Antibiotic Resistance and NARMS Surveillance
Antibiotic resistance is a major global public health threat. Illnesses that were once easily treatable with antibiotics* are becoming more difficult to cure and more expensive to treat. Infections from common antibiotic-resistant bacteria, such as Salmonella, can cause more severe health outcomes than infections with bacteria that are not resistant to antibiotics.
NARMS scientists track and study changes in antibiotic resistance among several bacteria, such as those transmitted commonly through food, water, animal contact, person-to-person contact, and environmental contamination.
NARMS data increase our understanding of
- Resistance trends
- New or emerging resistance
- Bacterial resistance genes
- Which resistant bacteria are making people sick
- Which groups of people are at risk and why
NARMS data are used to help guide efforts to prevent and reduce the spread of resistance and resistant bacteria. Organizations and groups using NARMS data include federal regulatory agencies, policymakers, consumer advocacy groups, health departments, industry, and the public.
*This site uses the term “antibiotics” to refer to antimicrobial agents used to treat bacterial infections in both people and animals.
- What is antibiotic resistance?
- How does antibiotic use in food animals affect people?
- Why is it important to use antibiotics responsibly in food animals?
- What is CDC doing to prevent foodborne infections caused by antibiotic-resistant bacteria?
- What can I do to reduce the chance of infection with resistant bacteria from foods?
What is antibiotic resistance?
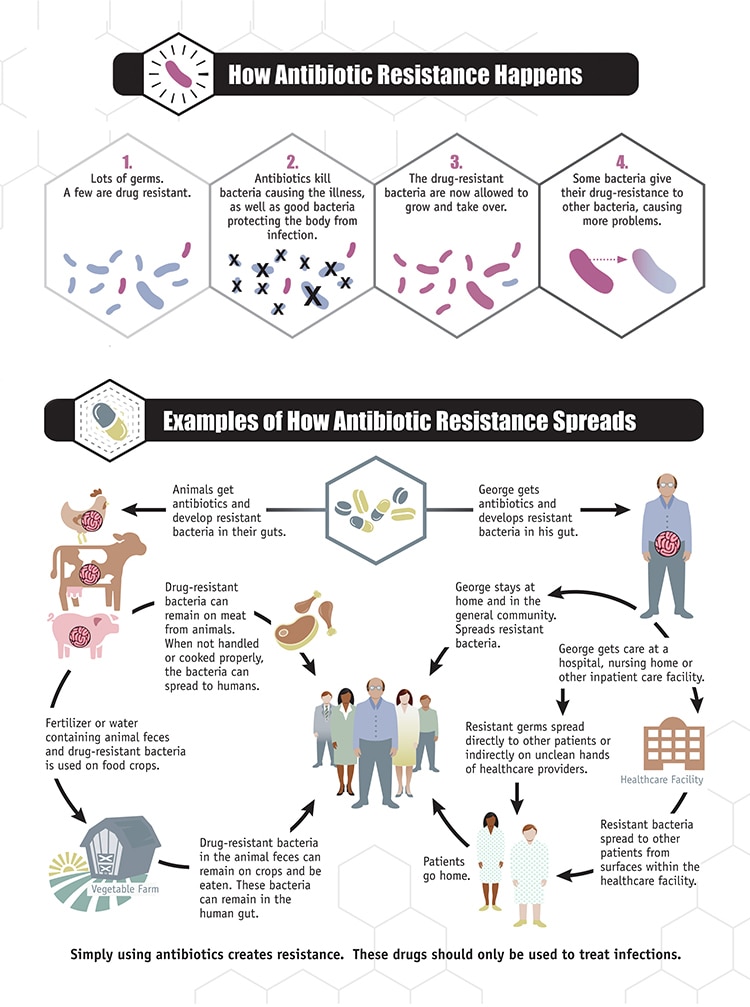
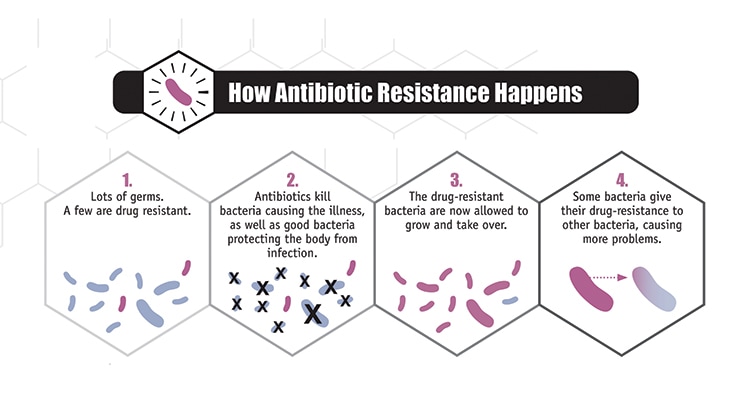
Antibiotic resistance is when bacteria (germs) are able to survive or grow despite the use of an antibiotic that was previously able to stop them.
