
Developing Interventions
James L. Hadler, Jay K. Varma, Duc J. Vugia, and Richard A. Goodman
All scientific work is incomplete—whether it be observational or experimental. All scientific work is liable to be upset or modified by advancing knowledge. That does not confer upon us a freedom to ignore the knowledge we already have, or to postpone the action that it appears to demand at a given time.
— Sir Austin Bradford Hill, British Epidemiologist (1897–1991) (1)
Public health officials who have responsibility and legal authority for making decisions about interventions should consider certain key principles: selecting the appropriate intervention, facilitating implementation of the intervention, and assessing the effectiveness of the intervention (Box 11.1).
- As soon as an acute public health problem is detected, a public health responsibility and societal expectation exist to intervene as soon as possible to minimize preventable morbidity and mortality.
- Public health interventions should be scientifically driven on the basis of established facts and data, current investigation findings, and knowledge from previous investigations and studies. Although salient sociopolitical forces (e.g., public fear or political outcry) might create pressures for rapid public health interventions, the interventions must be based on evidence. However, adapting certain intervention components might be necessary to make them more acceptable and responsive to the needs of the affected community, potentially affected persons, elected officials, and the media.
- For any given problem, the type(s) and number of interventions to be implemented will vary, depending on the nature of the acute problem, including its cause, mode of spread, and other factors.
- The type(s) and number of interventions used might evolve as a function of incremental gains in information developed during the investigation.
- Most public health interventions demand—and even might be potentiated by—open, two-way communication between involved government agencies and the public.
Field epidemiologists must consider multiple crucial determinants during the course of making a decision about whether a scientifically rational basis exists for employing an intervention and when selecting one or more specific interventions optimally matched to the public health problem. These determinants, which might be both interrelated and not mutually exclusive, encompass a constellation of factors (e.g., specific knowledge of causative etiologic agent[s] and of reservoirs or mode[s] of acquisition or spread) and recognition of other causal determinants as reflected, in part, by assessing the investigation’s ability to address the causation criteria (see the following section). This section examines three highly interrelated key determinants: severity of the problem, levels of certainty about key epidemiologic factors, and causation criteria. Additionally, it considers the sociopolitical context and its possible role in determining interventions.
Severity of the Problem
The severity of a specific problem is a principal determinant of the urgency and course of a field investigation and of any early intervention. The greater the severity, the sooner a public health intervention is expected. The primary determinants of severity are the consequences of the event and the probability of the event occurring. Consequences to consider include the most common symptoms and syndrome caused, duration of illness, complications including hospitalization and case-fatality rates, need for treatment, and economic impact. The consequences, even more than the probability, tend to drive perception of the importance of intervening.
One example is botulism, which is a low-probability but high-consequence event. Virtually all US cases trigger extensive epidemiologic investigations because identifying the food or beverage source can prevent additional intoxications, and identifying exposed or ill persons enables administration of life-saving antitoxin. Similarly, clusters of a healthcare-associated infection—especially among postsurgical or immunocompromised patients—are often investigated because of the potential for serious complications and greatly prolonged hospitalization, the possibility of iatrogenic illness as an avoidable medical event, and the immediate need to resolve questions about the safety of continuing to admit patients to the hospital (2).
Levels of Certainty About Agents, Sources, and Modes of Spread
In addition to severity, a spectrum of other factors influences the aggressiveness, extent, and scientific rigor of an epidemiologic field investigation. In the prototypic investigation, control measures are formulated only after other steps have been implemented (see Chapter 3). In practice, however, control measures might be appropriate or warranted at any step in the sequence. For most outbreaks of acute disease, the scope of an investigation is dictated by the levels of certainty about (1) the etiology of the problem (e.g., the specific pathogen or toxic agent) and (2) the source or mode of spread (e.g., waterborne, airborne, or vectorborne) (3). When the problem is identified initially, the levels of certainty about the etiology, source, and mode of spread can range from known to unknown (Figure 11.1). These basic dichotomies are illustrated in Figure 11.1 by four examples that represent the extremes. In certain situations, control measures follow policy or practice guidelines; in others, interventions are appropriate only after exhaustive epidemiologic investigation. Preliminary control measures often can start on the basis of limited initial information and then be modified as investigations proceed.
