Trends in Human Papillomavirus–Associated Cancers — United States, 1999–2015
Weekly / August 24, 2018 / 67(33);918–924
Elizabeth A. Van Dyne, MD1,2; S. Jane Henley, MSPH2; Mona Saraiya, MD2; Cheryll C. Thomas, MSPH2; Lauri E. Markowitz, MD3; Vicki B. Benard, PhD2 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
Human papillomavirus (HPV) can cause some types of cervical, vulvar, vaginal, penile, anal, and oropharyngeal cancers.
What is added by this report?
Oropharyngeal squamous cell carcinoma is now the most common HPV-associated cancer. During 1999–2015 cervical carcinoma incidence rates decreased 1.6% per year, and oropharyngeal SCC incidence rates increased 2.7% per year among men and 0.8% per year among women.
What are the implications for public health practice?
Population-based screening is recommended for only one HPV-associated cancer (cervical) at this time; however, HPV vaccination can prevent infection with the HPV types most strongly associated with cancer. Ongoing surveillance for HPV-associated cancers using high-quality population-based registries is critical to monitor cancer rates and trends.
Human papillomavirus (HPV) is a known cause of cervical cancer, as well as some oropharyngeal, vulvar, vaginal, penile, and anal cancers. To assess trends, characterized by average annual percent change (AAPC), in HPV-associated cancer incidence during 1999–2015, CDC analyzed data from cancer registries covering 97.8% of the U.S. population. A total of 30,115 new cases of HPV-associated cancers were reported in 1999 and 43,371 in 2015. During 1999–2015, cervical cancer rates decreased 1.6% per year; vaginal squamous cell carcinoma (SCC) rates decreased 0.6% per year; oropharyngeal SCC rates increased among both men (2.7%) and women (0.8%); anal SCC rates also increased among both men (2.1%) and women (2.9%); vulvar SCC rates increased (1.3%); and penile SCC rates remained stable. In 2015 oropharyngeal SCC (15,479 cases among men and 3,438 among women) was the most common HPV-associated cancer. Continued surveillance through high-quality cancer registries is important to monitor cancer incidence and trends in these potentially preventable cancers.
HPV causes cervical cancer and some types of oropharyngeal, vulvar, vaginal, penile, and anal cancer; HPV DNA is found in specific tissue types that include carcinomas of the cervix and SCCs of the vulva, vagina, penis, oropharynx, and anus (1,2). The natural history from HPV infection to precancerous lesion to invasive cervical cancer is well established. HPV is the most commonly sexually transmitted infection in the United States and is often acquired soon after initiating sexual activity (3). Studies indicate that approximately 90% of new cervical HPV infections, including types that cause cancer, clear or become undetectable within 2 years, and those that do not clear take decades to progress to invasive cervical cancer.* Less is known about carcinogenic progression of HPV-associated infection at other anatomic sites (2).
CDC analyzed data from population-based cancer registries that participate in the CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results program that met the criteria for high data quality for all years from 1999 to 2015; these data cover approximately 97.8% of the U.S. population.† Invasive cancers are not tested for HPV in most cancer registries; therefore, an HPV-associated cancer was defined as an invasive malignancy in which HPV DNA was frequently found in special studies, including carcinomas of the cervix (i.e., SCC, adenocarcinomas, and other carcinomas) and SCC of the vulva, vagina, penis, oropharynx, and anus (including rectal SCC) (2) and was microscopically confirmed.§ Cases were classified by anatomic site and cell type using the International Classification of Diseases for Oncology, Third Edition. Oropharyngeal SCC included squamous cell cancer types at the base of tongue, pharyngeal tonsils, anterior and posterior tonsillar pillars, glossotonsillar sulci, anterior surface of soft palate and uvula, and lateral and posterior pharyngeal walls. Anal SCC also included rectal SCCs because they are biologically similar and might be misclassified. Age-adjusted incidence rates were calculated per 100,000 persons and standardized to the 2000 U.S. standard population. Trends were measured with AAPC in rates calculated using joinpoint regression.¶ Rates were considered to increase if the AAPC was greater than zero (p<0.05) and to decrease if the AAPC was less than zero (p<0.05); otherwise, rates were considered stable. A maximum of two joinpoints was used. Rates and trends were estimated by sex, age group, race,** ethnicity,†† and region.§§
In the United States, a total of 30,115 new cases of HPV-associated cancer were reported in 1999 and 43,371 in 2015 (Table 1). In 1999, cervical carcinoma (13,125 cases) was the most common HPV-associated cancer: 3,750 more cases of cervical carcinoma than of oropharyngeal SCC were identified. During 1999–2015 cervical carcinoma rates decreased 1.6% per year, and oropharyngeal SCC rates increased 2.7% per year among men and 0.8% per year among women (Figure 1) (Figure 2). In 2015, there were 11,788 reported cases of cervical carcinoma and 18,917 cases of oropharyngeal SCC, including 15,479 (82%) among men and 3,438 (18%) among women.
