Recent Trends in Heart Failure-related Mortality: United States, 2000–2014
- Key findings
- The age-adjusted rates for heart failure-related deaths declined from 2000 through 2012 but increased from 2012 through 2014.
- The age-adjusted rate for heart failure-related deaths was higher for the non-Hispanic black population than for the non-Hispanic white and Hispanic populations.
- Heart failure-related death rates declined for all selected age and sex groups from 2000 through 2012 but increased from 2012 through 2014.
- The percentage of heart failure-related deaths occurring in a hospital decreased from 2000 through 2014.
- Non-cardiovascular disease was the underlying cause of death for more than one-third of heart failure-related deaths of adults aged 45 and over in 2014.
- Summary
- Definitions
- Data source and methods
- About the authors
- References
- Suggested citation
NCHS Data Brief No. 231, December 2015
PDF Versionpdf icon (351 KB)
Hanyu Ni, Ph.D.; and Jiaquan Xu, M.D.
Key findings
Data from the National Vital Statistics System, Mortality
- The age-adjusted rate for heart failure-related deaths decreased from 2000 through 2012 but increased from 2012 through 2014.
- The death rate for heart failure was higher for the
non-Hispanic black population than for the non-Hispanic white and Hispanic populations. - The death rate was higher for men than for women in all age groups. The gap in the death rate for adults aged 45–64 and 85 and over increased over time.
- The percentage of heart failure-related deaths that occurred in a hospital decreased from 2000 through 2014.
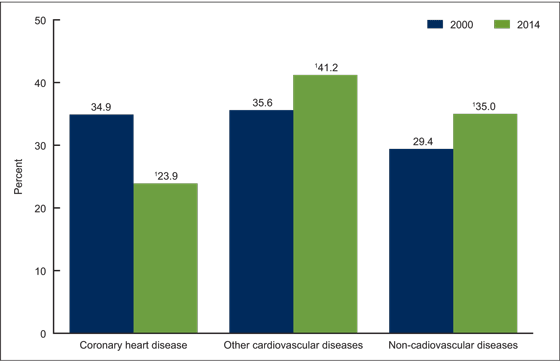
- The percentage of heart failure-related deaths for adults aged 45 and over with coronary heart disease as the underlying cause of death decreased 32%, from 34.9% in 2000 to 23.9% in 2014.
Heart failure is a major public health problem associated with significant hospital admission rates, mortality, and costly health care expenditures, despite advances in the treatment and management of heart failure and heart failure-related risk factors (1–4). Using data from the multiple cause of death files, this report describes the trends in heart failure-related mortality from 2000 through 2014 for the U.S. population, by age, sex, race and Hispanic origin, and place of death. Heart failure-related deaths were identified as those with heart failure reported anywhere on the death certificate, either as an underlying or contributing cause of death. Changes in the underlying causes of heart failure-related deaths are also described in this report.
Keywords: mortality, heart failure, trend, National Vital Statistics System
The age-adjusted rates for heart failure-related deaths declined from 2000 through 2012 but increased from 2012 through 2014.
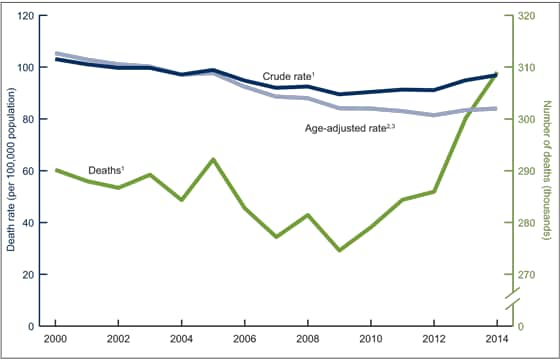
- The crude rate for heart failure-related deaths decreased from 103.1 deaths per 100,000 population in 2000 to 89.5 in 2009. The rate then increased to 96.9 in 2014 (Figure 1).
- The age-adjusted rate for heart failure-related deaths decreased from 105.4 deaths per 100,000 standard population in 2000 to 81.4 in 2012. The rate then increased to 83.4 in 2013 and to 84.0 in 2014.
- The number of heart failure-related deaths declined from 2000 through 2009, but then increased steadily through 2014.
Figure 1. Number of and crude and age-adjusted rates for heart failure-related deaths: United States, 2000–2014
1Declining trends in the number of and crude rates for heart failure-related deaths from 2000 through 2009 were statistically significant (p < 0.05) and their increases from 2009 through 2014 were also significant (p < 0.05).