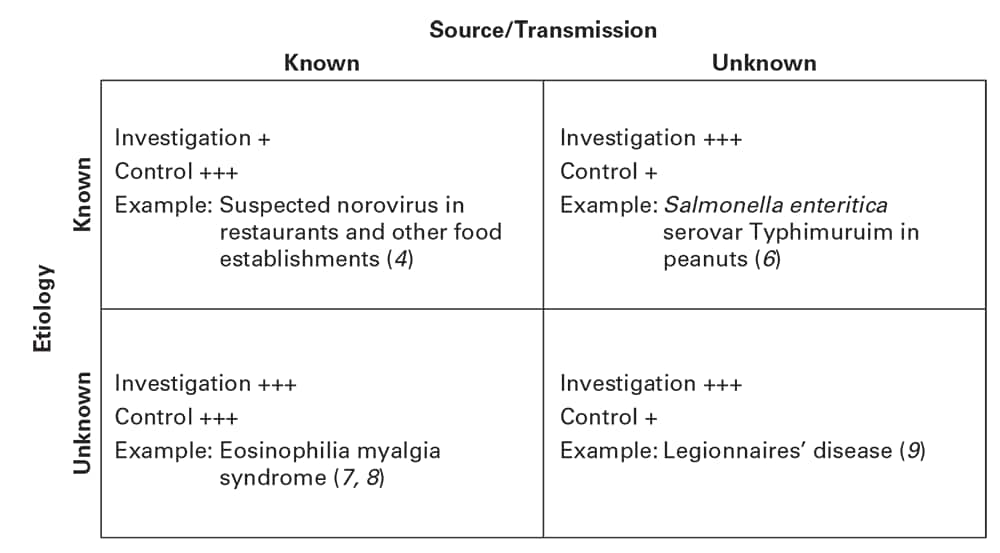
Relative emphasis of investigative and control efforts (intervention options) in disease outbreaks as influenced by levels of certainty about etiology and source or mode of transmission. Investigation means extent of the investigation; control means the basis for rapid implementation of control or intervention measures at the time the problem is initially identified. Plus signs indicate the level of response indicated, ranging from + (low) to +++ (high).
For example, a suspected norovirus outbreak associated with a restaurant or food preparation establishment might warrant a spectrum of interventions, including
- Promptly excluding food service employees symptomatic with vomiting or diarrhea;
- Temporarily closing the restaurant;
- Replacing all food items;
- Sanitizing all surfaces and equipment;
- Monitoring food-handling practices until more specific information is available from the epidemiologic investigation;
- Educating food handlers about norovirus containment; and
- Providing training and education about health codes for restaurant owners (4).
In such an instance, the response will be based on knowledge of possible continuing sources of norovirus or some other enteric pathogen, exposure in a restaurant, and removal of those sources. Although this sort of prompt and appropriate response addresses the possibility of continued transmission on the basis of known agent-specific facts and experience, epidemiologists sometimes need to extend the investigation, depending on the circumstances and needs (e.g., when a trace-back is indicated to identify a continuing primary source for a restaurant-associated outbreak, such as shellfish or lettuce that was contaminated before being harvested) (5).
