Model Performance Evaluation Program Report of Results: August 2022
MPEP August 2022 [PDF – 819 KB]
The purpose of this report is to present results of the U.S. Centers for Disease Control and Prevention (CDC) Model Performance Evaluation Program (MPEP) for Mycobacterium tuberculosis complex (MTBC) drug susceptibility testing survey sent to participants in August 2022.
Primary Classification
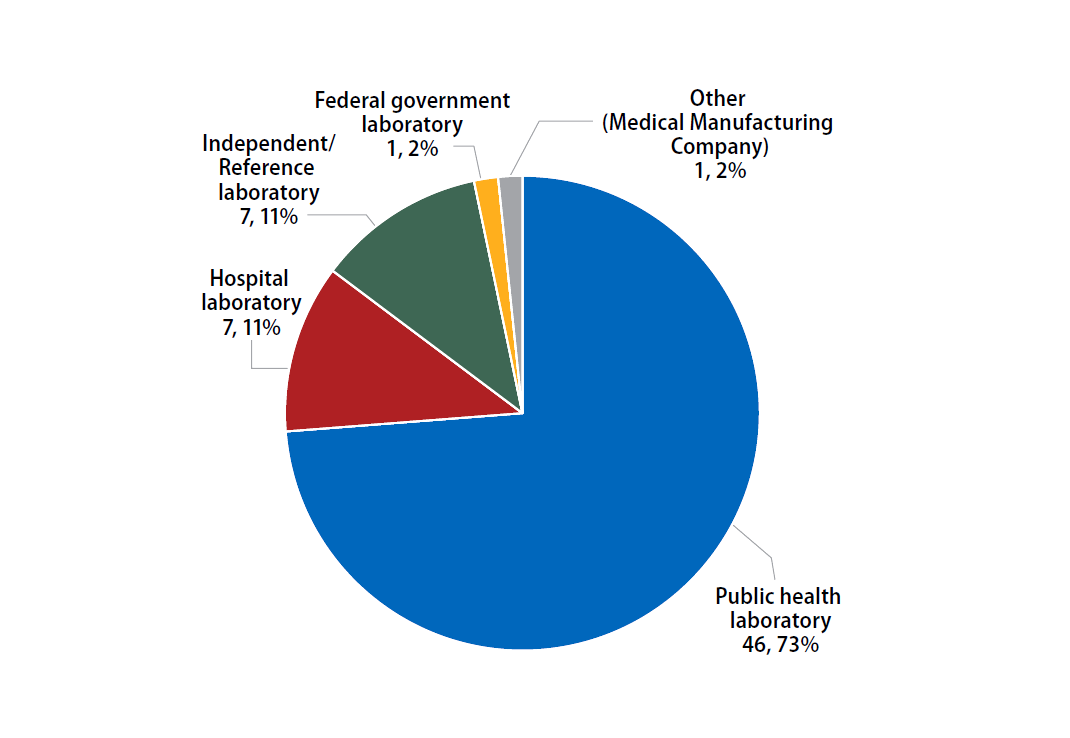
This report contains DST results submitted to CDC by survey participants at 61 laboratories in 32 states.
The participants were asked to indicate the primary classification of their laboratory (Figure 1).
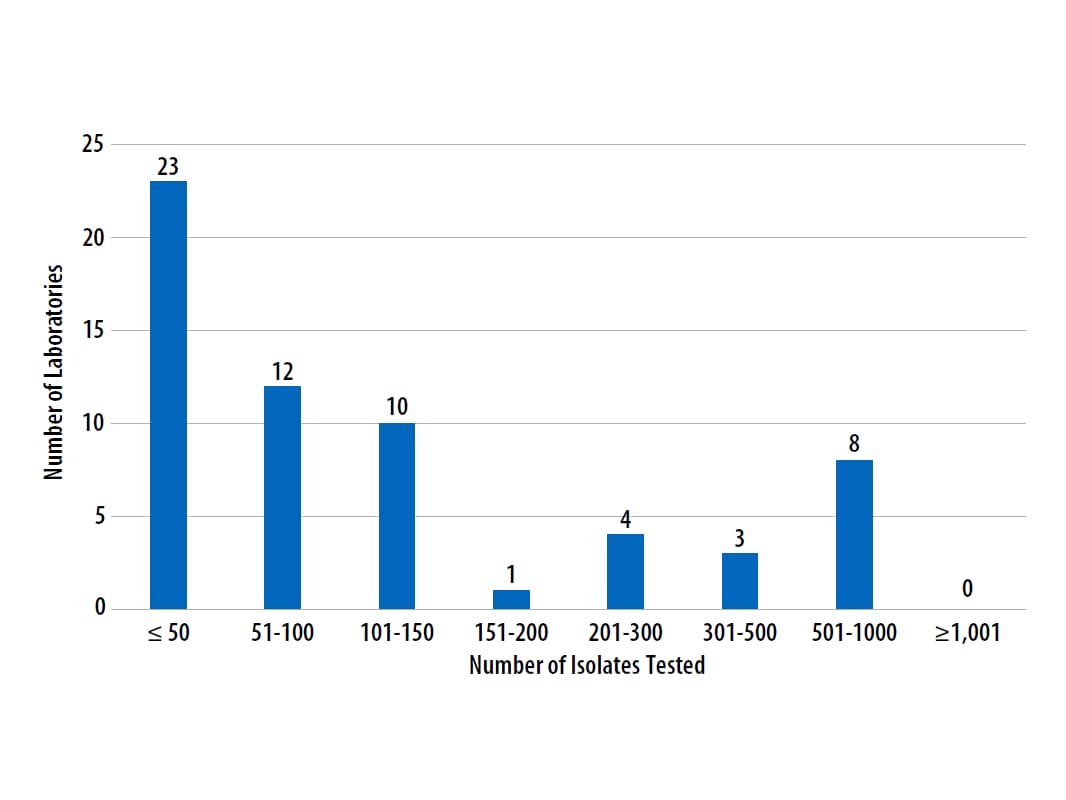
Annual Number of MTBC Drug Susceptibility Tests Performed