Rates of oropharyngeal SCC increased among men in all age groups ≥40 years, ranging from 0.8% among men aged 40–49 years to 4.0% among those aged 60–69 years (Table 1). Rates varied by race, with the largest increase occurring among white men (3.3%), and by region, with rates increasing more in the Midwest (3.2%) than in other regions (Table 2).
During 1999–2015 cervical carcinoma rates were stable among women aged 35–39 years and decreased among women aged 20–34 years and aged ≥40 years, decreasing >3% per year among women aged 20–24 years and ≥70 years (Table 1). Cervical carcinoma rates decreased among all racial/ethnic groups, more among Hispanics than among non-Hispanics, and more in the West than in all other regions (Table 2). During 1999–2015 vaginal SCC decreased 0.6% per year.
In contrast, penile SCC rates were stable, and vulvar SCC rates increased 1.3% per year (Table 1) (Figure 2). Specifically, vulvar SCC rates increased during 1999–2015 among women aged 50–69 years, among whites (1.5%), and blacks (1.0%), and in the Northeast (1.5%), Midwestern (1.5%), and Southern (1.3%) regions of the United States.
Anal SCC rates increased among women (2.9% per year) and men (2.1%) during this period. The largest increases in anal SCC rates were among women aged 50–69 years (4.6%–4.8% per year) and men aged 50–59 years (4.0%). Anal SCC rates increased among white women (3.2% per year), black women (2.2%), white men (2.1%), and black men (3.0%). Anal SCC rates increased among both men and women in all regions except among men in the West region; the largest rate increases were among women in the Northeast (4.3% per year) and Midwest (3.6%).
Discussion
HPV-associated cancer rates changed from 1999 to 2015. Rates increased for oropharyngeal SCC, anal SCC and vulvar SCC, decreased for cervical carcinoma and vaginal SCC, and remained stable for penile SCC.
The decline in cervical cancer from 1999 to 2015 represents a continued trend since the 1950s as a result of cancer screening (4). Rates of cervical carcinoma in this report decreased more among Hispanics, American Indian/Alaska Natives, and blacks than other groups; however, incidence rates were still higher among Hispanics and blacks than among whites in 2015. These persistent disparities in incidence suggest that health care delivery needs of some groups are not fully met.
Several factors could contribute to the increase in oropharyngeal and anal cancers including changing sexual behaviors. Unprotected oral sex and receptive anal sex are risk factors for HPV infection (2,5). White men have the highest number of lifetime oral sex partners and report first performing oral sex at a younger age compared with other racial/ethnic groups; these risk factors could be contributing to a higher rate of oropharyngeal SCC among white men than other racial/ethnic groups (6). Although smoking is a risk factor for oropharyngeal cancers, smoking rates have been declining in the United States, and studies have indicated that the increase in oropharyngeal cancer is attributable to HPV (5). In contrast to cervical cancer, there currently is no U.S. Preventive Services Task Force recommended screening for other HPV-associated cancers (7).
The findings in this report are subject to at least two limitations. First, although population-based cancer registries provide a reliable system for counting invasive cancers, registries do not routinely determine the HPV status of cancers. In the United States, HPV DNA has been determined through special studies and found in 91% of cervical, 91% of anal, 75% of vaginal, 70% of oropharyngeal, 69% of vulvar, and 63% of penile cancers (1). Second, reporting of race and ethnicity uses data from medical records, which might be inaccurate in a small proportion of cases. An important strength of this study is the use of high quality population-based surveillance data with 97.8% coverage of the U.S. population, allowing for specific histologic definitions to monitor HPV-associated cancer trends.
Measures to prevent HPV-associated diseases in the United States include both females and males; HPV vaccination was included in the routine immunization program for females in 2006 and for males in 2011. Although it might be too soon for effects on invasive cancers from HPV vaccination in the United States, studies have reported reductions in cervical HPV infection, genital warts, and cervical precancers (8). Most cervical cancers are preventable with both HPV vaccination and regular and timely screening among women aged 21–65 years with follow-up for abnormal test results. Routine HPV vaccination is recommended at age 11 or 12 years; currently, the 9-valent HPV vaccine, which targets oncogenic types attributed to 73% of HPV-associated cancers, is being used in the United States (1,9). Further research to understand the progression from HPV infection to oropharyngeal cancer would be beneficial. Continued surveillance through high-quality registries is important to monitor changes in HPV-associated cancer incidence.