2Declining trend in the age-adjusted rate for heart failure-related deaths from 2000 through 2012 was statistically significant (p < 0.05).
3Increase in the age-adjusted rate from 2012 through 2014 was significant (p < 0.05).
NOTES: Heart failure-related deaths are those with heart failure (ICD–10 code I50) reported anywhere on the death certificate (i.e., as an underlying or contributing cause of death). Access data table for Figure 1pdf icon.
SOURCE: CDC/NCHS, National Vital Statistics System mortality data, 2000–2014.
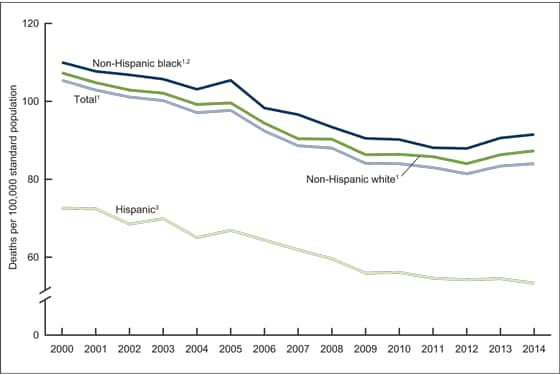
The age-adjusted rate for heart failure-related deaths was higher for the non-Hispanic black population than for the non-Hispanic white and Hispanic populations.
- The age-adjusted rate for heart failure-related deaths was higher for the non-Hispanic black population than for the non-Hispanic white and Hispanic populations from 2000 through 2014 (Figure 2). The death rate was 91.5 deaths per 100,000 standard population for the non-Hispanic black population, 87.3 for the non-Hispanic white population, and 53.3 for the Hispanic population in 2014.
- The age-adjusted death rate decreased 20% for the non-Hispanic black population and 22% for the non-Hispanic white population from 2000 through 2012, and then increased 4% for each population from 2012 through 2014.
- The age-adjusted death rate decreased 27% for the Hispanic population from 2000 through 2014.
Figure 2. Age-adjusted rate for heart failure-related deaths, by race and Hispanic origin: United States, 2000–2014
1Age-adjusted rate of heart failure-related deaths declined significantly from 2000 through 2012 and then increased from 2012 through 2014 for the overall population and for the non-Hispanic white and non-Hispanic black populations (p < 0.05).
2Age-adjusted death rate was significantly higher for the non-Hispanic black population than for the non-Hispanic white and Hispanic populations (p < 0.05).
3Declining trend in the age-adjusted rate of heart failure-related deaths for the Hispanic population from 2000 through 2014 was statistically significant (p < 0.05).
NOTES: Heart failure-related deaths are those with heart failure (ICD–10 code I50) reported anywhere on the death certificate (i.e., as an underlying or contributing cause of death). Access data table for Figure 2pdf icon.
SOURCE: CDC/NCHS, National Vital Statistics System mortality data, 2000–2014.
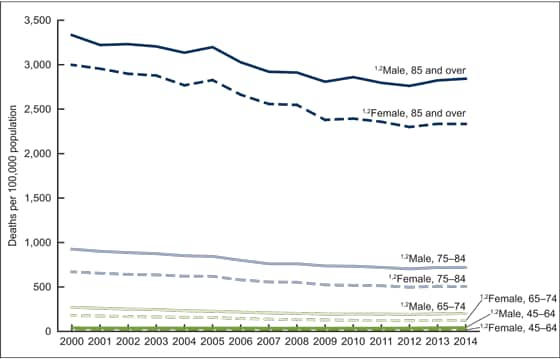
Heart failure-related death rates declined for all selected age and sex groups from 2000 through 2012 but increased from 2012 through 2014.
- Heart failure-related death rates declined from 2000 through 2012 for all age groups (45–64, 65–74, 75–84, and 85 and over) and for both men and women (Figure 3). The death rate increased for all age and sex subgroups from 2012 through 2014.
- The death rate was higher for men than for women in all age and sex subgroups. For adults aged 45–64 and 85 and over, the gap in the death rate between men and women increased over time.
