HIV Infection Risk, Prevention, and Testing Behaviors Among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 13 U.S. Cities, 2021: Commentary
Lowering the annual number of new HIV infections is a major HIV prevention goal [1]. This goal can be achieved by implementing three important strategies for reducing HIV infections: (1) intensifying HIV prevention efforts among populations with high burden of HIV, including gay, bisexual, and other men who have sex with men (hereafter referred to as MSM); Black or African American people (hereafter referred to as Black); Hispanic or Latino people; and people who inject drugs (PWID); (2) expanding efforts to prevent HIV infection by using a combination of effective, evidence-based, scalable approaches; and (3) educating the general public about HIV infection and how to prevent it. State and local health departments, as well as federal agencies, are expected to monitor progress toward HIV prevention goals [1].
National HIV Behavioral Surveillance (NHBS) provides data for monitoring behaviors among populations at risk of acquiring or transmitting HIV infection and identifies the populations for whom scientifically proven, cost-effective, and scalable interventions are most appropriate. Monitoring key indicators among members of populations disproportionally affected by HIV is critical to achieving the goals of the Ending the HIV Epidemic in the U.S. (EHE) Initiative [2] and the Centers for Disease Control and Prevention (CDC)’s high-impact prevention (HIP) approach [3]. The EHE Initiative is aimed at reducing new HIV infections by 90% by 2030 by implementing evidence-based strategies for specific populations in geographic areas most affected by HIV. NHBS has previously proven effective at monitoring key indicators, such as behavioral risk factors, HIV testing, and linkage to care; access to and use of prevention interventions, including preexposure prophylaxis (PrEP) and syringe services programs (SSPs); and prevalence of HIV in areas with high HIV prevalence among 3 populations at high risk of HIV infection: MSM, PWID, and heterosexually active persons at increased risk for HIV infection [4, 5].
Male-to-male sexual contact continues to be the most common route of HIV transmission in the United States among adults and adolescents, accounting for approximately 72% of the HIV infections diagnosed in 2020, including those attributed to the combination of male-to-male contact and injection drug use [6]. This report summarizes findings from the 2021 NHBS data collection cycle among MSM. Data from previous MSM cycles of NHBS have been published elsewhere [7–11].
The report provides descriptive, unweighted data that can be used to describe HIV infection among MSM and the percentages reporting specific behavioral risk factors, HIV testing, and participation in prevention programs. Monitoring these outcomes is useful for assessing behavioral risk factors and the use of prevention efforts over time and for identifying new HIV prevention opportunities for this population.
Report Changes
CDC routinely assesses NHBS reports to ensure the content and methods best meet the information needs of the nation. The following reporting changes were made from the previous NHBS report on MSM [11]:
- In 2021, 23 metropolitan statistical areas (MSAs) participated in NHBS among MSM; however, this report includes data from 13 MSAs that met the threshold for sufficient sample size (Figure 1; see Data Analysis section).
- In previous MSM cycles a venue-based sampling (VBS) method was used to collect data. As a result of the COVID-19 pandemic, 2 sampling methods were used in the 2021 cycle: respondent-driven sampling (RDS) and virtual venues sampling (VVS). The results in this report combine data from both sampling methods.
- Due to the impact of the COVID-19 pandemic, in addition to the standard NHBS HIV testing protocol (i.e., blood specimens collected for rapid HIV testing with rapid or laboratory-based supplemental testing), the NHBS HIV testing protocol could be modified locally to include testing without in-person contact, such as offering only one rapid oral HIV self-test. As a result, rapid or laboratory-based supplemental testing was not always performed to confirm infection. Therefore, HIV status in this report (Table 1) is reported using the following 4 categories: HIV-negative, HIV-positive, presumed HIV-positive, and no valid HIV test result.
- Tables are not stratified by participants’ HIV status determined from the NHBS HIV test results (i.e., HIV-positive, HIV-negative, and no valid NHBS HIV test results); instead, some tables include a new row ‘self-reported HIV-positive (Yes/No)’, which serves as a proxy for the traditional stratification by HIV status.
- A new indicator, ‘unprotected sex with an HIV-discordant partner at last sex’, was developed and presented for the first time in this report. This indicator accounts for sex without the participant’s use of either condoms or HIV medications (i.e., PrEP among those without HIV or antiretrovirals among those with HIV) with a sex partner of different or unknown HIV status.
Some modifications to “measure definitions” are made routinely to more accurately, or more precisely, describe the outcome or characteristic of interest; measure definitions are described in the appendix of this report.
Figure 1. Participating National HIV Behavioral Surveillance project areas—United States, 2021
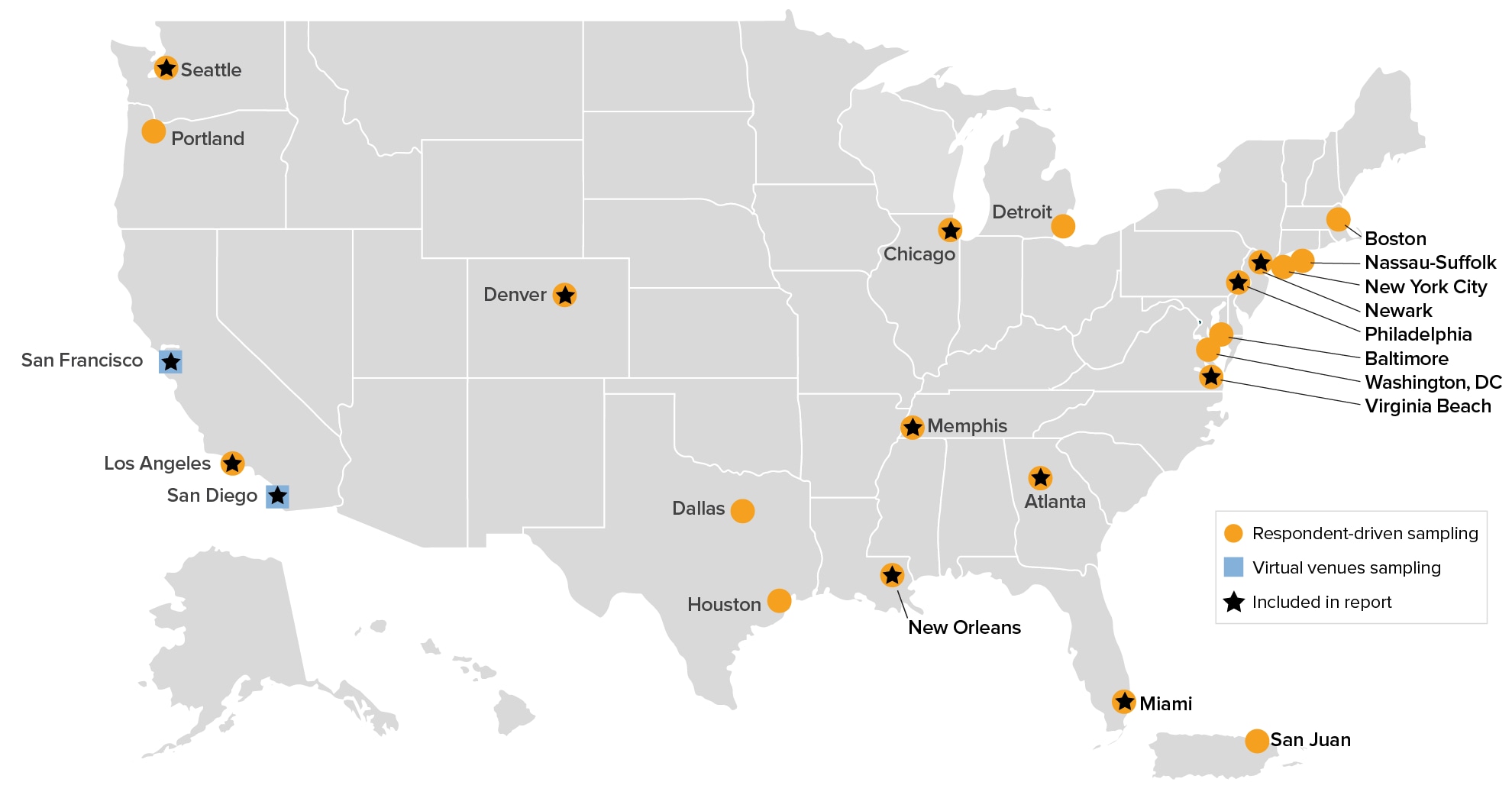
Note. In 2021, 23 metropolitan statistical areas (MSAs) participated in National HIV Behavioral Surveillance among gay, bi-sexual, and other men who have sex with men (MSM); 13 MSAs met the threshold for sufficient sample size.