Corresponding author: Mona Saraiya, msaraiya@cdc.gov, 770-488-4293.
1Epidemic Intelligence Service, CDC; 2Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, CDC; 3Division of Viral Diseases, National Center for Immunization and Respiratory Diseases, CDC.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* Manual for the Surveillance of Vaccine-Preventable Diseases, Chapter 5: Human Papillomavirus (HPV). https://www.cdc.gov/vaccines/pubs/surv-manual/chpt05-hpv.html.
† Cancer registries’ incidence data met the following five United States Cancer Statistics criteria: 1) ≤5% of cases ascertained solely on the basis of death certificate; 2) ≤3% of cases missing information on sex; 3) ≤3% of cases missing information on age; 4) ≤5% of cases missing information on race; and 5) ≥97% of registry’s records passed a set of single-field and interfield computerized edits that test the validity and logic of data components. https://gis.cdc.gov/Cancer/USCS/DataViz.html.
§ HPV-associated cancers were defined as cancers at specific anatomic sites with specific cell types in which HPV DNA frequently is found. All cancers were microscopically confirmed. Cervical cancers (ICD-O-3 http://codes.iarc.fr/ [ICD-O-3] site codes C53.0–C53.9) are limited to carcinomas (ICD-O-3 histology codes 8010–8671, 8940–8941). Vaginal (ICD-O-3 site code C52.9), vulvar (ICD-O-3 site codes C51.0–C51.9), penile (ICD-O-3 site codes C60.0–60.9), anal (including rectal SCC; ICD-O-3 site code C20.9, C21.0–C21.9), and oropharyngeal (ICD-O-3 site codes C01.9, C02.4, C02.8, C05.1, C05.2, C09.0, C09.1, C09.8, C09.9, C10.0, C10.1, C10.2, C10.3, C10.4, C10.8, C10.9, C14.0, C14.2 and C14.8) cancer sites are limited to squamous cell carcinomas (ICD-O-3 histology codes 8050–8084, 8120–8131). Anal and rectal SCC were combined into a single category “anal SCC” because a very small subset of rectal cancers (i.e. the SCCs, around 700 per year) are similar to anal SCC.
¶ https://surveillance.cancer.gov/joinpoint/.
** Population estimates incorporate bridged single-race estimates derived from the original multiple-race categories in the 2010 U.S. Census. https://seer.cancer.gov/popdata.
†† https://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
§§ Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, and Wisconsin. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. South: Alabama, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
References
- Saraiya M, Unger ER, Thompson TD, et al. ; HPV Typing of Cancers Workgroup. US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. J Natl Cancer Inst 2015;107:djv086. CrossRef PubMed
- Bouvard V, Baan R, Straif K, et al.; World Health Organization International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens. part b: biological agents. Lancet 2009;10:321–2. CrossRef
- Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis 2013;40:187–93. CrossRef PubMed
- Benard VB, Thomas CC, King J, Massetti GM, Doria-Rose VP, Saraiya M. Vital signs: cervical cancer incidence, mortality, and screening—United States, 2007–2012. MMWR Morb Mortal Wkly Rep 2014;63:1004–9. PubMed
- Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C. Epidemiology of human papillomavirus–positive head and neck squamous cell carcinoma. J Clin Oncol 2015;33:3235–42. CrossRef PubMed
- D’Souza G, McNeel TS, Fakhry C. Understanding personal risk of oropharyngeal cancer: risk-groups for oncogenic oral HPV infection and oropharyngeal cancer. Ann Oncol 2017;28:3065–9. CrossRef PubMed
- United States Preventive Services Task Force. Published recommendations. Rockville, MD: Guide to Community Preventive Service; 2018. https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations.
- Markowitz LE, Gee J, Chesson H, Stokley S. Ten years of human papillomavirus vaccination in the United States. Acad Pediatr 2018;18(2S):S3–10. CrossRef PubMed
- Petrosky E, Bocchini JA Jr, Hariri S, et al. . Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2015;64:300–4. PubMed
Sources: CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results program.
Abbreviations: AAPC = average annual percent change; CI = confidence interval; SCC = squamous cell carcinoma.
* Per 100,000 persons, age-adjusted to the 2000 U.S. standard population.
† Significant at p<0.05. Trends were measured with AAPC in rates and were considered to increase or decrease if p<0.05; otherwise rates were considered stable.
