delgado, who gave their support to opening the care and treatment center in the Regional Hospital of Santa Cruz Del Quiché in April 2022. Indigenous people living with HIV in Quiché now have better access to HIV care and treatment, helping to reduce health inequities in this vulnerable population.
Enhancing Capacity and Workforce Engagement
CDC builds workforce capacity and engagement by developing internal capacity to create a multi-disciplinary workforce with more inclusive climates, policies, and practices for a broader a public health impact.
The Birth Defects Surveillance Toolkit (available in both English and Spanish) is a collaborative effort between the International Clearinghouse for Birth Defects Surveillance and Research, the World Health Organization, and CDC that is used globally to enhance capacity and workforce training on identification and surveillance of major external birth defects. The toolkit builds internal capacity to cultivate a multi-disciplinary workforce with more inclusive climates, policies, and practices.
Health Equity in Action: PulseNet International – Building Capacity in the Asia Pacific Region

A public health scientist from CDC’s PulseNet team analyzing whole genome sequencing (WGS) data on a sequencing instrument. WGS provides detailed genetic information about pathogens that cause foodborne outbreaks. Credit: Lauren Bishop, CDC
Globally, antibiotic resistance (AR) is a growing concern and is one of the top global health threats facing humanity according to the World Health Organization. As a result, global initiatives have been developed to support surveillance and identify emerging drug-resistant strains circulating within regions and globally. PulseNet International was established in the early 2000s as a worldwide network for detecting foodborne disease clusters and outbreaks using molecular subtyping methods such as whole genome sequencing. PulseNet International recently joined a larger CDC initiative, the Global Antimicrobial Resistance Laboratory & Response Network, focusing on building laboratory capacity for antibiotic resistance surveillance within PulseNet International regions.
This year, CDC, the Association of Public Health Laboratories, and other PulseNet International partners launched a feasibility study targeting four low- and middle-income countries within the Asia Pacific region to demonstrate the impact of the PulseNet surveillance system for detecting potential foodborne outbreaks and monitoring emerging antibiotic resistance trends. A key goal of this study is to determine feasibility and encourage the development of whole genome sequencing and analysis capacity for antibiotic resistance surveillance in the Asia Pacific region. This study will also allow participating countries to improve access to sequencing, ability to analyze data, and data sharing globally. CDC will provide laboratory and data analysis training and technical assistance to participating laboratories throughout the project.
Health Equity in Action: Cultivating Health Equity Through Training in the Vietnam Country Office

Outpatient clinic in Mai Son District, Son La Province, Vietnam. Credit: CDC Vietnam
In September 2022, CDC’s Country Office in Vietnam became the first overseas U.S. Department of Health and Human Services (HHS) office to receive health equity training supported by the HHS Equity Technical Assistance Center (ETAC). A team comprised of ETAC consultants, and CDC and HHS staff adapted equity training materials originally developed for a U.S. domestic audience to be applicable to the Vietnamese context. The training enabled CDC Vietnam staff – Americans and Vietnamese – to better understand equity principles and apply those principles in their work. Responding to results from an equity landscape assessment of CDC Vietnam staff, the training also provided a foundational understanding of equity, incorporating contextual background from the United States and Vietnam.
Topics included distinguishing equity versus equality, understanding intersectionality, and operationalizing equity principles. In addition to CDC Vietnam leadership, U.S. Embassy Hanoi Deputy Chief of Mission Melissa Bishop provided closing remarks, noting, “[equity] is not a one-time action; it is a consistent lens we can apply to everything we do.” She commended CDC Vietnam for “establishing Vietnam as a champion for equity in the health sphere.”
Four weeks after the training, 89% of participants indicated that it helped them understand how to advance health equity through their work. CDC’s Country Office in Vietnam will continue to affirm its commitment to health for all, with the consistent and deliberate advancement of health equity principles and approaches within its science, interventions, partnerships, and policies. The lessons learned from this pilot training in Vietnam will inform scaling of equity support to other CDC overseas offices, ensuring CDC beneficiaries across the globe can achieve their highest attainable level of health.