More commonly, a degree of uncertainty exists about the etiology or sources and the mode of spread (Figure 11.1). For most gastrointestinal outbreaks, selecting control measures depends on knowing whether transmission has resulted from person-to-person, foodborne, or waterborne spread and, if either of the two latter modes, on identifying the source. For example, an outbreak of Salmonella enterica serovar Typhimurium across multiple states during 2008 required extensive multipronged epidemiologic field investigations and analytic (case– control) studies before peanut butter and peanut butter–containing products were identified as the transmission vehicles (6). The converse situation—involving a presumed source but unknown etiology—is illustrated by the nationwide outbreak of eosinophilia myalgia syndrome in the United States in 1989 (7,8). During that outbreak, L-tryptophan, a nonprescription dietary supplement, initially was implicated as the source of the exposure, and contaminants in specific brands were eventually implicated through laboratory analysis. In the interim, epidemiologists issued recommendations preventing further exposures and cases. Finally, as illustrated by the Legionnaires’ disease outbreak in 1976, an extensive field investigation can fail to identify the cause, the source, and mode of spread in time to control the acute problem but still can enable advances in knowledge that ultimately lead to preventive measures (9).
Causation and the Field Investigation
In his seminal article on criteria for assessing causal associations in epidemiology, Austin Bradford Hill concluded with a call for basing action on weighing the strength of the epidemiologic evidence against the severity of the consequences of delaying action and of taking premature action (1). These same concerns commonly confront epidemiologists during field investigations. The criteria specified by Hill—temporality, strength of association, biologic gradient, consistency, plausibility, coherence, experiment, and analogy—provide a useful framework for assessing the strength of epidemiologic evidence developed during a field investigation. Assessing causality at each step in an investigation is important not only for assessing the strength of evidence developed up to that point, but also in helping to identify what evidence is missing or requires further attention and for planning additional approaches (e.g., data gathering and analysis) essential for supporting decisions regarding interventions.
Such criteria as strength of association, dose-response, and temporality can increase confidence in initiating actions. Moreover, at any step in the investigation, evidence that satisfies a specific criterion might be unavailable. Nonetheless, field investigators should try to collect data for examining causality by using as many criteria as is feasible. Although a single criterion might not be convincing in a given context or fully accepted on the basis of the interpreter’s viewpoint, a combination of well-assessed criteria pointing to a common exposure can strengthen confidence and facilitate support for directed interventions.
Epidemiology, in particular field epidemiology, is a relatively young scientific discipline in the medical world, acquiring academic, and then public, acceptance only gradually over the past five to six decades. Among certain sectors—for example, the legal profession, private enterprise, and even regulatory agencies—acceptance of epidemiologic conclusions has been slower, in part because of the nature of causation in epidemiology: epidemiologic evidence establishes associations, not hard, irrefutable proof. Meanwhile, epidemiologic evidence often is the first basis for implicating a causative agent or mode of spread before the results of more in-depth and lengthier scientific investigations become available to support decision-making about interventions. Moreover, and lamentably, epidemiologic evidence that compels epidemiologists to take prompt action might not readily convince others whose cooperation is necessary for initiating action. For example, years elapsed after field studies had clearly implicated antecedent aspirin use as a risk factor for Reye syndrome (10) before industry and the Food and Drug Administration accepted the association and issued warnings to that effect. The story of toxic shock syndrome further illustrates the reluctance of some to accept epidemiologic evidence in the face of an acute public health problem on the scale of a nationwide epidemic (11). These examples underscore the practical challenges in balancing the need to assess causality through the process of scientific inquiry with the potentially conflicting need to intervene quickly to protect the public’s health.
During any outbreak, multiple groups of persons might be exposed, affected, or involved in some respect. Because of differences in knowledge, beliefs, and perceived impact of the outbreak, each group might draw different conclusions about causality from the same information. For example, in a suspected restaurant-associated foodborne illness outbreak, restaurant patrons, the public, owners and management, media, attorneys, and public health officials are each likely to have a different threshold for judging the degree of association between eating food from the restaurant and illness. In this situation, the public health field epidemiologist’s concerns might focus especially on the criteria of strength of association and dose-response effect between exposure to a certain food item and illness, whereas a restaurant patron’s primary concern is simply plausibility. In contrast, attorneys—who either are representing plaintiff-patrons who putatively acquired their illnesses as a result of restaurant exposure or are defending a restaurant epidemiologically associated with a foodborne illness epidemic—will approach such a problem by using a legal framework for causation, which varies from epidemiologic causation (12). In civil cases, the plaintiff’s attorney in particular must meet a preponderance-of-evidence standard of proof, which means that the factfinder (i.e., the judge or jury) must believe that the plaintiff’s version of events is more probable than not for the plaintiff to prevail (13); this standard also has been analogized to a probability of 0.51 or greater (14).