§ HPV-associated cancers were defined as cancers at specific anatomic sites with specific cell types in which HPV DNA frequently is found. All cancers were microscopically confirmed. Cervical cancers (International Classification of Diseases for Oncology, Third Edition [ICD-O-3] site codes C53.0–C53.9) are limited to carcinomas (ICD-O-3 histology codes 8010–8671, 8940–8941). Vaginal (ICD-O-3 site code C52.9), vulvar (ICD-O-3 site codes C51.0–C51.9), penile (ICD-O-3 site codes C60.0–60.9), anal (including rectal SCC; ICD-O-3 site code C20.9, C21.0–C21.9), and oropharyngeal (ICD-O-3 site codes C01.9, C02.4, C02.8, C05.1, C05.2, C09.0, C09.1, C09.8, C09.9, C10.0, C10.1, C10.2, C10.3, C10.4, C10.8, C10.9, C14.0, C14.2 and C14.8) cancer sites are limited to squamous cell carcinomas (ICD-O-3 histology codes 8050–8084, 8120–8131).
¶ Cancer incidence compiled from cancer registries that meet the data quality criteria for all invasive cancer sites combined (covering approximately 97.8% of the U.S. population).
** Data suppressed for rates when the number of cases was <6 in a year.
 FIGURE 1. Trends* in age-adjusted incidence of cervical carcinoma among females and oropharyngeal SCC among men,† — United States,§ 1999–2015
FIGURE 1. Trends* in age-adjusted incidence of cervical carcinoma among females and oropharyngeal SCC among men,† — United States,§ 1999–2015
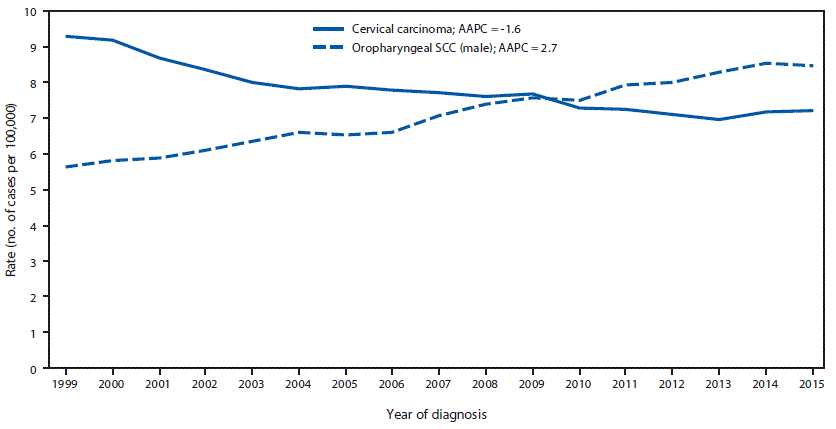
Sources: CDC’s National Program of Cancer Registries; National Cancer Institute’s Surveillance, Epidemiology, and End Results program.
Abbreviations: AAPC=average annual percent change; NS=not significant; SCC = squamous cell carcinoma.
* Trends were measured with AAPC in age-adjusted rates, and were considered to increase or decrease if p<0.05; otherwise trends were considered stable.
† HPV-associated cancers were defined as cancers at specific anatomic sites with specific cell types in which HPV DNA frequently is found. All cancers were microscopically confirmed. Cervical cancers (International Classification of Diseases for Oncology, Third Edition [ICD-O-3] site codes C53.0–C53.9) are limited to carcinomas (ICD-O-3 histology codes 8010–8671, 8940–8941). Oropharyngeal (ICD-O-3 site codes C01.9, C02.4, C02.8, C05.1, C05.2, C09.0, C09.1, C09.8, C09.9, C10.0, C10.1, C10.2, C10.3, C10.4, C10.8, C10.9, C14.0, C14.2 and C14.8) cancer sites are limited to squamous cell carcinomas (ICD-O-3 histology codes 8050–8084, 8120–8131).
§ Cancer incidence compiled from cancer registries that meet the data quality criteria for all invasive cancer sites combined for each year during the period 1999–2015 (covering 97.8% of the U.S. population).
The figure above is a line chart showing trends in age-adjusted incidence of cervical carcinoma among females and oropharyngeal SCC among men, in the United States during 1999–2015.