Highlights
Demographic Characteristics, HIV Testing, and Preexposure Prophylaxis
This report describes data from 2,241 MSM who participated in NHBS in 2021, of whom 26% were aged 29 years or younger (Figure 2), 38% were Black, 27% were White, and 25% were Hispanic or Latino (Figure 3; Table 1). Overall, 71% of MSM had more than a high school education and 71% had a household income above the federal poverty level; 86% of MSM had health insurance and 89% had visited a health care provider in the 12 months before interview; 30% of MSM reported having a disability and 18% reported being unemployed; 14% experienced homelessness and 6% were incarcerated in the 12 months before interview (Figure 4).
Figure 2. Age distribution of men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
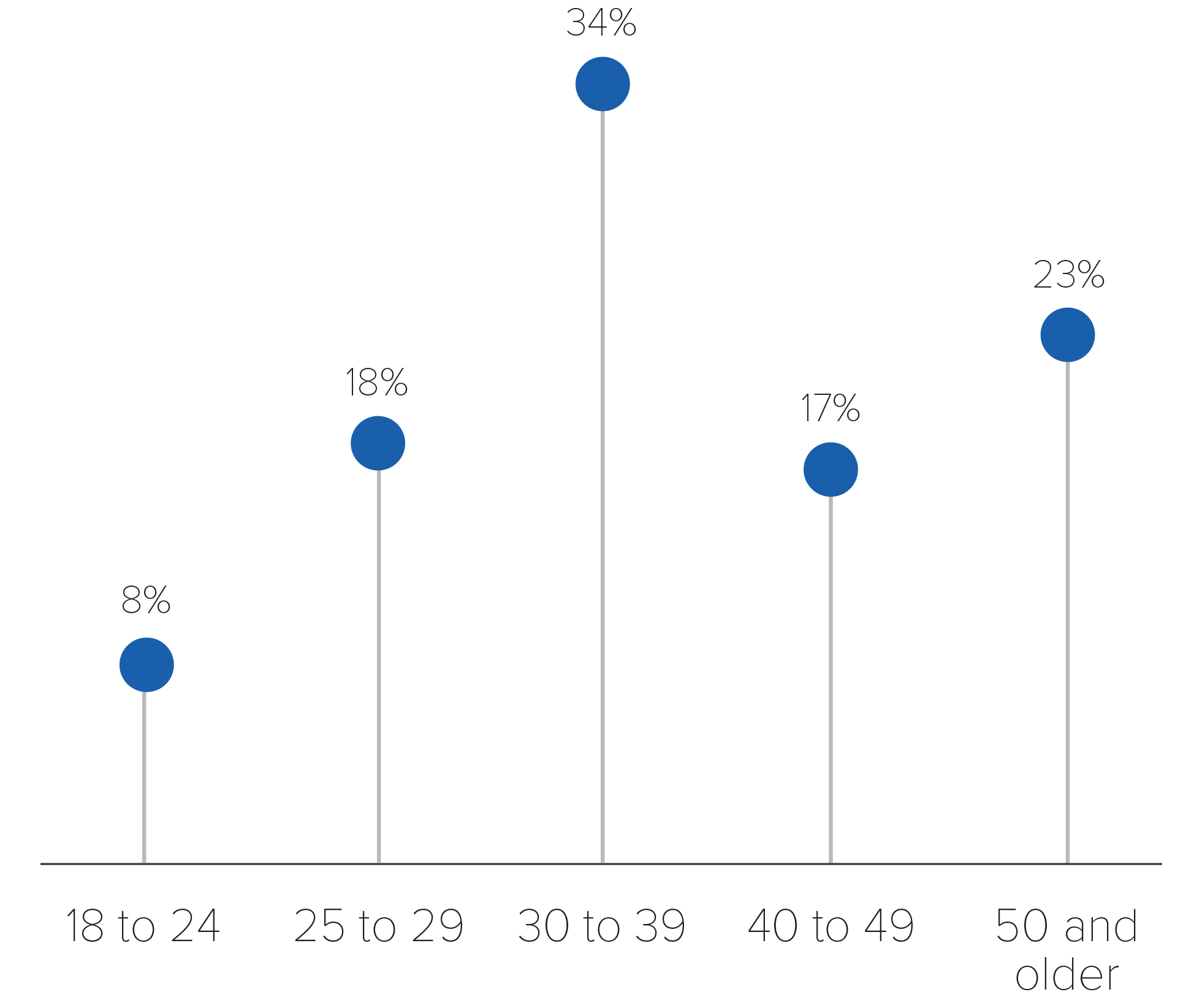
Figure 3. Race/ethnicity distribution of men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
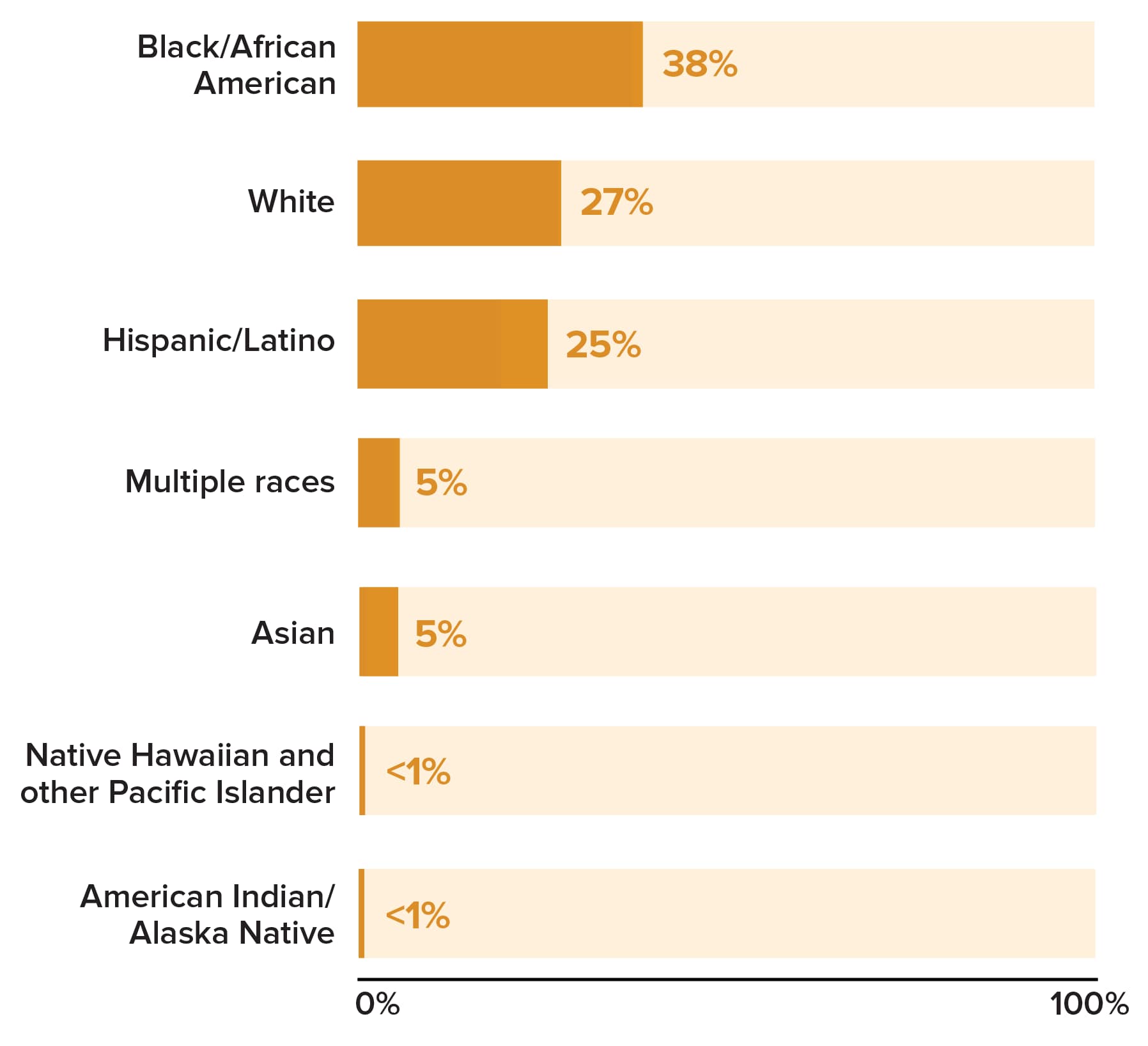
Note. Hispanic/Latino persons can be of any race.
Figure 4. Social determinants of health among men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
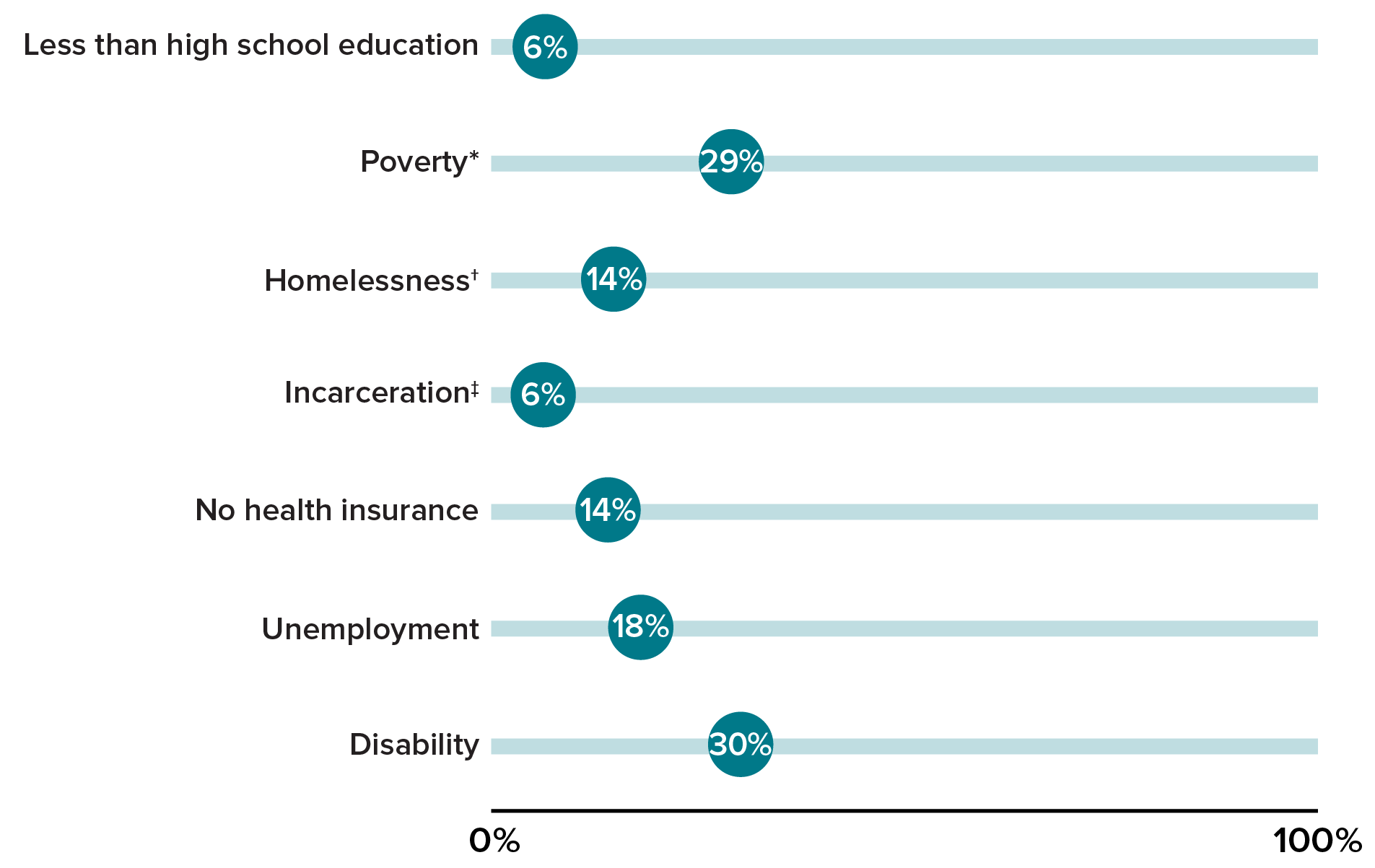
* Poverty level is based on household income and household size.