The number of MTBC isolates tested for drug susceptibility by the 61 participants in 2021 (excluding isolates used for quality control) is shown in Figure 2. In 2021, the counts ranged from 0 to 860 tests. Participants at 23 (38%) laboratories reported testing 50 or fewer DST isolates per year. Laboratories with low MTBC DST volumes are encouraged to consider referral of testing because of concerns about maintaining proficiency [9].
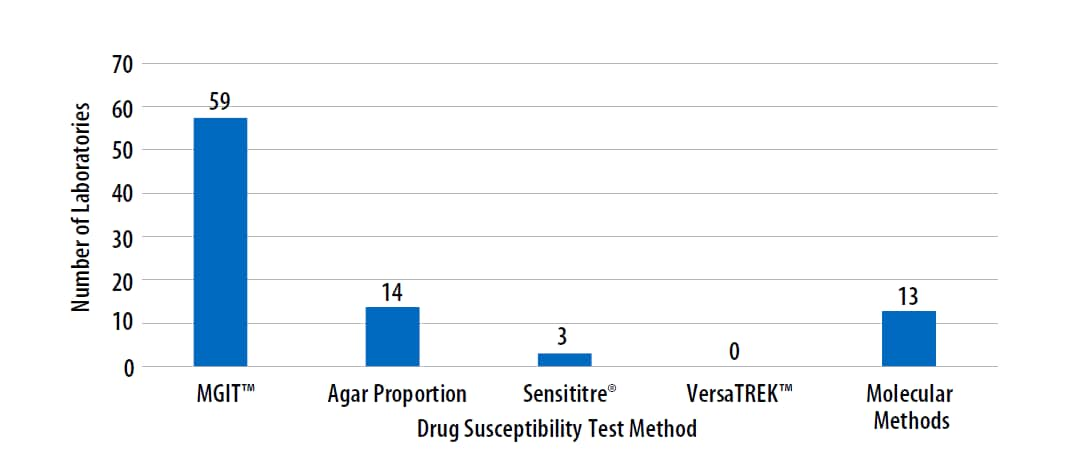
MTBC DST Methods Used by Participants
The DST methods that were performed by participating laboratories for this panel of MTBC isolates are displayed in Figure 3. Of participating laboratories, 39 (64%) reported results for only one method, 19 (31%) reported two methods, and 3 (5%) noted three susceptibility methods. Fifty-nine (66%) participating laboratories indicated use of MGIT.
