Using Telehealth to Decrease Carbapenem Use in a Critical Access Hospital
Key Take Away Points
- Tracking antimicrobial use over time in a hospital and comparing its use with other facilities helps identify targets for antimicrobial stewardship and interventions to improve prescribing.
- Data sharing with prescribers and other stakeholders can drive behavioral changes.
- An active prospective audit and feedback approach is an effective and efficient strategy in critical access hospitals.
Critical access hospital within the Intermountain Healthcare system.
This hospital has less than 20 beds and is located in rural Utah. The antimicrobial stewardship program is locally run with the support of Infectious Diseases (ID) Telehealth physicians and an ID Telehealth pharmacist.
The Need
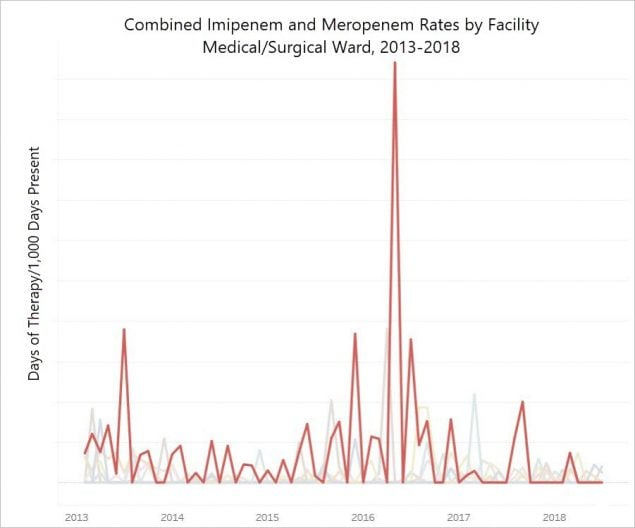
A facility submitted data into the CDC’s National Healthcare Safety Network (NHSN) Antimicrobial Use (AU) Option from 2013-2018. At this facility, imipenem and meropenem days of therapy per 1,000 days present were identified as an outlier compared to eight other small community hospitals within Intermountain’s system, six of which are critical access. The figure shows combined meropenem and imipenem rates from 2013 through 2018. The red line represents the single medical/surgical ward at the outlier facility while the grey lines represent the medical/surgical wards of the other eight comparator facilities.
The Intervention
The ID Telehealth Pharmacist and ID Telehealth Physician presented the NHSN AU Option rate data at the hospital’s antimicrobial stewardship meeting to the local physician and pharmacist champion in January 2017. Empiric therapy was noted as a primary driver of high carbapenem usage. The antibiogram was shared with prescribers to educate them on local resistance patterns and to help guide their prescribing of empiric antimicrobial therapy. Providers were also informed that the ID Telehealth Pharmacist would be reviewing meropenem orders for appropriateness moving forward. For the 18 months following the intervention (January 2017 – June 2018), the ID Telehealth Pharmacist prospectively reviewed new orders of meropenem and intervened on those that were suboptimal.
The Result
Following the intervention meropenem and imipenem use rates decreased substantially (Figure). These agents, in addition to other broad-spectrum agents predominantly used for hospital-onset/ multi-drug resistant bacteria will continue to be monitored on an ongoing basis.
For more information contact: John Veillette, PharmD, BCPS
ID Telehealth Pharmacist
Intermountain Healthcare
Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.