What to know
CDC estimates approximately 20 million new sexually transmitted infections (STIs) infections occur in the United States each year, costing nearly $16 billion. More than 110 million total (new and existing) people are infected with an STI at any given time. Increasingly, certain STIs are becoming resistant to the antimicrobials used to treat them. AMD technology advances the understanding of STIs and improves surveillance for antimicrobial resistance markers in pathogen DNA. The technology could inform vaccine development and potentially change the diagnosis and treatment paradigm into customized treatment for individual patients.

Detecting infections sooner
In a report from 2021, CDC estimates that 1.2 million people in the United States are living with HIV. Of those people, about 13%, or 1 in 8, did not know they were infected. There have been great strides in preventing and treating HIV. Unfortunately, the disease remains a persistent problem in the United States and globally.
Early detection is key in preventing spread of HIV. CDC scientists are using AMD methods to improve diagnostic tests. The purpose is to catch infections weeks earlier than previous testing methods. In addition, scientists use AMD bioinformatics capabilities to develop new computer software tools. Those tools have the ability to identify transmission networks for HIV and other diseases.
Tracking disease transmission
To stop STI or HIV outbreaks, public health agencies conduct surveillance to discern the most likely clusters of people involved. The surveillance helps target interventions where those efforts will make the most impact. With AMD technologies, traditional epidemiology is combined with genomic data to identify transmission clusters.
CDC investigators used AMD bioinformatics capabilities to develop a browser-based data integration, analysis, and visualization tool called MicrobeTrace. The tool, used to identify transmission networks for HIV and other pathogens, is free, intuitive, flexible, secure and pathogen agnostic. The tool merges large amounts of epidemiologic, genomic sequence, and clinical data. Those data merges provide visual representations of transmission networks, including spatial and temporal views. That information makes it easy to pinpoint clusters of recent transmission and to better focus treatment and prevention efforts.
The paper detailing MicrobeTrace development was published in 2021. In two years, the user base increased from ~390 in 2018 to more than 11,300 users globally as of April 2023. The broader use of this tool ensures benefits at the state and local levels.
Investigators leverage MicrobeTrace to assist with outbreaks involving other pathogens, including tuberculosis, hepatitis, gonorrhea, syphilis, and SARS-CoV-2. To align with the data modernization initiative, the software code has been modernized. Currently, plans are underway to develop a cloud-based version to increase functionality and access.
Did you know?
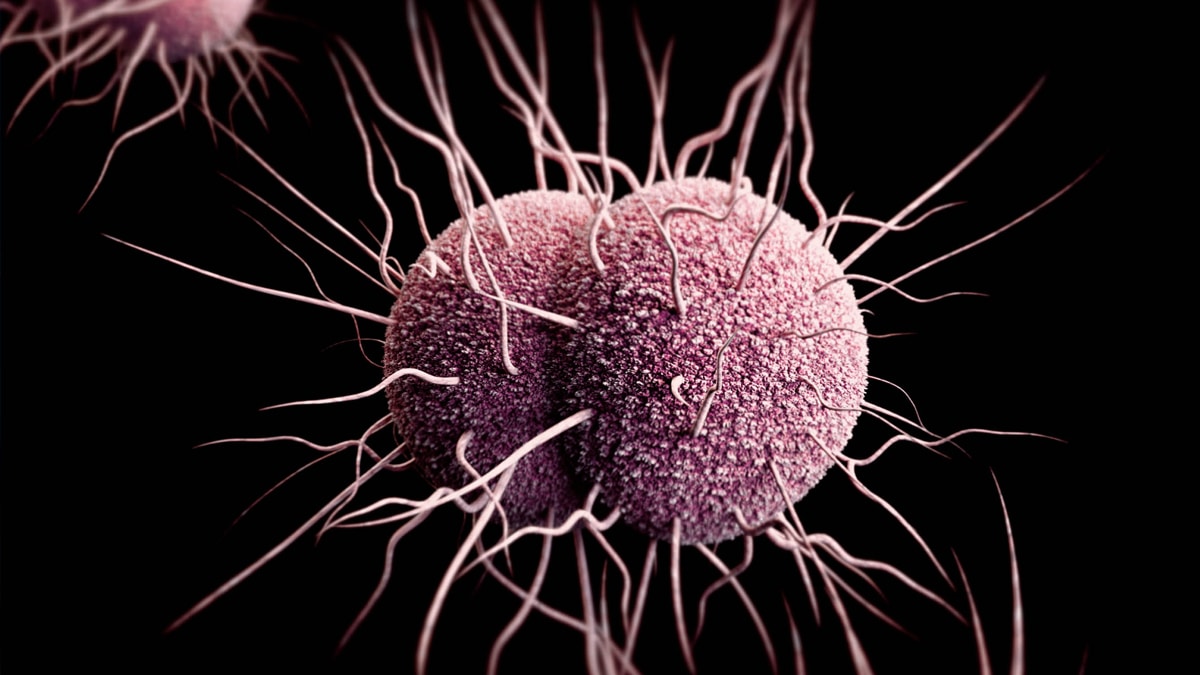
Identifying antibiotic-resistant gonorrhea
Gonorrhea is increasingly resistant to the drugs prescribed to treat it. Few antibiotic options remain. Scientists are working to unlock the potential to develop new drugs to treat gonorrhea. They also are working to develop better tests to determine whether a patient has a resistant infection.