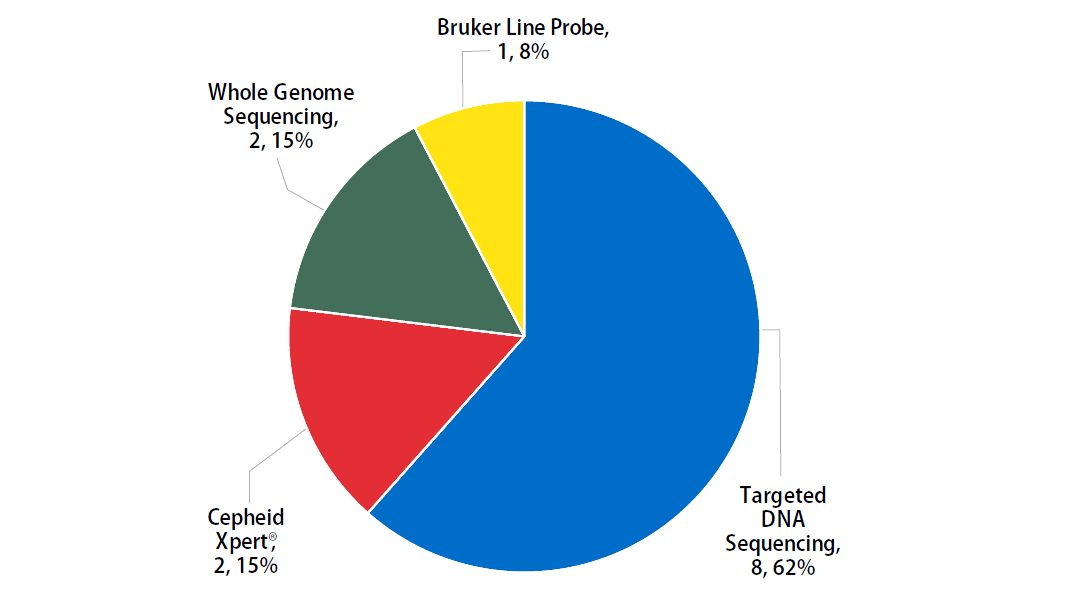
Molecular methods reported by participants are shown in Figure 4. The method performed most frequently (62%) was targeted DNA sequencing.
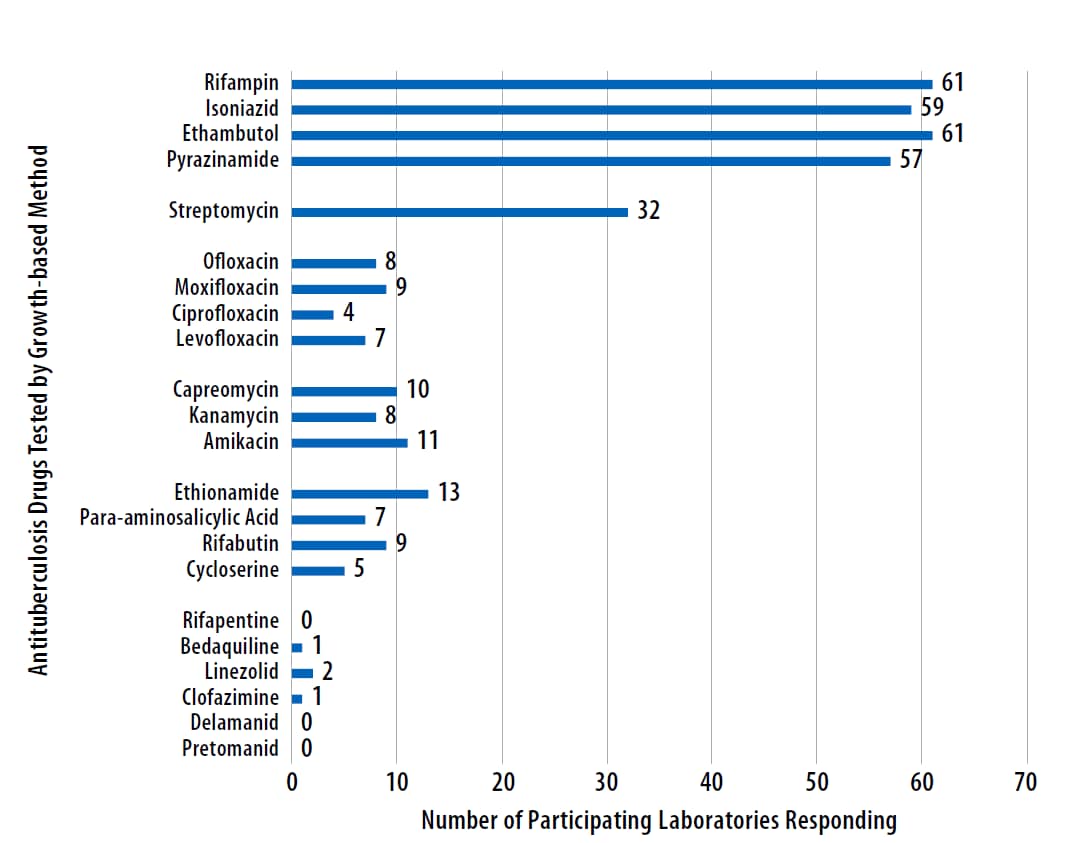
Antituberculosis Drugs Tested by Participants
The number of participating laboratories that reported testing each antituberculosis drug in the August 2022 survey is presented in Figure 5. CLSI recommends testing a full panel of first-line drugs (rifampin [RMP], isoniazid [INH], ethambutol [EMB], and pyrazinamide [PZA])[1] because it represents a combination of tests that provides the clinician with comprehensive information related to the 6- or 9-month four-drug RIPE TB treatment regimen used for many patients. Laboratories should consider the addition of fluoroquinolones to their testing panel as CDC recommends susceptibility testing for fluoroquinolones (e.g., moxifloxacin) with use of the alternate 4-month rifapentine-moxifloxacin treatment regimen; RMP may be used as a proxy for rifapentine [10].
