Chronic Kidney Disease in the United States, 2023
Download the print version: Chronic Kidney Disease in the United States, 2023 [PDF – 516 KB]
When people develop chronic kidney disease (CKD), their kidneys become damaged and over time may not clean the blood as well as healthy kidneys. If kidneys do not work well, toxic waste and extra fluid accumulate in the body and may lead to high blood pressure, heart disease, stroke, and early death. However, people with CKD and people at risk for CKD can take steps to protect their kidneys with the help of their health care providers.
CKD Is Common Among US Adults
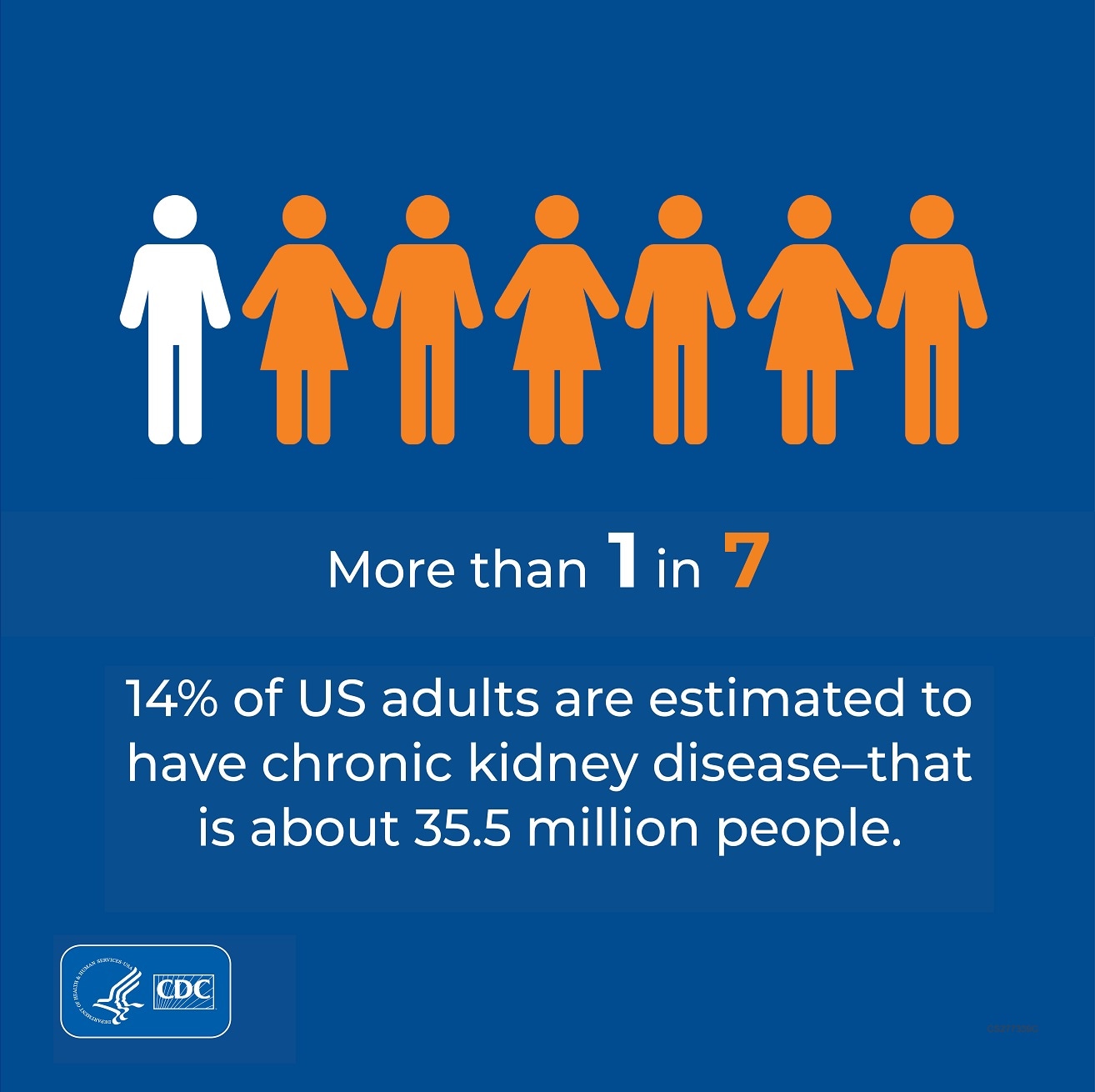
- More than 1 in 7 US adults–about 35.5 million people, or 14%–are estimated to have CKD.†
- As many as 9 in 10 adults with CKD do not know they have it.