- In 2014, the death rate was highest for adults aged 85 and over (2,842.9 deaths per 100,000 population for men and 2,333.5 for women), followed by adults aged 75–84 (720.0 for men and 504.7 for women), adults aged 65–74 (201.8 for men and 124.6 for women), and adults aged 45–64 (41.3 for men and 24.0 for women).
Figure 3. Death rate for heart failure, by sex and selected age group: United States, 2000–2014
1Declining trends in the heart failure-related death rate from 2000 through 2012, and the increases from 2012 through 2014, were statistically significant for all sex and selected age subgroups (p < 0.05).
2Differences by sex and age group were statistically significant throughout the study period (p < 0.05).
NOTES: Heart failure-related deaths are those with heart failure (ICD–10 code I50) reported anywhere on the death certificate (i.e., as an underlying or contributing cause of death). Access data table for Figure 3pdf icon.
SOURCE: CDC/NCHS, National Vital Statistics System mortality data, 2000–2014.
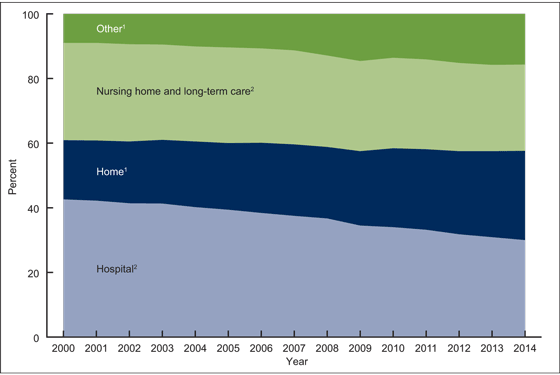
The percentage of heart failure-related deaths occurring in a hospital decreased from 2000 through 2014.
- The percentage of heart failure-related deaths that occurred in a hospital decreased 30%, from 42.6% in 2000 to 30.0% in 2014 (Figure 4).
- The percentage of heart failure-related deaths that occurred at a descendant’s home increased 51%, from 18.3% in 2000 to 27.6% in 2014.
- The percentage of heart failure-related deaths that occurred in nursing homes or long-term care facilities decreased 11%, from 30.1% in 2000 to 26.7% in 2014.
- The percentage of heart failure-related deaths that occurred in other places (such as an outpatient clinic or hospice facility) increased 74%, from 9.0% in 2000 to 15.7% in 2014.
Figure 4. Percent distribution of place of death from heart failure: United States, 2000–2014
1Increases in the percentage of deaths that occurred at home and other places were statistically significant (p < 0.05).
2Percentages of heart failure-related deaths that occurred in a hospital, nursing home, and long-term care facilities declined significantly (p < 0.05).
NOTES: Heart failure-related deaths were identified as those with heart failure (ICD–10 code I50) reported anywhere on the death certificate (i.e., as an underlying or contributing cause of death). Access data table for Figure 4pdf icon.
SOURCE: CDC/NCHS, National Vital Statistics System mortality data, 2000–2014.
Non-cardiovascular disease was the underlying cause of death for more than one-third of heart failure-related deaths of adults aged 45 and over in 2014.
- Coronary heart disease (CHD) was the underlying cause of death for 34.9% of heart failure-related deaths of adults aged 45 and over in 2000. Other cardiovascular diseases accounted for 35.6% and non-cardiovascular diseases for 29.4% (Figure 5).
- CHD was the underlying cause of death for 23.9% of heart failure-related deaths of adults aged 45 and over in 2014. Other cardiovascular diseases accounted for 41.2% and non-cardiovascular diseases for 34.9%.
- The percentage of heart failure-related deaths with CHD as the underlying cause of death decreased 32%, from 34.9% in 2000 to 23.9% in 2014.
Figure 5. Percentage of underlying causes of heart failure-related deaths for adults aged 45 and over: United States, 2000 and 2014
1Differences in the percentage of each underlying cause of death between 2000 and 2014 were statistically significant (p < 0.05).
NOTES: Heart failure-related deaths are those with heart failure (ICD–10 code I50) reported anywhere on the death certificate (i.e., as an underlying or contributing cause of death). Deaths from coronary heart disease (CHD) were identified using underlying cause of death codes (I20–I25). Deaths from other cardiovascular diseases included all deaths from major cardiovascular diseases (I00–I78) after excluding deaths from CHD.
SOURCE: CDC/NCHS, National Vital Statistics System mortality data, 2000–2014.