Sociopolitical Context
Field investigations often occur in the public limelight, whether intentionally or not. When a problem is perceived as severe (e.g., a death has occurred) and possibly ongoing, the public might demand information and action. In addition, when interest is intense among politicians, including executive branch leaders (e.g., governors and mayors), such leaders might wish to be visible and demonstrate their interest in protecting the public. For example, a schoolchild’s death from meningitis might lead to political pressure to close the school. A hospital patient’s death from Legionnaires’ disease might lead to political pressure to consider closing the hospital.
As part of the deliberation about when and how to intervene, effective and continuous communication with all concerned entities is essential. These entities need to be aware of the possibilities, the ongoing risks (if any), and how best to address them given the level of information available. An essential component of any intervention is effective communication with political leaders and the public. Such communication will assist in enabling use of scientific factors as the determinants for selecting the intervention(s) to protect the public against disease and should help minimize the potential for unnecessary, costly, and misleading interventions. Nonetheless, the evidence-based perspective might not be the only one eventually considered in the choice of interventions. During the 2014–2015 Ebola virus disease epidemic in parts of West Africa, many US jurisdictions, often for political reasons, implemented strict quarantine and health monitoring for persons who had traveled to an affected country, despite these persons having no history of exposure to anyone with Ebola virus infection (15).
Interventions for preventing and controlling public health problems—including infectious disease outbreaks and noninfectious diseases, injuries, and disabilities—can be approached through different classification schemes. Examples of these approaches include
- Interventions targeting specific aspects of the relation between the host, environment, and disease-or injury-causing agent;
- Primary, secondary, and tertiary prevention options; and
- Haddon’s injury prevention model, which keys on intervention strategies at the preevent, event, and postevent phases (16–18).
In addition to the specific nature of the etiologic agent, decision-makers might need to consider other factors, including
- The agent’s reservoir or source;
- The mode of spread or transmission;
- Host-related risk factors;
- Environmental and other mediating factors;
- A priori evidence of effectiveness of the intervention;
- Operational and logistical feasibility; and
- Legal authority necessary to support implementing the measure.
In this chapter, the model used to systematically identify and characterize the spectrum of intervention options for outbreaks and other acute health threats focuses on two basic biologic and environmental dimensions: (1) interventions that can be directed at the source(s) of most infectious and other disease-causing agents and (2) interventions that can be directed at persons susceptible to such agents (Box 11.2). The first category—interventions directed at the source—includes measures that would eliminate the disease-causing agent’s presence as a risk factor for susceptible populations (e.g., seizing and destroying contaminated foods or temporarily barring an infected person from preparing or serving food). Both categories encompass some of the same options and thus are not completely mutually exclusive. For example, during the 2016–2017 Zika virus infection outbreak, men returning from travel to epidemic areas were advised to use condoms when having sex with susceptible pregnant or potentially pregnant women, as well as for pregnant or potentially pregnant susceptible women to use condoms with any male partner who might have been exposed to the virus to decrease the women’s risk for exposure (19).
During the Ebola virus disease epidemic in 2014–2015, public health officials in the United States used a combination of intervention measures directed at persons in whom Ebola virus disease was diagnosed (isolation), at their close contacts (active monitoring, quarantine, or restrictions on travel), at those providing healthcare to them (training in correct use of special protective gear and active monitoring), and at those arriving from selected countries (screening or active monitoring) (20).