CDC has adopted a new hybrid definition of XDR that includes both the former classification (i.e., MDR with resistance to second-line injectable plus fluoroquinolone) or the revised WHO definition (i.e., MDR plus resistance to fluoroquinolone and either bedaquiline or linezolid) [11, 12]. Eighteen laboratories reported second-line drug results other than streptomycin. Four (22%) of these laboratories tested all three second-line injectable drugs (amikacin, kanamycin, and capreomycin) and at least one fluoroquinolone (ofloxacin, ciprofloxacin, levofloxacin, or moxifloxacin) needed to confidently define the former classification of XDR TB. Two laboratories tested at least one fluoroquinolone and either bedaquiline or linezolid to define the WHO’s revised XDR TB definition.
Anticipated growth-based and molecular results for the panel of MTBC isolates sent to participants in August 2022 are shown in the tables below. Although CDC recommends broth-based methods for routine first-line DST of MTBC isolates, the results obtained by the reference agar proportion method (except for pyrazinamide, in which MGIT™ was performed) are shown in Table 1. Molecular results obtained by whole genome sequencing are listed in Table 2 [6].
Table 1. Expected Growth-based Results for February 2022 Survey
Note—S=susceptible, R=resistant
| Isolate | RMP | INH | EMB | PZA | Second-line Drugs Resistances: |
| 2022F | S | S | S | S | |
| 2022G | S | S | S | R* | |
| 2022H | S | S | S | S | |
| 2022I | S | R | S | S | ETA |
| 2022J | S | R | S | S |
*80% consensus for a single categorical result across all methods reported for this drug of either susceptible or resistant was not achieved for this isolate among participating laboratories.
Table 2. Expected Molecular Results (Mutations Detected in Loci Associated with Resistance) for August 2022 Survey
Note—Empty cell=No mutation detected
| Isolate | rpoB¥ | katG | inhA | pncA | ethA |
|---|---|---|---|---|---|
| 2022F | Phe433Phe* (Phe514Phe)† |
||||
| 2022G | His82Asp | ||||
| 2022H | Leu430Pro* (Leu511Pro)† |
||||
| 2022I | C-15T | ||||
| 2022J | Deletion | Ser266Arg§ |
¥Mutation is listed using both the M. tuberculosis and E.coli numbering system [7, 8]
*M. tuberculosis numbering system used
†E. coli numbering system used
§Mutation not associated with resistance
- CLSI, Susceptibility Testing of Mycobacteria, Nocardiae spp., and Other Aerobic Actinomycetes, in 3rd Ed. CLSI Standard M24. 2018, Clinical and Laboratory Standards Institute: Wayne, PA.
- CLSI, Performance Standards for Susceptibility Testing of Mycobacteria, Nocardia spp., and Other Aerobic Actinomycetes, in 1st Ed. CLSI supplement M62. 2018, Clinical and Laboratory Standards Institute: Wayne, PA.
- CLSI, Performance Standards for Susceptibility Testing of Mycobacteria, Nocardia spp., and Other Aerobic Actinomycetes, in 2nd edition. CLSI supplement M24S. 2023, Clinical and Laboratory Standards Institute: Wayne, PA.
- World Health Organization, Technical Report on critical concentrations for drug susceptibility testing of medicines used in the treatment of drug-resistant tuberculosis. 2018: Geneva.
- World Health Organization, Technical report on critical concentrations for drug susceptibility testing of isoniazid and the rifamycins (rifampicin, rifabutin and rifapentine). 2021, Geneva: World Health Organization.
- Campbell, P.J., et al., Molecular detection of mutations associated with first- and second-line drug resistance compared with conventional drug susceptibility testing of Mycobacterium tuberculosis. Antimicrob Agents Chemother, 2011. 55(5): p. 2032-41.