Summary
This report provides the most recent trends in heart failure-related mortality by age, sex, race and Hispanic origin, and place of death for the U.S. population. The analysis revealed a decline in age-adjusted death rates for heart failure for all selected race and ethnic groups as well as for age and sex subgroups from 2000 through 2012. An increase in the death rate, however, was observed from 2012 through 2014 for the overall population, for selected age and sex groups, and for the non-Hispanic black and non-Hispanic white populations. The age-adjusted rate for heart failure-related deaths was higher for the non-Hispanic black population than for the non-Hispanic white and Hispanic populations from 2000 through 2014.
The underlying cause of heart failure-related deaths for adults aged 45 and over was less likely to be CHD, but more likely to be other cardiovascular diseases and non-cardiovascular diseases (such as cancer, diabetes, chronic lower respiratory diseases, and kidney disease) in 2014 compared with 2000. This shift in the distribution of the causes of death toward less ischemic heart disease is consistent with the results of a community-based study on heart failure (5). This finding is important for heart failure management approaches.
The results of this study also revealed a decrease in the percentage of heart failure-related deaths occurring in hospitals, nursing homes, and other long-term care facilities. An increase was seen in the percentage of deaths at home and in other places. This shift in place of death was observed for heart disease and other causes of death from 1980 through 1998 (6). Place of death is an indicator of the state of end-of-life care, indicating where the patient was receiving care at the very end of life.
Definitions
Cause-of-death classification: Medical information, including injury diagnoses and external causes of injury entered on death certificates filed in the United States, classified and coded in accordance with the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD–10) (7).
Underlying causes of death: Defined by the World Health Organization as “the disease or injury which initiated the train of events leading directly to death, or the circumstances of the accident or violence which produce the fatal injury” (7).
Multiple cause of death: Includes not only the underlying cause but also the immediate cause of death and all other intermediate and contributory conditions reported by the certifying physicians.
Heart failure-related death: All death records with heart failure reported on the death certificate (any mention of heart failure), either as an underlying or a contributing cause. The deaths were identified in the multiple cause of death files as those with ICD–10 code I50 in the record axis fields.
Data source and methods
This report analyzed the multiple cause-of-death mortality files from the National Vital Statistics System from 2000 through 2014. The direct standardization method was used to calculate age-adjusted death rates, based on the projected year 2000 standard population, using age groups with 10-year intervals. Terms such as “higher than” or “lower than” indicate that the estimates being compared are statistically significant. Trends in death rates were evaluated using the Joinpoint Regression Program (8). The comparisons of rates and percentages are based on the two-tailed z test at the 0.05 level.
About the authors
Hanyu Ni and Jiaquan Xu are with CDC’s National Center for Health Statistics, Division of Vital Statistics.
References
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation 127:e6–e245. 2013.
- Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup E, Ezekowitz MD, et al. Forcasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 123(8):933–44. 2011.
- Roger VL. Epidemiology of heart failure. Circ Res 113:646–59. 2013.
- Braunwald E. Heart failure. J Am Coll Cardiol HF;1(1):1–20. 2013.
- Henkel DM, Redfield MM, Weston SA, Gerber Y, Roger VL. Death in heart failure: A community perspective. Circ Heart Fail 1(2):91–7. 2008.
- Flory J, Yinong YX, Gurol I, Levinsky N, Ash A, Emmanuel E. Place of death: U.S. trends since 1980. Health Aff (Millwood) 23(3):194–200. 2004.
- WHO. International statistical classification of diseases and related health problems, tenth revision (ICD–10). 2008 ed. Geneva, Switzerland. 2009.
- National Cancer Institute. Joinpoint Regression Program (Version 4.1.1.) [computer software]. 2014.
Suggested citation
Ni H, Xu JQ. Recent trends in heart failure-related mortality: United States, 2000–2014. NCHS data brief, no 231. Hyattsville, MD: National Center for Health Statistics. 2015.
Copyright information
All material appearing in this report is in the public domain and may be reproduced or copied without permission; citation as to source, however, is appreciated.
National Center for Health Statistics
Charles J. Rothwell, M.S., M.B.A., Director
Nathaniel Schenker, Ph.D., Deputy Director
Jennifer H. Madans, Ph.D., Associate Director for Science
Division of Vital Statistics
Delton Atkinson, M.P.H., M.P.H., P.M.P., Director
Hanyu Ni, Ph.D., M.P.H., Associate Director for Science