Selection from measures listed in Box 11.2 and other alternatives might be considered at any stage of a field investigation. During early stages, interventions based on established guidelines for disease control can be applied. For example, as indicated earlier in this chapter, excluding symptomatic employees and removing all possible existing sources of an enteric pathogen such as norovirus from a food preparation facility can be done regardless of the actual source of the outbreak (4). If, at a subsequent point, the nature of the risk for infection is more sharply defined, then additional, tailored corrective measures can be directed at the source and/or mode of spread.
These interventions are grouped according to those that can be directed at the source(s) of most infectious and other disease-causing agents and those that can be directed at persons susceptible to such agents.
Interventions Directed at the Source
- Treat infected or affected persons and animals.
- Isolate infected persons, including cohorting, if needed.
- Use barrier methods (e.g., face masks, condoms).
- Monitor exposed persons for signs of illness.
- Quarantine contaminated sites or sources.
- Implement cordon sanitaire, close public places, and prevent gatherings to freeze or limit movement and minimize likelihood of mixing groups by exposure or infection status.
- Use contact tracing, partner notification, and treatment.
- Seize or destroy contaminated food, property, animals, or other sources.
- Clean and disinfect contaminated surfaces and other environmental repositories.
- Modify the affected environment through vector control.
- Modify the affected environment by restricting or controlling dangerous drugs or contaminants.
- Modify behavior to reduce risks to self or others.
- Deter through civil suits or criminal prosecution.
Interventions Directed at Susceptible Persons or Animals
- Administer postexposure prophylaxis.
- Immunize or vaccinate in advance.
- Exclude unvaccinated persons from cohorts of vaccinated persons.
- Use barrier methods (e.g., face masks, condoms).
- Implement cordon sanitaire, close public places, and prevent gatherings to freeze or limit movement and minimize likelihood of mixing groups by exposure or infection status.
- Modify behavior to reduce risks to self or others.
- Use shelter-in-place (i.e., reverse quarantine).
- Issue press releases, health alerts, and other information about risk reduction.
Although this chapter has explored a science-based foundation for identifying, selecting, and implementing public health interventions, field investigators also must contend with a spectrum of new and evolving concerns that challenge decision-making about interventions. This section briefly addresses three such concerns.
- The dilemma public health officials face in selecting and implementing interventions when science-based information might be limited regarding their appropriateness or effectiveness. For certain infectious diseases and other public health problems, recent efforts to plan for selecting and using different interventions have encountered controversy or other challenges because of limitations in the availability of science-based information about their benefits versus their societal costs. For example, during deliberations about what measures might be most effective for responding to an influenza A(H5N1) pandemic, many persons have questioned whether sufficient science-based evidence exists to support widespread use of some relatively draconian social distancing measures (21).
- The paramount importance of increasing an affected community’s understanding of the nature of the public health problem and the rationale for the recommended intervention(s). An influential trend in selecting and implementing interventions is the increasing role of community involvement. For example, for the past several decades, public health agencies have had to innovatively modify their responses to such problems as outbreaks of multidrug-resistant tuberculosis, clusters of cases of human immunodeficiency virus infection, resurgent and antibiotic-resistant sexually transmitted diseases, and meningococcal disease among men who have sex with men (22–25). For some public health problems, traditional methods for investigation and contact evaluation have been supplanted by newer social network approaches—interventions that require increased involvement of community representatives. In such settings, community support is essential for the success of the investigation and longer term prevention and control measures; conversely, failure to obtain community trust and support can disable or constrain the impact of an investigation. This can be especially true when problems disproportionately affect groups who are marginalized and who otherwise might be initially reluctant to work with public health officials. The need for obtaining community trust also implicates the important role of health and risk communications, as well as the importance of explaining to the community both the rationale for and potential limitations of an intervention (e.g., why the intervention might not work or be 100% effective). Community representatives can also help disseminate information to persons most at risk through blogs, social media, mobile phone applications, or other nontraditional communication channels. The increasing role of community involvement in and support for public health interventions applies not only to infectious diseases but also to preventing and controlling environmental hazards, including substance abuse, injuries, and other noninfectious disease problems.