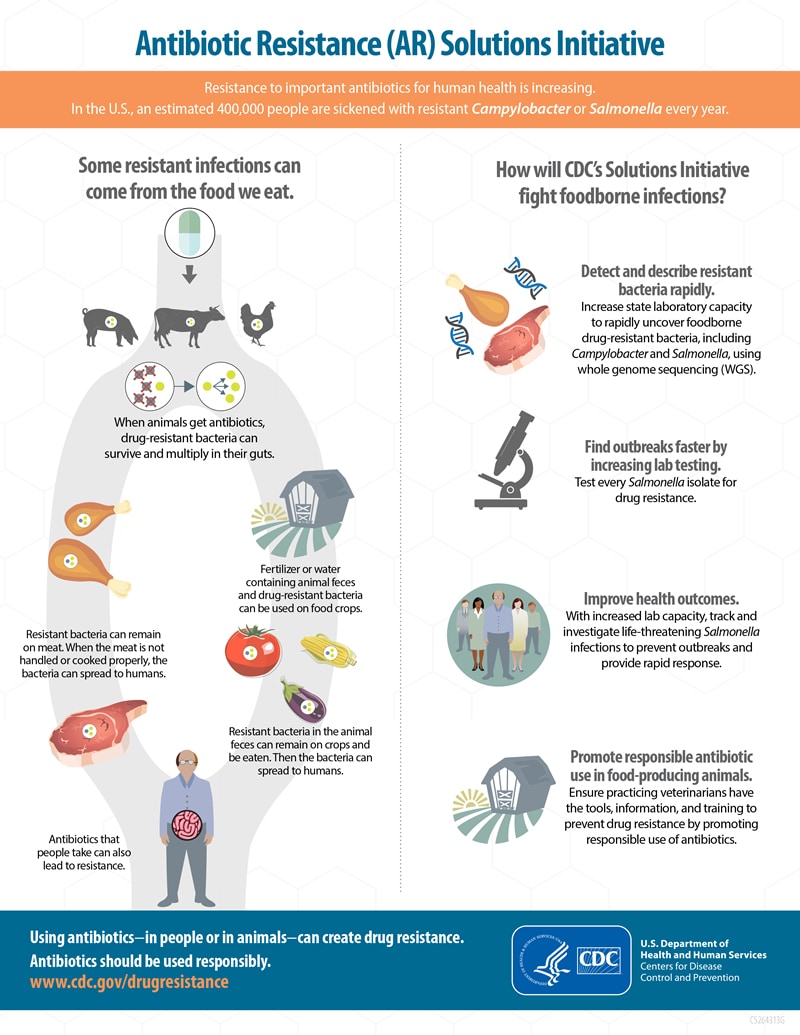
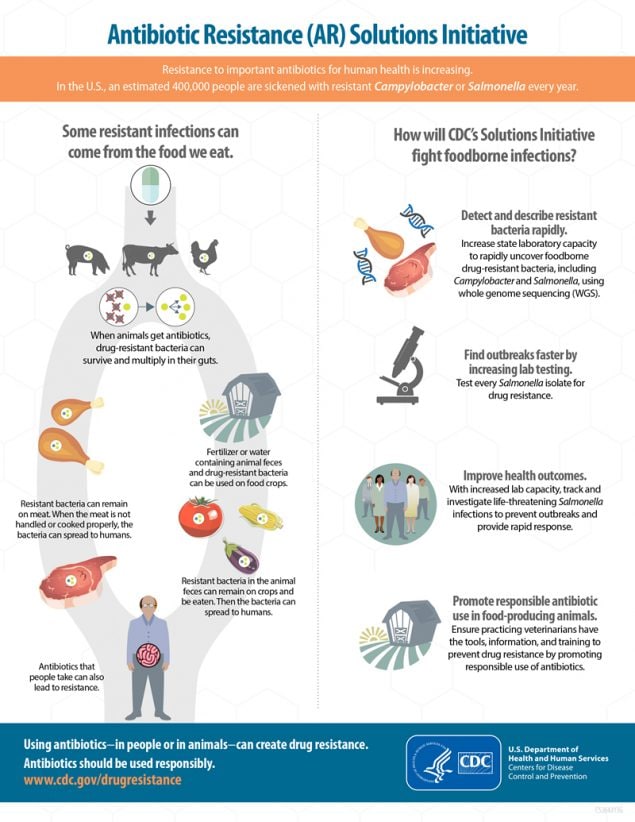
Food animals can carry bacteria, such as Salmonella and Campylobacter, that can make people ill. When animals are given antibiotics, resistant bacteria in their intestines can continue to survive and grow.