 FIGURE 2. Trends* in age-adjusted HPV-associated cancer incidence,† by cancer type and sex — United States,§ 1999–2015
FIGURE 2. Trends* in age-adjusted HPV-associated cancer incidence,† by cancer type and sex — United States,§ 1999–2015
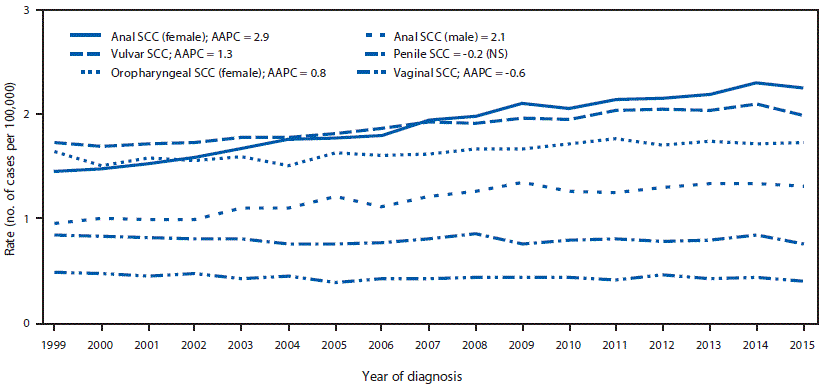
Sources: CDC’s National Program of Cancer Registries; National Cancer Institute’s Surveillance, Epidemiology, and End Results program.
Abbreviations: AAPC=average annual percent change; HPV = human papillomavirus; NS=not significant; SCC = squamous cell carcinoma.
* Trends were measured with AAPC in age-adjusted rates, and were considered to increase or decrease if p<0.05; otherwise trends were considered stable.
† HPV-associated cancers were defined as cancers at specific anatomic sites with specific cell types in which HPV DNA frequently is found. All cancers were microscopically confirmed. Vaginal (International Classification of Diseases for Oncology, Third Edition [ICD-O-3] site code C52.9), vulvar (ICD-O-3 site codes C51.0–C51.9), penile (ICD-O-3 site codes C60.0–60.9), anal (including rectal SCC; ICD-O-3 site code C20.9, C21.0–C21.9), and oropharyngeal (ICD-O-3 site codes C01.9, C02.4, C02.8, C05.1, C05.2, C09.0, C09.1, C09.8, C09.9, C10.0, C10.1, C10.2, C10.3, C10.4, C10.8, C10.9, C14.0, C14.2 and C14.8) cancer sites are limited to squamous cell carcinomas (ICD-O-3 histology codes 8050–8084, 8120–8131).
§ Cancer incidence compiled from cancer registries that meet the data quality criteria for all invasive cancer sites combined for each year during the period 1999–2015 (covering 97.8% of the U.S. population).
The figure above is a line chart showing trends in age-adjusted HPV-associated cancer incidence, by cancer type and sex in the United States during 1999–2015.
Sources: CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results program.
Abbreviations: AAPC = average annual percent change; AI/AN = American Indian/Alaska Native; API = Asian or Pacific Islander; CI = confidence interval; SCC = squamous cell carcinoma.
* Per 100,000 persons, age-adjusted to the 2000 U.S. standard population.
† Significant at p<0.05. Trends were measured with AAPC in rates and were considered to increase or decrease if p<0.05; otherwise rates were considered stable.
§ HPV-associated cancers were defined as cancers at specific anatomic sites with specific cell types in which HPV DNA frequently is found. All cancers were microscopically confirmed. Cervical cancers (International Classification of Diseases for Oncology, Third Edition [ICD-O-3] site codes C53.0–C53.9) are limited to carcinomas (ICD-O-3 histology codes 8010–8671, 8940–8941). Vaginal (ICD-O-3 site code C52.9), vulvar (ICD-O-3 site codes C51.0–C51.9), penile (ICD-O-3 site codes C60.0–60.9), anal (including rectal SCC; ICD-O-3 site code C20.9, C21.0–C21.9), and oropharyngeal (ICD-O-3 site codes C01.9, C02.4, C02.8, C05.1, C05.2, C09.0, C09.1, C09.8, C09.9, C10.0, C10.1, C10.2, C10.3, C10.4, C10.8, C10.9, C14.0, C14.2 and C14.8) cancer sites are limited to squamous cell carcinomas (ICD-O-3 histology codes 8050–8084, 8120–8131).
¶ Racial categories are not mutually exclusive from Hispanic ethnicity. Rates are not presented for cases with unknown or other race or unknown ethnicity.
** Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, and Wisconsin. Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. South: Alabama, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
†† Cancer incidence compiled from cancer registries that meet the data quality criteria for all invasive cancer sites combined (covering approximately 97.8% of the U.S. population).
§§ Data suppressed for rates when the number of cases was <6 in a year.
Suggested citation for this article: Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in Human Papillomavirus–Associated Cancers — United States, 1999–2015. MMWR Morb Mortal Wkly Rep 2018;67:918–924. DOI: http://dx.doi.org/10.15585/mmwr.mm6733a2.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.