† Homelessness is defined as living on the street, in a shelter, in a single-room-occupancy hotel, or in a car in the 12 months before interview.
‡ Incarceration is defined as having been held in a detention center, jail, or prison for more than 24 hours in the 12 months before interview.
CDC recommends that persons with risk factors for HIV infection, including sexually active MSM, undergo HIV testing at least annually [12]. Among MSM who (1) did not report a previous HIV-positive test result or (2) had received their first HIV-positive test result less than 12 months before interview, 76% reported that they had been tested for HIV in the 12 months before interview (Figure 5), and 95% reported that they had ever been tested (Table 2).
In 2021, CDC released an update to clinical guidance recommending the use of PrEP for persons at an increased risk of HIV acquisition, including MSM [13]. Among participants who did not report a previous HIV-positive test result and participants who received their first HIV-positive test result less than 12 months before interview, the majority reported previously hearing about PrEP (89%) and 42% reported taking PrEP in the past 12 months (Figure 5); 57% of White MSM reported taking PrEP compared with 44% of Hispanic or Latino MSM and 24% of Black MSM.
Figure 5. Prevalence of HIV testing and preexposure prophylaxis among men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
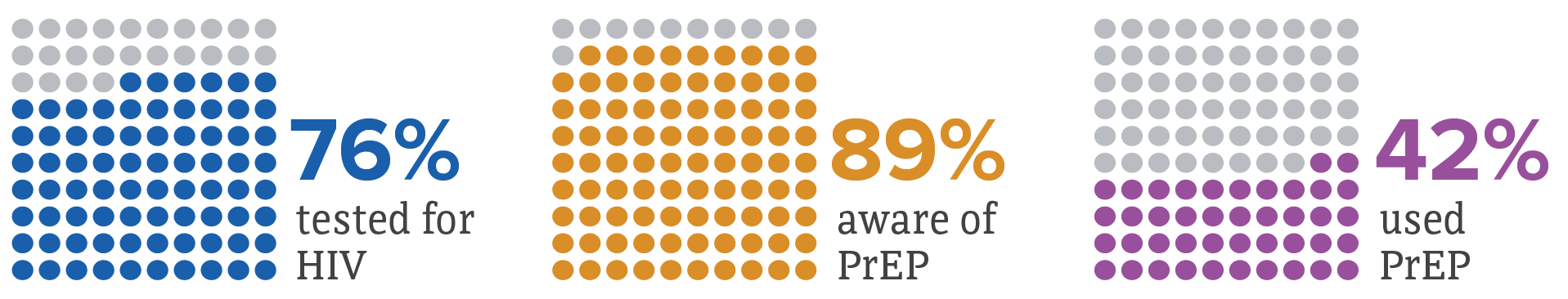
Abbreviation: PrEP, preexposure prophylaxis.
Note. Among participants who did not report a previous HIV-positive test result and participants who received their first HIV-positive test result less than 12 months before interview. HIV testing and PrEP use are in the 12 months before interview. PrEP awareness is ever.
Among MSM who were tested for HIV in the past 12 months, 72% reported their most recent test was performed in a clinical setting (Figure 6), while 25% reported being tested in a nonclinical setting such as an HIV counseling and testing site, an HIV street outreach program or mobile unit, a syringe services program, or at home (Table 3). Testing in nonclinical settings varied by race and ethnicity: 32% of Black MSM and 29% of Hispanic or Latino MSM reported their most recent HIV test was conducted in a nonclinical setting, while 15% of White MSM reported a nonclinical setting for their most recent HIV test.
Figure 6. Setting of most recent HIV test among men who have sex with men and who were tested for HIV during the 12 months before interview—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
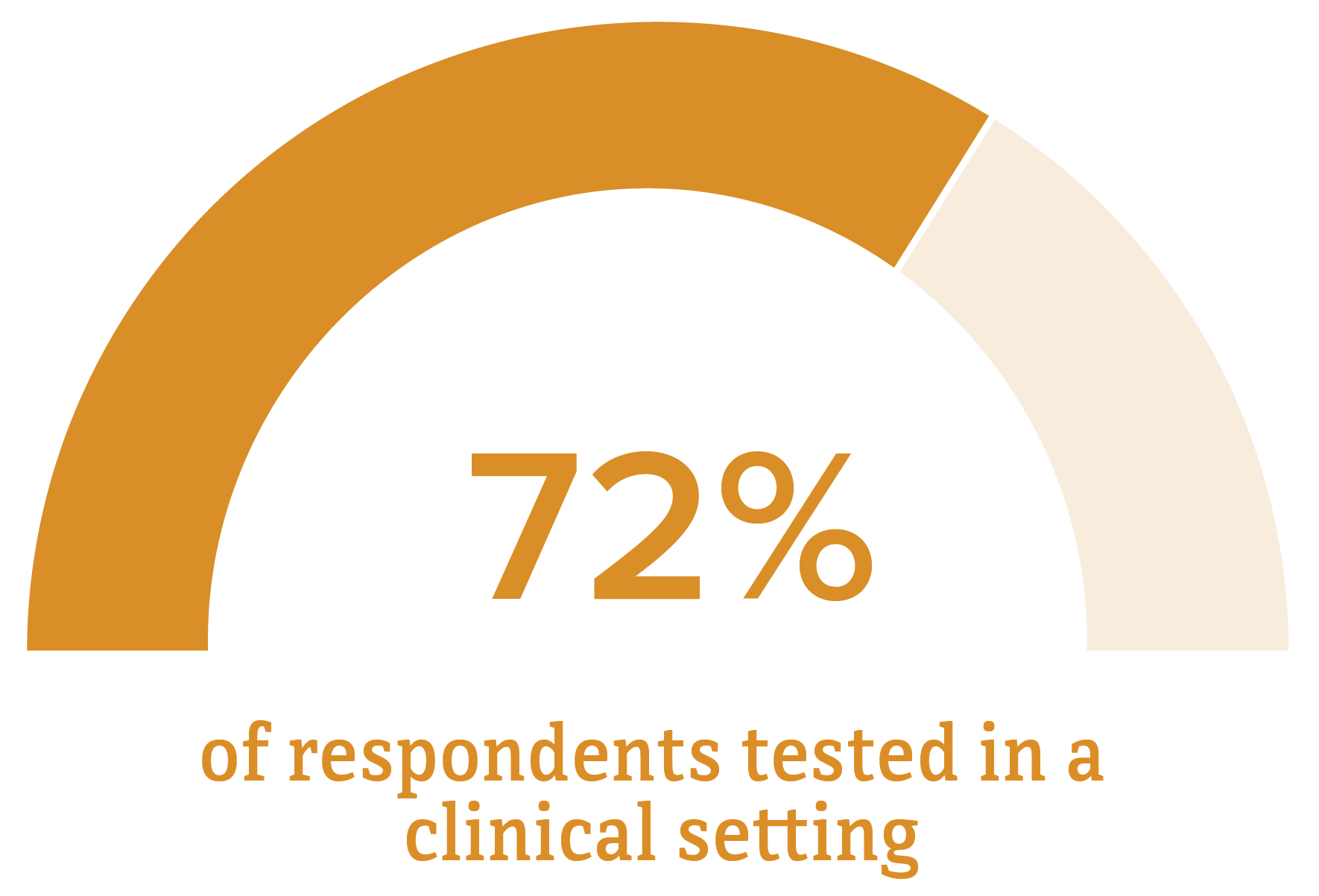
Note. Clinical settings include private doctor’s office (including health maintenance organization), emergency department, hospital (inpatient), public health clinic or community health center, family planning or obstetrics clinic, correctional facility, or drug treatment program.