What are some ways these bacteria can get into the food supply?
Resistant bacteria that food animals carry can get into a variety of foods. Meat and poultry can become contaminated when the animals are slaughtered and processed. Fruits and vegetables can become contaminated when resistant bacteria from animal feces (poop) spreads to them through the environment, such as through irrigation water or fertilizers.
What are some ways people get infected with resistant bacteria from food animals?
People can get infected with these bacteria in several ways, including
- Handling or eating raw or uncooked meat or poultry
- Coming into contact with food animals or their feces
- Eating raw fruits and vegetables that came into contact with animal feces in the environment, such as through irrigation water or fertilizer
- Consuming water, including recreational water, that came into contact with animal feces
What effects do resistant infections have on people?
Some resistant infections cause severe illness. People with these infections may
- Be more likely to be hospitalized and have higher medical expenses
- Take longer to get well
- Die from the infection

Antibiotics must be used responsibly in both people and animals to help prevent the development, persistence, and spread of resistant bacteria. Antibiotics are valuable tools for reducing animal disease and suffering from bacterial infections, but decisions about which antibiotics to use in food animals and how to use them must also be made with consideration of human health and the environmental impact.
- See the Food and Drug Administration’s (FDA) guidance documents on responsible use of antibiotics in food-producing animals.
- See the World Health Organization’s list of critically important antimicrobials for human medicine.
What are the approved uses for antibiotics in food animals?
FDA has approved antibiotics for these uses in food animals:
- Disease treatment for animals that are sick.
- Disease control for a group of animals when some of the animals are sick.
- Disease prevention for animals that are at risk of becoming sick.

Preventing foodborne and other gastrointestinal illnesses reduces both antibiotic-susceptible and antibiotic-resistant infections. CDC activities that help prevent these infections include:
Tracking Resistance
- Tracking resistance in infections
- Estimating how many antibiotic-resistant infections occur
- Collaborating with domestic and international partners to monitor resistance and improve detection capacities
- Studying how resistance emerges and spreads
Identifying Sources of Infection
- Determining the sources of antibiotic-resistant infections that are commonly spread through food
- Investigating antibiotic-resistant infections to solve and stop outbreaks and improve prevention
- Developing better tools, such as whole genome sequencing, to accurately link cases of foodborne illness to outbreaks and identify sources of food contamination
Improving Food Safety
- Strengthening the ability of state and local health departments to detect, respond to, and report antibiotic-resistant infections
- Educating consumers and food workers about safe food handling and proper handwashing
- Identifying groups with a greater chance of infection and educating them about how to reduce the likelihood of illness
- Promoting the responsible use of antibiotics in animals as well as people
CDC estimates that U.S. doctors’ offices and emergency departments prescribe about 47 million antibiotic courses each year for infections that don’t need antibiotics. That’s about 30% of all antibiotics prescribed in these settings.
Visit CDC’s Be Antibiotics Aware website to learn how improving antibiotic use in hospitals can reduce rates of infection and antibiotic resistance, improve patient outcomes, and save hundreds of thousands of dollars.
You can reduce the chance of getting a resistant bacterial infection by following some easy recommendations for safe food handling and preparation.
- Follow the Clean, Separate, Cook, and Chill guidelines.
- Wash hands, utensils, and kitchen surfaces with soap and water before preparing food, while preparing food, and before eating.
- Use separate chopping boards and keep raw meat, poultry, seafood, and eggs away from food that does not need to be cooked before eating, such as salad.
- Cook meat, poultry, and eggs to a safe minimum internal temperature.
- Don’t drink raw milk.
- Wash your hands after contact with human or animal feces, animals, or animal environments.
- Follow CDC’s Traveler’s Health recommendations for food and water safety when traveling internationally.