Before antibiotics, gonorrhea could lead to lifelong, severe illnesses. These include blindness in newborns, infertility in women, and scarring of the urinary tract in men. With effective antibiotics, people are cured of gonorrhea with a single dose. Despite those treatments, over the past few decades, public health agencies have seen a growing number of drug-resistant gonorrhea strains.
To fight this urgent public health threat, CDC is using the latest advances in genome sequencing techniques. Those AMD technologies unlock the DNA of the bacterium responsible for gonorrhea and pinpoint the genes that cause antibiotic resistance. Scientists hope this innovative research will help scientists find more effective ways to prevent gonorrhea. The underlying goal is to keep untreatable gonorrhea from becoming a reality.
Investigating emerging meningococcal disease
In 2015, public health researchers found multiple cases of urethritis caused by Neisseria meningitidis, the bacteria that causes meningococcal disease. Urethritis, a swelling and irritation of the urethra (the tube that carries urine from the bladder), is typically associated with STIs like gonorrhea. Researchers are investigating how common meningococcal urethritis is and are using AMD methods to investigate what causes it and how it spreads. Researchers are also studying bloodstream infections and meningitis caused by N. meningitidis to determine whether any belong to the group of N. meningitidis causing urethritis. This work is helping guide practices to control this disease and prevent it from spreading further.
Tracing the specter of hepatitis C
Hepatitis C is a contagious liver disease that can cause lifelong illness. People are infected with the hepatitis C virus (HCV) primarily through contact with the blood of an infected person. This infection can be spread by sharing needles or other equipment to inject drugs, as well as other methods.
Genomic data acquired through AMD methods combined with epidemiologic information help researchers identify HCV transmission clusters. Identifying the clusters greatly improves capacity for rapid and effective response.
Global Health Outbreak and Surveillance Technology (GHOST) is a web-based system that performs a comprehensive analysis of genomic and epidemiologic data. Once a user inputs unique genomic data from an HCV sample, GHOST identifies transmission links between other virus samples. Then the system automatically creates a simple graph that shows plainly which cases are linked by transmission. This testing can help identify transmission linkages, however determining the source of infection or direction of transmission must be accomplished through other components of an epidemiologic investigation.
The technology also reduces the cost of molecular testing, making it more affordable to many more laboratories. In addition, CDC is expanding this modern molecular surveillance tool for other infectious diseases. The goal is to help establish a platform for effective collaboration and communication across the public health system.
- "GHOST: global hepatitis outbreak and surveillance technology," Longmire, Atkinson G., et al., BMC Genomics (2017)
- Automated quality control for a molecular surveillance system. Sims, Seth, et. al., BMC Bioinformatics (2018)
- A large HCV transmission network enabled a fast-growing HIV outbreak in rural Indiana, 2015. Ramachandran, Sumathi, et.all., eBioMedicine (2018)
- HCV transmission in high-risk communities in Bulgaria. Ganova-Raeva Lilia, et. al., PLoS One (2019)
- Hepatitis C virus transmission cluster among injection drug users in Pakistan. Sahibzada, Kashif Iqbal, et. al., PLoS One (2022)
