Acute Flaccid Myelitis Task Force Update
May 7, 2019
Also available as Printable PDF pdf icon[PDF – 250 KB, 13 pages]
Slide 1
Acute Flaccid Myelitis Task Force Update
Ruth Lynfield, MD and Jill Taylor, PhD
AFM-TF Co-chairs
CDC Board of Scientific Counselors, Office of Infectious Diseases
Atlanta, GA
May 7, 2019
Slide 2

AFM Task Force – Terms of Reference
Present findings, observations, and outcomes to CDC Board of Scientific Counselors (BSC), Office of Infectious Diseases for discussion, deliberation, and decision
- Etiologies and pathogenesis
- Evaluate current understanding and the pathogenic mechanisms of AFM
- Review available data and develop hypotheses about possible or likely etiologies and the pathogenesis of AFM
- Propose new studies, study designs, laboratory techniques, assays, and other activities to address specific hypotheses on AFM etiologies and pathogenesis
- Develop and prioritize findings and observations for the BSC to utilize in the development of recommendations for areas of further study or investigation
- Clinical treatment
- Build on existing information on clinical practices by seeking information on clinical experience with the treatment of AFM
- Identify research gaps in the diagnosis and treatment of AFM
- Develop potential findings and observations on patient management for referral to the BSC
Slide 3

AFM Task Force Membership
BSC Members
- Emily Erbelding, National Institutes of Health, Div. of Microbiology & Infectious Diseases (Ex Officio)
- Ruth Lynfield, Minnesota Dept. of Health
- Bonnie Maldonado, Stanford University School of Medicine, Depts. of Pediatrics and Health Research and Policy
- Jill Taylor, New York State Dept. of Health, Wadsworth Laboratory
AFM Clinical and Research Experts
- Leslie Benson, Boston Children’s Hospital, Dept. of Neurology
- Benjamin Greenberg, University of Texas Southwestern Medical Center, Dept. of Neurology and Neurotherapeutics
- Bryan Grenfell, Princeton University, Ecology and Evolutionary Biology and Public Affairs, Woodrow Wilson School
- Tory Johnson, Johns Hopkins University School of Medicine, Dept. of Neurology
- Kevin Messacar, University of Colorado School of Medicine, Dept. of Pediatrics
- John Modlin, Bill & Melinda Gates Foundation, Polio Research and Policy
- Nancy Murphy, University of Utah, Dept. of Pediatrics and Physical Medicine & Rehabilitation
- Avi Nath, National Institutes of Health, National Institute of Neurological Disorders and Stroke
- Carlos Pardo-Villamizar, Johns Hopkins University School of Medicine, Dept. of Neurology, Johns Hopkins Transverse Myelitis Center
- Matthew Schniederjan, Emory University School of Medicine, Dept. of Pathology
- Nate Smith, Arkansas Dept. of Health
- Ken Tyler, University of Colorado School of Medicine, Chair, Dept. of Neurology
- Arun Venkatesan, Johns Hopkins University School of Medicine, Div. and Physical Medic of Neuroimmunology and Neuroinfectious Diseases
Slide 4
AFM Task Force – Activities Since December 2018 BSC Meeting
- January-March 2019: monthly conference calls
- Form AFM collaboration to
- Strengthen infrastructure for case identification and surveillance, including long-term follow-up of cases
- Facilitate research evaluations through case identification, data and specimen collection, and information sharing
- Immunology: approaches to determine if pathology is due to direct effect of virus or damage due to immune response to virus
- Host genetics and AFM
- Form AFM collaboration to
- April 2019: in-person meeting
- Reviewed ongoing research projects and other activities
- Prioritized virology and immunology research questions
- Defined key knowledge gaps in genetics and treatment, including rehabilitation
- Updated Task Force on the AFM natural history study (NIH)
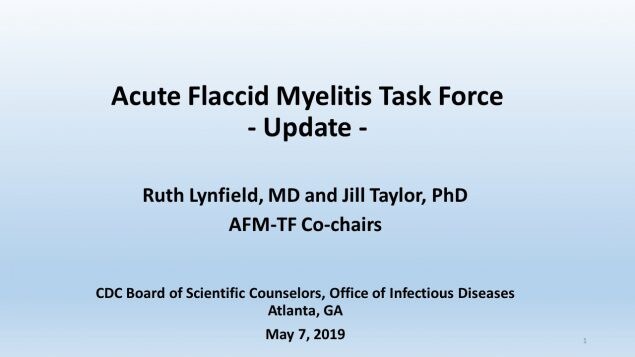
Enterovirus D68 Nucleotide Tree
In red: CDC confirmed AFM cases EV-D68 (respiratory specimens)
Slide 6
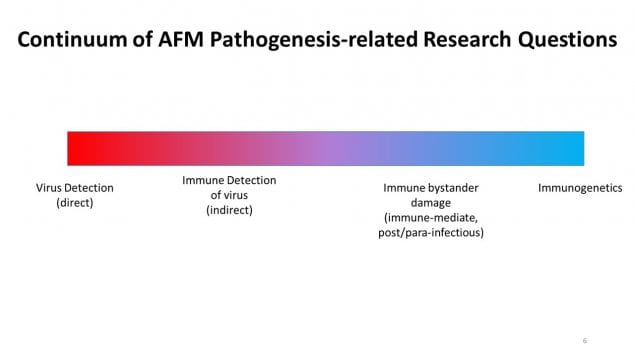
Continuum of AFM Pathogenesis-related Research Questions
[From left to right]
Virus Detection (direct), Immune Detection of Virus (indirect), Immune bystander damage (immune-mediate, post/para-infectious), Immunogenetics
Slide 7
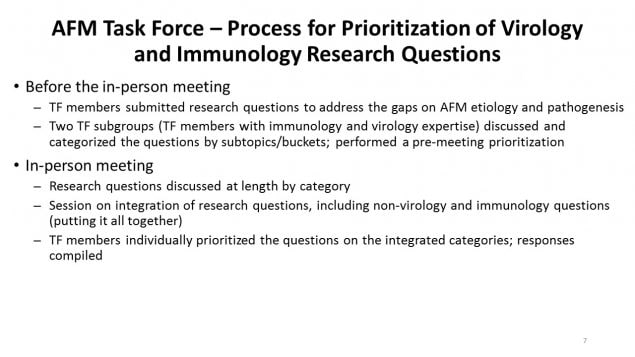
AFM Task Force – Process for Prioritization of Virology and Immunology Research Questions
- Before the in-person meeting
- TF members submitted research questions to address the gaps on AFM etiology and pathogenesis
- Two TF subgroups (TF members with immunology and virology expertise) discussed and categorized the questions by subtopics/buckets; performed a pre-meeting prioritization
- In-person meeting
- Research questions discussed at length by category
- Session on integration of research questions, including non-virology and immunology questions (putting it all together)
- TF members individually prioritized the questions on the integrated categories; responses compiled
Slide 8