- About 1 in 3 adults with severe CKD do not know they have CKD.
CKD by Age, Sex, and Race/Ethnicity
According to current estimates:†
- CKD is more common in people aged 65 years or older (34%) than in people aged 45–64 years (12%) or 18–44 years (6%).
- CKD is slightly more common in women (14%) than men (12%).
- CKD is more common in non-Hispanic Black adults (20%) than in non-Hispanic Asian adults (14%) or non-Hispanic White adults (12%).
- About 14% of Hispanic adults have CKD.
Percentage of US Adults Aged 18 Years and Older With CKD,† by Age, Sex, and Race/Ethnicity
†How estimates were calculated: Percentage of CKD stages 1–4 among US adults aged 18 years and older using data from the 2017–March 2020 National Health and Nutrition Examination Survey based on 2021 CKD Epidemiology Collaboration GFR estimating equation, including serum creatinine, age, and sex. CKD stage 5 (that is, kidney failure) was not included. Severe CKD refers to stage 4. These estimates were based on a single measure of albuminuria or serum creatinine; they do not account for persistence of albuminuria or elevated creatinine as indicated by the Kidney Disease Improving Global Outcomes recommendations. Thus, CKD in this report might be overestimated. Estimates by sex and race/ ethnicity were age-standardized using the 2010 US Census population; the overall percentage is unadjusted. The number of adults with CKD stages 1–4 was estimated by applying the overall percentage to the 2019 US Census population aged 18 years and older. Blood pressure–lowering medicines included angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers; blood sugar–lowering medicines included GLP-1 receptor agonists, SGLT2 inhibitors, and DPP-4 inhibitors; diagnosed diabetes was self-reported.
The following organizations** collaborated in developing and reviewing this fact sheet. Check their websites for CKD online resources for patients or providers:
- Centers for Disease Control and Prevention, Chronic Kidney Disease Initiative
- Centers for Medicare & Medicaid Services
- US Department of Defense
- US Department of Veterans Affairs
- US Food & Drug Administration
- Kidney Interagency Coordinating Committee
- National Heart, Lung, and Blood Institute of the National Institutes of Health
- National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health
- United States Renal Data System
- American Association of Kidney Patients
- American Society of Nephrology
- National Kidney Foundation
- University of California, San Francisco, and University of California, San Francisco Center for Vulnerable Populations
- University of Michigan, Division of Nephrology, Department of Internal Medicine, and University of Michigan Kidney Epidemiology and Cost Center
**Links to nonfederal organizations are provided solely as a courtesy. Links do not constitute an endorsement of any organization by CDC, the Department of Army/Navy/Air Force, Department of Defense, or the federal government and none should be inferred. CDC is not responsible for the content of individual organization’s web pages.
Note: This publication is not subject to copyright restrictions; duplicate and distribute copies as desired.
Citation: Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2023. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2023.
For Public Inquiries and Publications
CDC-INFO Contact Center
Telephone: 1-800-CDC-INFO (232-4636), 1-888-232-6348 TTY
Email: cdcinfo@cdc.gov
In English and Spanish
24 hours a day, 7 days a week
- National Institutes of Health. Health Information: Chronic Kidney Disease website. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd. Accessed 3/24/2023.
- Kidney Disease: Improving Global Outcomes CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter. 2013;3(1)(suppl):1–150.
- United Stated Renal Data System 2022 Annual Data Report. https://usrds-adr.niddk.nih.gov/2022. Accessed 3/24/2023.
- Diabetes in CKD. https://kdigo.org/guidelines/diabetes-ckd/. Accessed 3/24/2023.