- The sometimes complex nature of making a decision about when to terminate an acute intervention or how to institutionalize or to sustain it for a longer period. This final challenge encompasses the need to assess the effectiveness of each intervention and make decisions about whether and when to terminate or sustain it. At the earliest possible moment, data being generated by the epidemiologic investigation should be used to assess the effectiveness of each intervention. Such information also guides decision-making regarding modification or termination of already implemented interventions and selection and use of additional or new measures. A decision to leave an intervention in place long term or permanently might be made in situations where the public health risk cannot be eliminated and remains an ongoing threat (e.g., ban on use of lead-based paint or sustaining a recommendation to vaccinate men who have sex with men against meningococcal disease after an outbreak is over because of sustained higher risk [25]).
Epidemiologic field investigations usually are initiated in response to epidemics or the occurrence of other acute disease, injury, or environmental health problems. Under such circumstances, the primary objective of the field investigation is to use the scientific principles of epidemiology to determine a rational and appropriate response for ending or controlling the problem. Key factors that influence decisions about the timing and choice of public health interventions include a carefully crafted balance among
- The severity of the problem,
- The levels of scientific certainty of the findings,
- The extent to which causal criteria have been established,
- The intervention’s operational and logistical feasibility,
- The public and political perceptions of what is the best course of action, and
- Legal considerations.
This chapter has examined essential factors epidemiologists and other public health officials must consider when making decisions about selecting and implementing public health interventions during epidemiologic field investigations. Taking these factors into account, the following actions should be reconsidered at each progressive stage of the field investigation:
- Define the scope of the public health problem with available information by assessing
- The severity of the illness, injury, or environmental hazard;
- The nature of the suspected etiologic agent;
- The number of possible susceptible persons and the extent of their exposure; and
- Possible reasons for the outbreak.
- Determine whether possible reasons for the outbreak might be ongoing, and, for all potentially ongoing reasons and exposures for which intervention(s) might be offered, consider what empiric interventions can be used to reduce or eliminate any ongoing risk for exposure or illness.
- For each potential intervention, consider the costs and benefits of implementing the intervention at that stage of the investigation in the absence of additional information.
- Implement all reasonable empiric interventions.
- Communicate the rationale for implementing or not implementing interventions at any point to persons within the community who have been exposed or affected, as well as others who might need to know.
- Continuously assess the effectiveness of and modify the interventions as new investigation information becomes available.
Adherence to these and other steps during epidemiologic field investigations can be integral to helping attain and optimize a scientifically rational basis for selecting and implementing public health interventions for controlling or terminating a problem.
Note
Portions of this chapter as incorporated within previous editions of this book were adapted from Goodman RA, Buehler JW, Koplan JP. The epidemiologic field investigation: science and judgment in public health practice. Am J Epidemiol. 1990;132:91–96.
Acknowledgments
We acknowledge James W. Buehler and Jeffrey P. Koplan, whose work on Chapter 9, “Developing Interventions,” in the first and second editions of this manual contributed in part to this chapter.
- Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300.
- Gaynes R, Richards C, Edwards J, et al. Feeding back surveillance data to prevent hospital-acquired infections. Emerg Infect Dis. 2001;7:295–8.
- Goodman RA, Buehler JW, Koplan JP. The epidemiologic field investigation: science and judgment in public health practice. Am J Epidemiol. 1990;132:91–6.
- Centers for Disease Control and Prevention. Vital signs: foodborne norovirus outbreaks—United States, 2009–2012. MMWR. 2014;63:491–5.
- Dowell SF, Groves C, Kirkland KB, et al. A multistate outbreak of oyster-associated gastroenteritis: implications for interstate tracing of contaminated shellfish. J Infect Dis. 1995;171:1497–503.