Sexual Behaviors
Condomless anal sex with male partners was reported by 77% of MSM regardless of self-reported HIV status (Figure 7; Table 4). Condomless vaginal or anal sex with female sex partners was higher among MSM who did not self-report HIV-positive (10% and 6%, respectively) than among MSM who self-reported HIV-positive (4% and 2%, respectively). MSM who self-reported HIV-positive reported condomless anal sex with main and casual male partners (44% and 55%, respectively) at a similar percentage to MSM who did not self-report HIV-positive (50% and 53%, respectively) (Table 5). Among MSM, 19% reported having a male last sex partner but not having had anal sex with him during their last sexual encounter, and this did not differ by self-reported HIV status (Table 6).
Figure 7. Sexual behaviors among men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
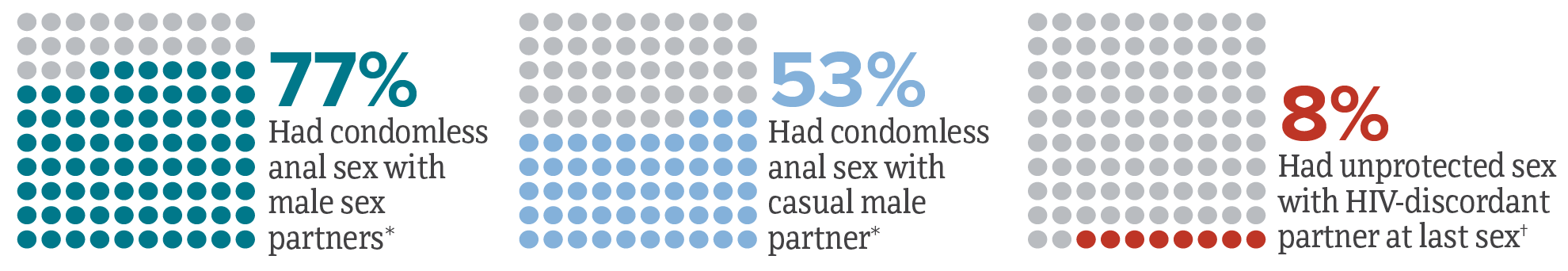
* Condomless anal sex with male sex partners and condomless anal sex with casual male partner are in the 12 months before interview.
† Unprotected sex refers to sex without the participant’s use of either condoms or HIV medications (i.e., HIV PrEP or antiretrovirals). HIV-discordant partner refers to a sex partner of different or unknown HIV status.
Despite the existence of other HIV prevention options, correct and consistent condom use is one of the primary means of protection from HIV and other infections [14, 15]. The high percentages of MSM who engaged in condomless sex underscore the importance of using effective, evidence-based scalable combination HIV prevention strategies among MSM at increased risk for HIV infection that include access to and use of condoms, PrEP, risk-reduction counseling, and HIV testing [3, 13].
Sexually Transmitted Infections
Sexually transmitted infections (STIs) can increase the likelihood of acquiring and transmitting HIV [16]. The percentage of MSM who reported a diagnosis of any bacterial STI (chlamydia, gonorrhea, or syphilis) during the 12 months before interview was 23% overall (Figure 8) and was higher among MSM who self-reported HIV-positive (33%) than among MSM who did not self-report HIV-positive (19%). Percentages of lifetime diagnosis of genital warts (18%) and genital herpes (13%) among MSM who self-reported HIV-positive were also higher than among MSM who did not self-report HIV-positive (8% for genital warts and 8% for genital herpes) (Table 7).
Figure 8. Diagnosis of sexually transmitted infections in the 12 months before interview among men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
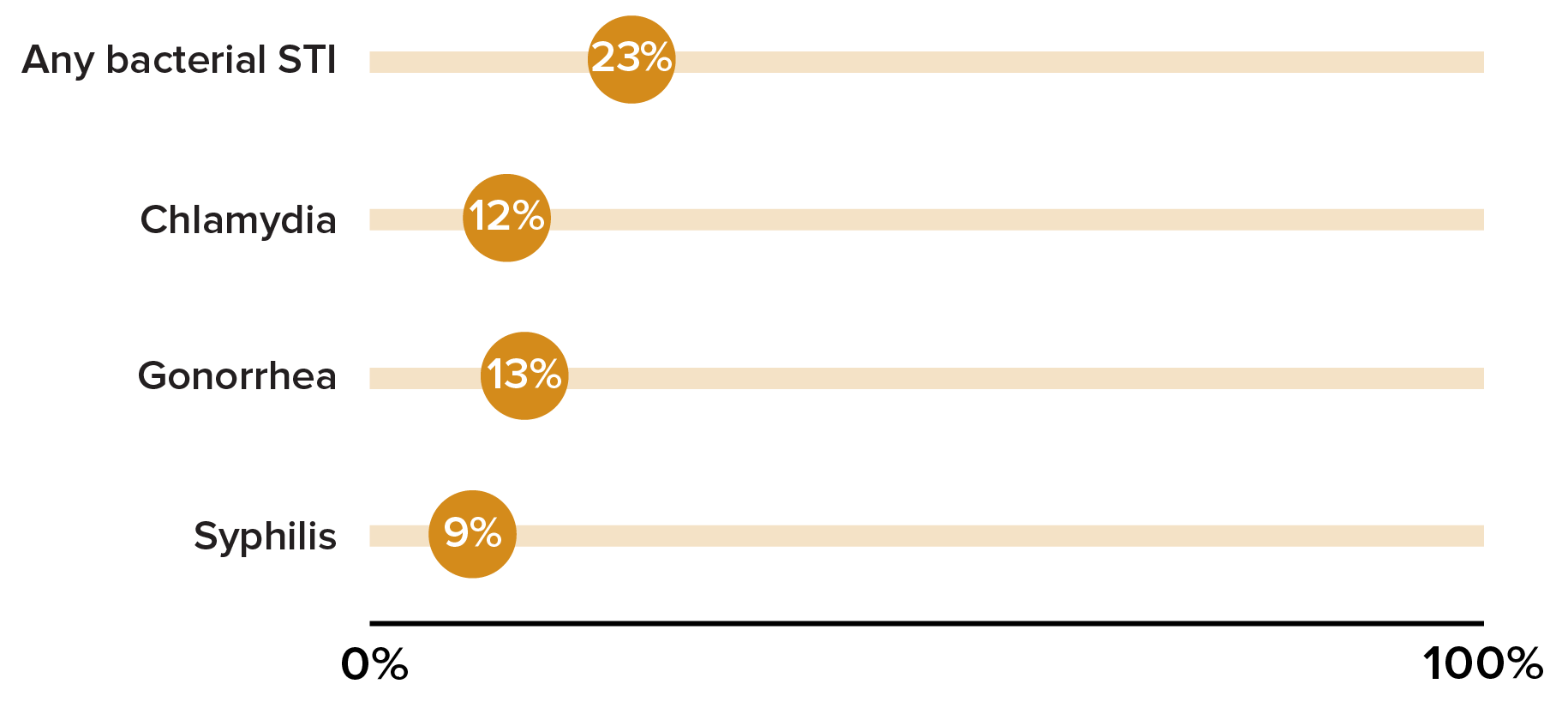
Abbreviation: STI, sexually transmitted infection.