AFM Task Force – Main Categories for Action and Research
- Communication and education
- Surveillance
- Diagnostic tool development
- Pathogenesis
- Risk factors studies
- Therapeutics and vaccines
- Treatment and rehabilitation
Slide 9

AFM Task Force – High Priority Activities by Category
Communication and education
- Communication and education efforts targeting health care providers, parents, and general public
Surveillance
- Robust, integrated case and viral surveillance
- Understand molecular epidemiology of EV-D68 strains
- Investigate temporal and geographic correlations of AFM cases with circulating viruses
Diagnostic tool development
- Detection of pathogen, host immune response
- Develop immunologic assays (e.g., EV-D68 IgM) in CSF and serum
- Detect exposure to infectious agents via the intrathecal antibody profile of AFM patients
Pathogenesis
- Determine viral molecular determinants of neurotropism, cell death, paralytic potential
- Use animal models to better understand viral pathogenesis
- Determine if there is evidence of autoimmunity
- Develop EV-D68 infectious clones
Slide 10
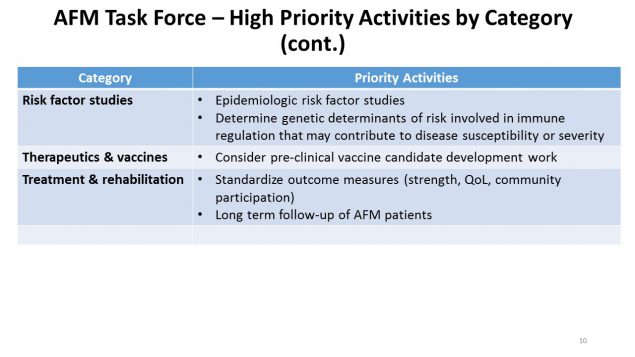
AFM Task Force – High Priority Activities by Category (continued)
Risk factor studies
- Epidemiologic risk factor studies
- Determine genetic determinants of risk involved in immune regulation that may contribute to disease susceptibility or severity
Therapeutics and vaccines
- Consider pre-clinical vaccine candidate development work
Treatment and rehabilitation
- Standardize outcome measures (strength, QoL, community participation)
- Long term follow-up of AFM patients
Slide 11
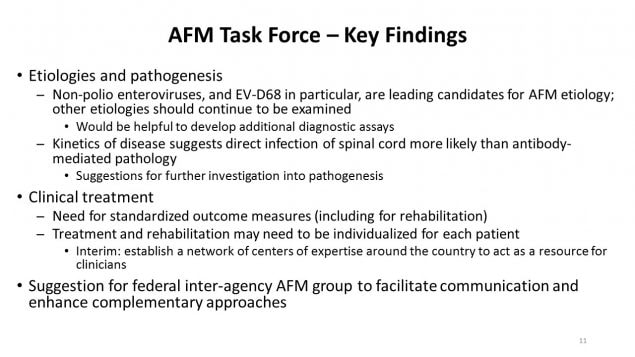
AFM Task Force – Key Findings
- Etiologies and pathogenesis
- Non-polio enteroviruses, and EV-D68 in particular, are leading candidates for AFM etiology; other etiologies should continue to be examined
- Would be helpful to develop additional diagnostic assays
- Kinetics of disease suggests direct infection of spinal cord more likely than antibody-mediated pathology
- Suggestions for further investigation into pathogenesis
- Non-polio enteroviruses, and EV-D68 in particular, are leading candidates for AFM etiology; other etiologies should continue to be examined
- Clinical treatment
- Need for standardized outcome measures (including for rehabilitation)
- Treatment and rehabilitation may need to be individualized for each patient
- Interim: establish a network of centers of expertise around the country to act as a resource for clinicians
- Suggestion for federal inter-agency AFM group to facilitate communication and enhance complementary approaches
Slide 12

Questions for BSC
- Do you agree with the main categories for action/research?
- Do you agree with the high priorities?
- Any other high priority areas for consideration?
- Suggestions for ways to ensure that clinicians recognize AFM and report to their health department?
- Other recommendations?
Slide 13
Acknowledgements
AFM Task Force Members, Mona Marin, Manisha Patel, Janell Routh, Adriana Lopez, Kathleen Dooling, Angela Guo, Amie Nisler, Jeanette St. Pierre, Tom Clark, Steve Oberste, Mark Pallansch, William Weldon, Jennifer Anstadt, Allan Nix, Nancy Messonnier