- Centers for Disease Control and Prevention. Multistate outbreak of Salmonella infections associated with peanut butter and peanut butter– containing products—United States, 2008–2009. MMWR. 2009;58:85–90.
- Centers for Disease Control and Prevention. Eosinophilia-myalgia syndrome—New Mexico. MMWR. 1989;38:765–7.
- Centers for Disease Control and Prevention. Eosinophilia-myalgia syndrome and L-tryptophan-containing products—New Mexico, Minnesota, Oregon, and New York, 1989. MMWR. 1989;38:785–8.
- Fraser DW, Tsai TR, Orenstein W, et al. Legionnaires’ disease: description of an epidemic of pneumonia. N Engl J Med. 1977;297:1189–97.
- Hurwitz ES, Schonberger LB. Reye syndrome—Ohio, Michigan. MMWR. 1997;46:750–5.
- Osterholm MT, Davis JP, Gibson RW, et al. Tri-state toxic-shock syndrome study. I. Epidemiologic findings. J Infect Dis. 1982;145:431–40.
- Goodman RA, Loue S, Shaw FE. Law in epidemiology. In: Bownson R, Petiti D, eds. Applied epidemiology. 2nd ed. New York: Oxford University Press; 2006:289–326.
- Freer RD, Perdue WC, eds. Civil procedure: cases, materials, and questions. 2nd ed. Cincinnati, OH: Anderson Publishing Co.; 1997.
- Lazzarini Z, Goodman RA, Dammers K. Criminal law and public health practice. In: Goodman RA, Hoffman RE, Lopez W, Matthews GW, Rothstein MA, Foster KL, eds. Law in public health practice. 2nd ed. New York: Oxford University Press; 2007:136–67.
- American Civil Liberties Union and Yale Global Health Justice Partnership. Fear, politics, and Ebola: how quarantines hurt the fight against Ebola and violate the Constitution. https://www.law.yale.edu/system/files/documents/pdf/Intellectual_Life/aclu_yale_ghjp_-_fear_politics_and_ebola-december_2015.pdf
- Wenzel RP. Overview: control of communicable diseases. In: Wallace RB, Kohatsu N, Brownson R, Schecter AJ, Scutchfield FD, eds. Maxcy-Rosenau-Last public health & preventive medicine. 15th ed. New York: McGraw-Hill Education; 2008:77– 100.
- Kim-Farley RJ. Global strategies for control of communicable diseases. In: Detels R, McEwen J, Beaglehole R, Tanaka H, eds. Oxford textbook of public health. 4th ed. New York: Oxford University Press; 2002:839–59.
- Olsen J. Disease prevention and control of non-communicable diseases. In: Detels R, McEwen J, Beaglehole R, Tanaka H, eds. Oxford textbook of public health. 4th ed. New York: Oxford University Press; 2002:1811–22.
- Oster AM, Russell K, Stryker JE, et al. Update: interim guidance for prevention of sexual transmission of Zika virus—United States, 2016. MMWR. 2016;65:323–5.
- Centers for Disease Control and Prevention. Interim U.S. guidance for monitoring and movement of persons with potential Ebola virus exposure. http://www.cdc.gov/vhf/ebola/exposure/monitoring-and-movement-of-persons-with-exposure.html
- Ferguson NM, Cummings DAT, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006;442:448–52.
- Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men—southern California, 2000. MMWR. 2001;50:117–20.
- Centers for Disease Control and Prevention. HIV-related tuberculosis in a transgender network—Baltimore, Maryland, and New York City area, 1998–2000. MMWR. 2000;49:317–20.
- Conrad C, Bradley HM, Boiz D, et al. Community outbreak of HIV infection linked to injection drug use of oxymorphone—Indiana, 2015. MMWR. 2015;64:443–4.
- Kratz MM, Weiss D, Ridpath A, et al. Community-based outbreak of Neisseria meningitidis serogroup C infection in men who have sex with men, New York City, New York, USA, 2010–2013. Emerg Infect Dis. 2015;21:1379–86.