Note. “Any bacterial STI” includes having received a diagnosis of gonorrhea, chlamydia, or syphilis in the 12 months before interview.
Since 2000, rates of primary and secondary syphilis have increased among men, likely attributable to increases in cases among MSM; however, increases among MSM have slowed in recent years and during 2019-2020, the number of cases of primary and secondary syphilis among MSM decreased 2.2%. Still, MSM are disproportionately impacted, accounting for a majority (53%) of all male primary and secondary syphilis cases in 2020 [17]. In the current NHBS cycle, 20% of MSM who self-reported HIV-positive reported receiving a syphilis diagnosis during the 12 months before interview compared with 5% of MSM who did not self-report HIV-positive.
Drug and Alcohol Use
Drug and alcohol use, particularly binge drinking, injection drug use, and methamphetamine use, have been associated with sexual risk behavior among MSM [18]. Among MSM, 17% reported binge drinking in the past 30 days, while 59% reported using marijuana, 18% reported using cocaine, 16% reported using ecstasy, and 14% reported using methamphetamine in the 12 months before interview (Figure 9; Table 8). Non-injection use of any drug in the 12 months before interview was reported by 65% of MSM while any injection drug use was reported by 6% of MSM.
Figure 9. Drug use in the 12 months before interview and binge drinking in the 30 days before interview among men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
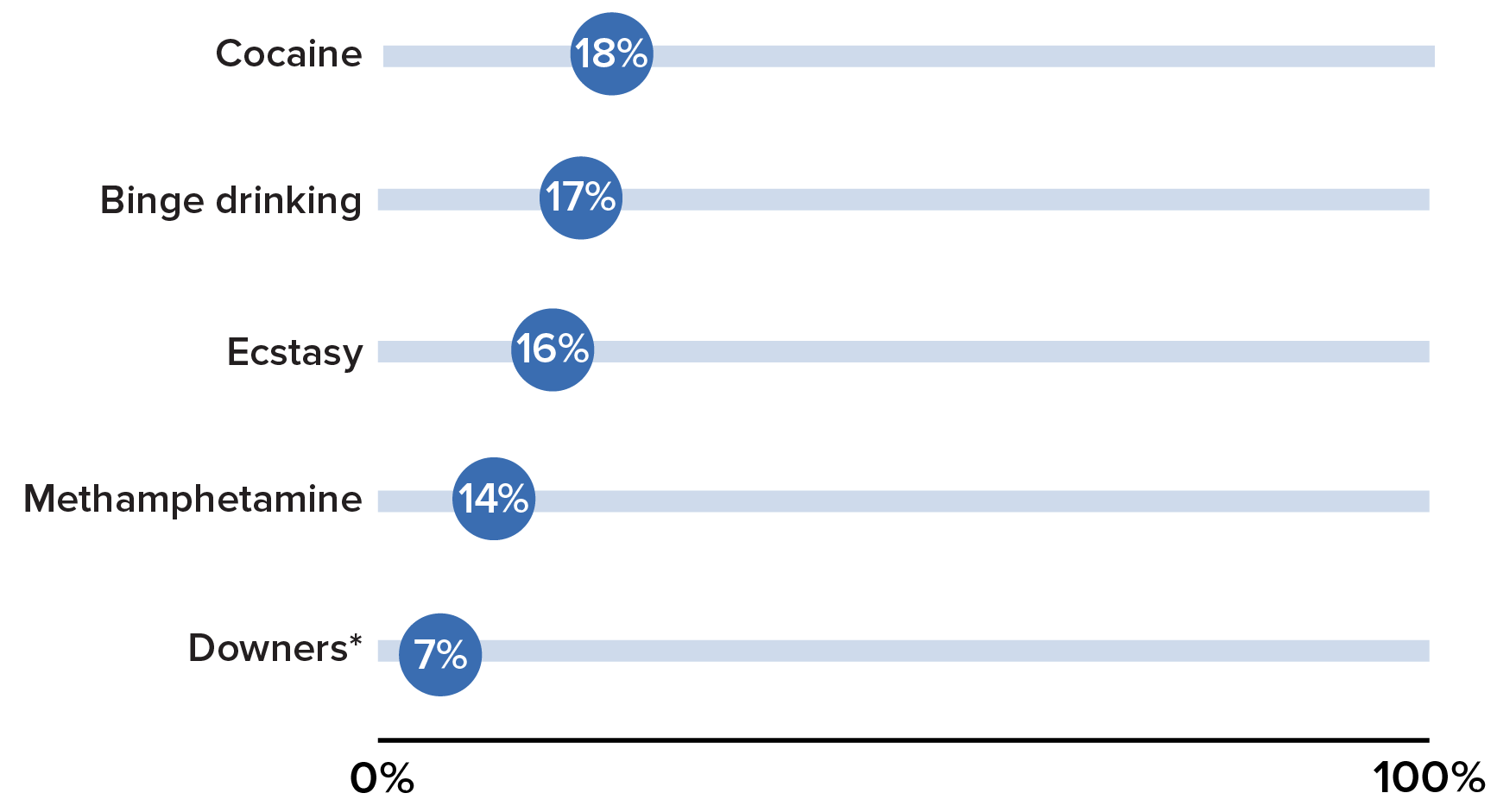
Disclaimer: The use of trade names is for identification only and does not imply endorsement by the Department of Health and Human Services or the Centers for Disease Control and Prevention.
Note. Binge drinking defined as 5 or more drinks at one sitting during the 30 days before interview.
* Downers such as Klonopin, Valium, Ativan, or Xanax.
Additional Outcomes
Table 9 presents data on additional outcomes related to the risk of HIV transmission and acquisition among MSM. Outcomes reported in Table 9 are of current relevance to HIV among MSM and may not be reported in future reports.
The median number of male sex partners reported in the 12 months before interview was 4 (Q1–Q3: 2–10) among MSM regardless of self-reported HIV-positive status.
Giving or receiving money or drugs in exchange for sex is a recognized risk factor for HIV infection [19]. In 2021, 13% of MSM reported giving or receiving things like money or drugs in exchange for sex with a male casual partner in the 12 months before interview (Figure 10). The percentage of MSM reporting exchange sex with a male casual partner was higher among MSM who self-reported HIV-positive (18%) than among MSM who did not self-report HIV-positive (11%).
Figure 10. Exchanged sex in the 12 months before interview among men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
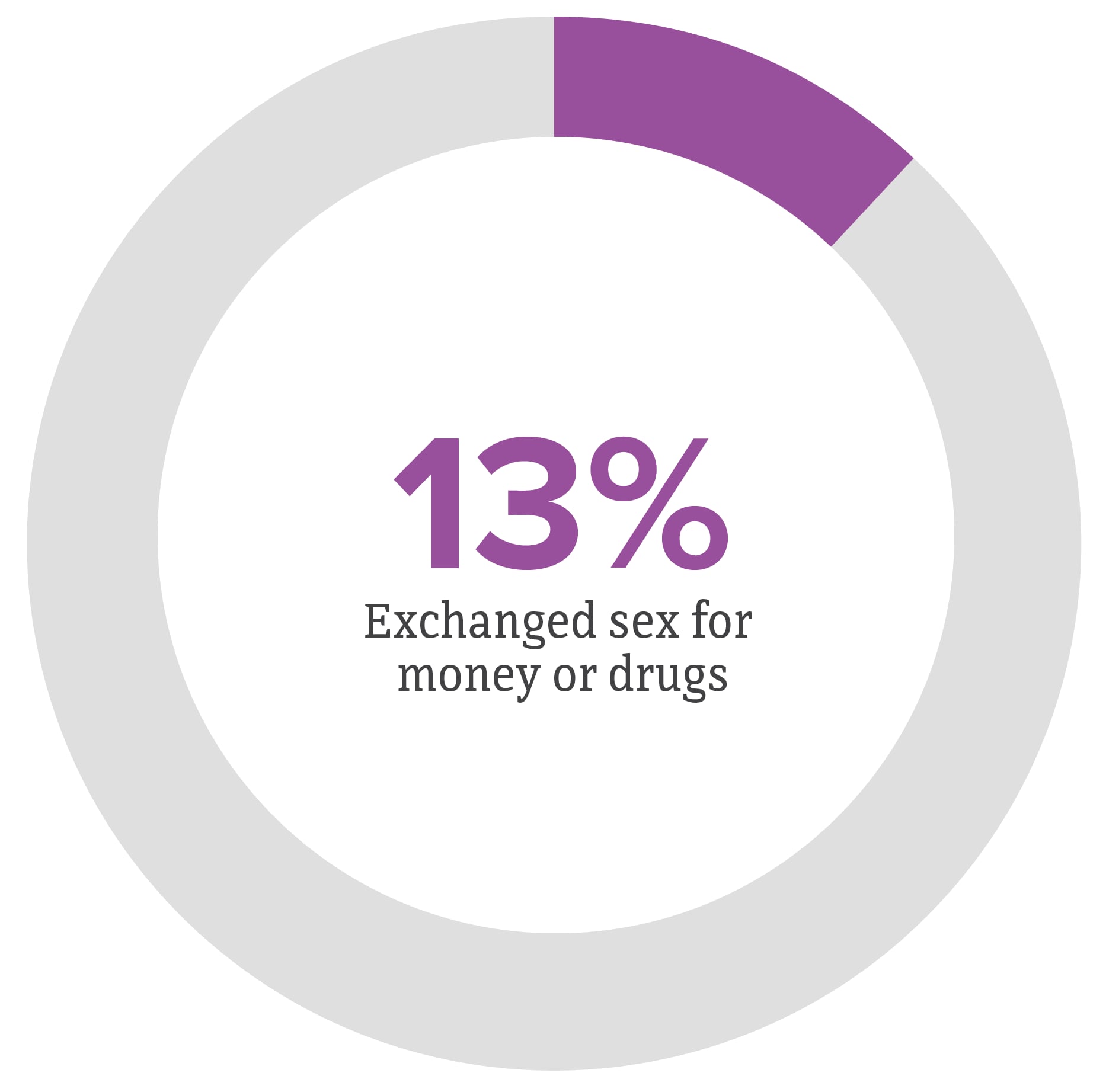
Note. Exchanged sex refers to giving or receiving money or drugs from a male casual partner in exchange for sex.
Overall, 8% of MSM reported unprotected sex with an HIV-discordant partner at last sex (Figure 7); this percentage was lower among MSM who self-reported HIV-positive (1%) compared with MSM who did not self-report HIV-positive (11%).
Overall, 51% of MSM reported receiving free condoms and 27% reported participating in an HIV behavioral intervention (Figure 11). The percentage of MSM who received condoms were higher among MSM who self-reported HIV-positive (61%) compared with MSM who did not self-report HIV-positive (47%). The percentage of MSM who reported participating in an HIV behavioral intervention was highest for MSM who self-reported HIV-positive (34%) and, among all MSM, for the youngest age group (32% of MSM aged 18–24 years).
Figure 11. Percentage of men who have sex with men receiving free condoms in the 12 months before interview—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
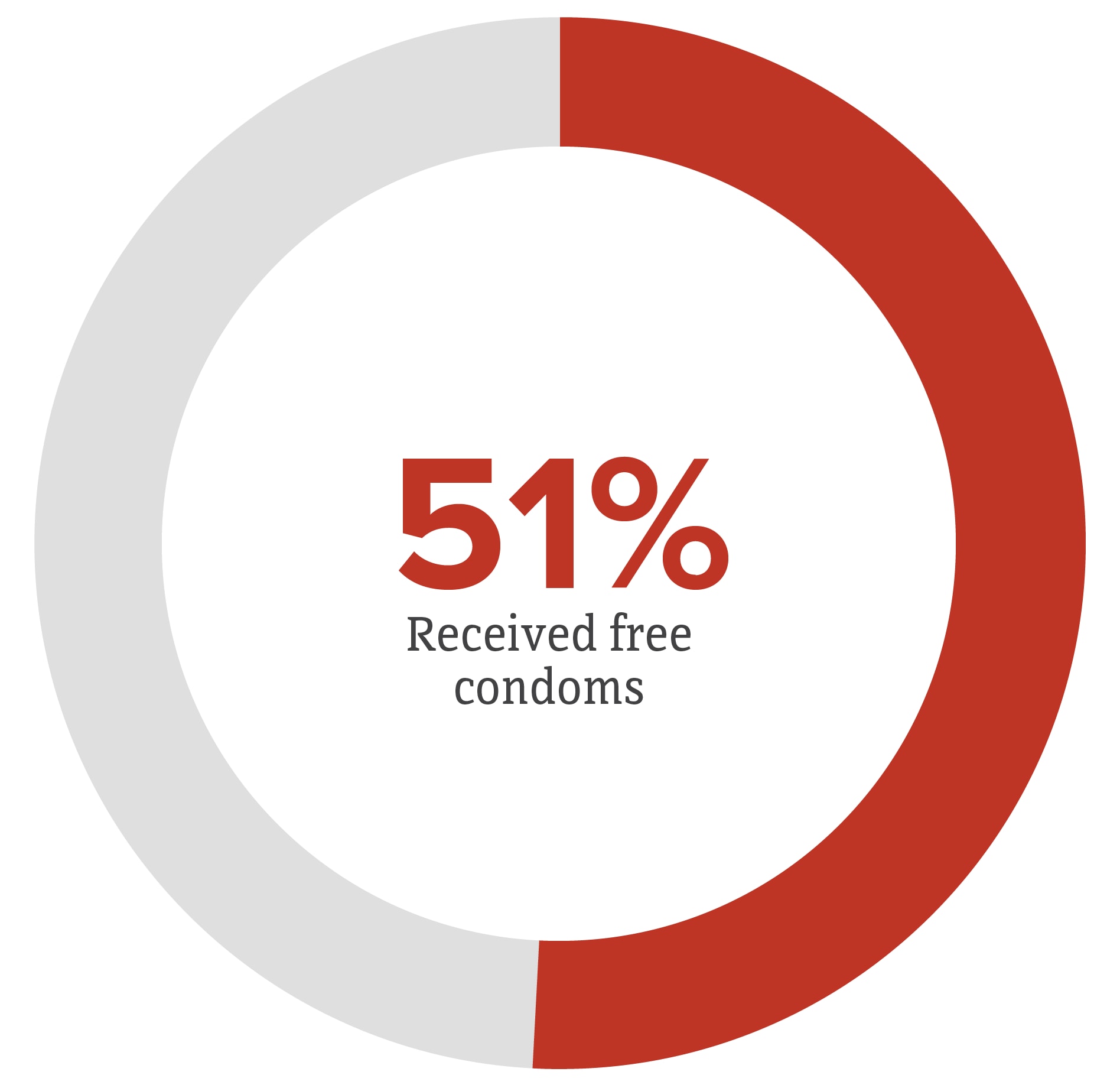
Note. Excludes condoms received from friends, relatives, or sex partners.
Receipt of HIV Care and Treatment
Achieving viral suppression through antiretroviral treatment improves clinical outcomes and reduces the likelihood of transmitting HIV to others [20]. The national goal is to link a person with a new HIV diagnosis to care within one month of diagnosis [1]. In 2021, among MSM who self-reported HIV-positive, 98% reported having ever visited a health care provider for HIV, 69% reported that they did so within one month after diagnosis, and 88% reported visiting a health care provider for HIV care in the six months before interview (Table 10). Current use of antiretroviral treatment was reported by 95% of MSM who self-reported HIV-positive (Figure 12).
Figure 12. Current antiretroviral use among self-reported HIV-positive men who have sex with men—National HIV Behavioral Surveillance, 13 U.S. cities, 2021
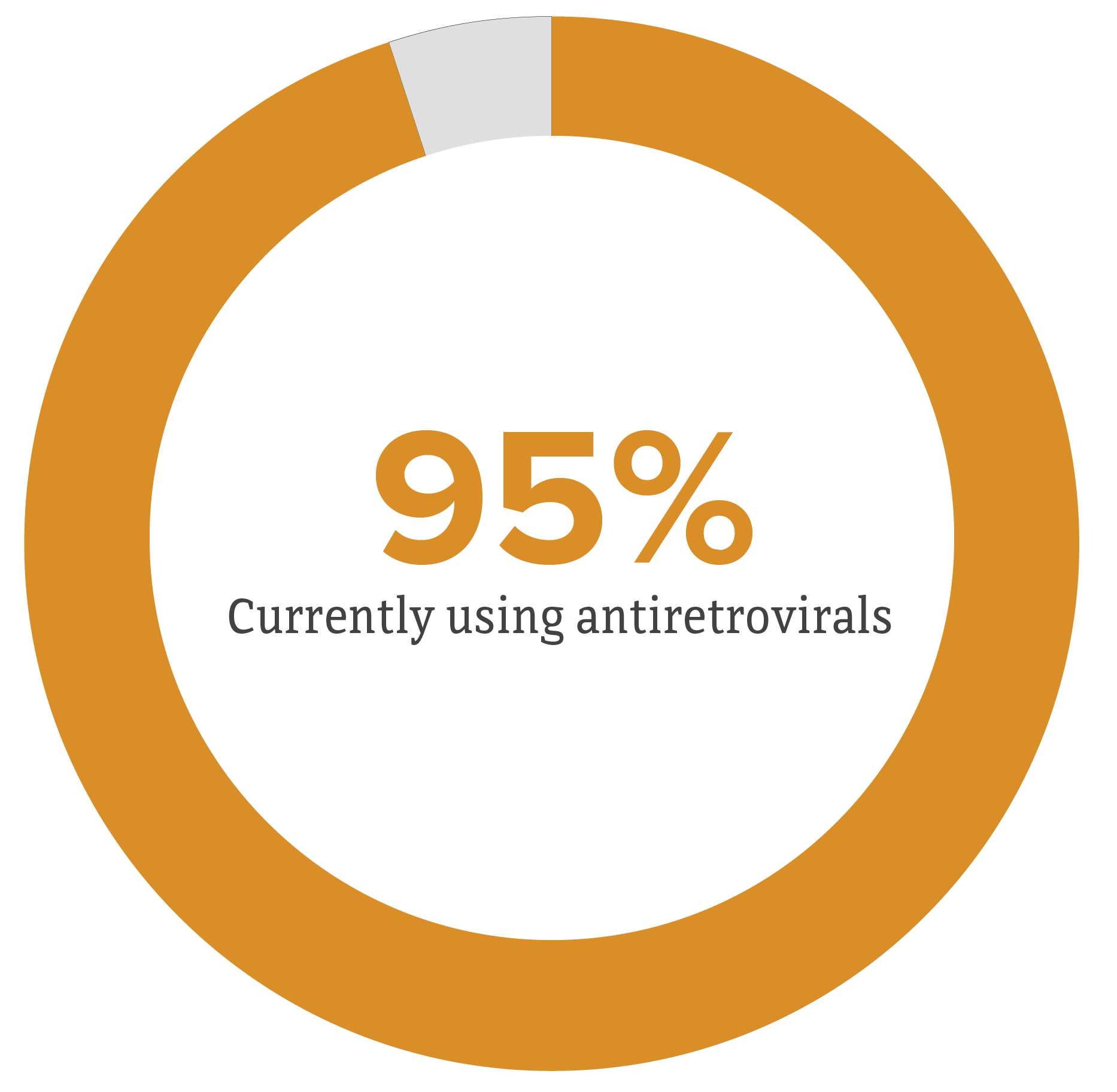
Note. Includes all participants who reported having ever received an HIV-positive test result, regardless of National HIV Behavioral Surveillance HIV test result.