- Andre, E., et al., Consensus numbering system for the rifampicin resistance-associated rpoB gene mutations in pathogenic mycobacteria. Clin Microbiol Infect, 2017. 23(3): p. 167-172.
- APHL, Issues in Mycobacterium tuberculosis complex (MTBC) Drug Susceptibility Testing: Rifampin (RIF), in APHL Issues in Brief: Infectious Diseases. 2019, Association of Public Health Laboratories: Washington, D.C.
- APHL, TB Drug Susceptibility Testing Expert Panel Meeting Summary Report. 2007, Association of Public Health Laboratories: Washington, D.C.
- Carr W, K.E., Starks A, Goswami N, Allen L, Winston C., Interim Guidance: 4-Month Rifapentine-Moxifloxacin Regimen for the Treatment of Drug-Susceptible Pulmonary Tuberculosis — United States, 2022. MMWR Morb Mortal Wkly Rep, 2022(71): p. 285–289.
- World Health Organization, Meeting report of the WHO expert consultation on the definition of extensively drug-resistant tuberculosis, 27-29 October 2020. 2021, World Health Organization: Geneva.
- CDC Division of Tuberculosis Elimination, Dear Colleague Letter: Surveillance definitions for extensively drug resistant (XDR) and pre-XDR tuberculosis. 2022.
- Almeida Da Silva, P.E. and J.C. Palomino, Molecular basis and mechanisms of drug resistance in Mycobacterium tuberculosis: classical and new drugs. J Antimicrob Chemother, 2011. 66(7): p. 1417-30.
- Zhang, Y. and W.W. Yew, Mechanisms of drug resistance in Mycobacterium tuberculosis: update 2015. Int J Tuberc Lung Dis, 2015. 19(11): p. 1276-89.
- Centers for Disease Control and Prevention, Availability of an assay for detecting Mycobacterium tuberculosis, including rifampin-resistant strains, and considerations for its use – United States, 2013. MMWR Morb Mortal Wkly Rep, 2013. 62(41): p. 821-7.
- Van Deun, A., et al., Rifampin drug resistance tests for tuberculosis: challenging the gold standard. J Clin Microbiol, 2013. 51(8): p. 2633-40.
- Zhang, Y. and D. Mitchison, The curious characteristics of pyrazinamide: a review. Int J Tuberc Lung Dis, 2003. 7(1): p. 6-21.
- Ramirez-Busby, S.M. and F. Valafar, Systematic Review of Mutations in Pyrazinamidase Associated with Pyrazinamide Resistance in Mycobacterium tuberculosis Clinical Isolates. Antimicrob Agents Chemother, 2015. 59(9): p. 5267-77.
- Van Deun, A., et al., Mycobacterium tuberculosis strains with highly discordant rifampin susceptibility test results. J Clin Microbiol, 2009. 47(11): p. 3501-6.
- Rigouts, L., et al., Rifampin resistance missed in automated liquid culture system for Mycobacterium tuberculosis isolates with specific rpoB mutations. J Clin Microbiol, 2013. 51(8): p. 2641-5.
- World Health Organization, Catalogue of mutations in Mycobacterium tuberculosis complex and their association with drug resistance. 2021, World Health Organization: Geneva.
- Zhang, Y. and W.W. Yew, Mechanisms of drug resistance in Mycobacterium tuberculosis. Int J Tuberc Lung Dis, 2009. 13(11): p. 1320-30.
- Seifert, M., et al., Genetic mutations associated with isoniazid resistance in Mycobacterium tuberculosis: a systematic review. PLoS One, 2015. 10(3): p. e0119628.
- Kandler, J.L., et al., Validation of Novel Mycobacterium tuberculosis Isoniazid Resistance Mutations Not Detectable by Common Molecular Tests. Antimicrob Agents Chemother, 2018. 62(10).
- Ramaswamy, S.V., et al., Single nucleotide polymorphisms in genes associated with isoniazid resistance in Mycobacterium tuberculosis. Antimicrob Agents Chemother, 2003. 47(4): p. 1241-50.
- Ando, H., et al., A silent mutation in mabA confers isoniazid resistance on Mycobacterium tuberculosis. Mol Microbiol, 2014. 91(3): p. 538-47.
- Morlock, G.P., et al., ethA, inhA, and katG loci of ethionamide-resistant clinical Mycobacterium tuberculosis isolates. Antimicrob Agents Chemother, 2003. 47(12): p. 3799-805.
- Varma-Basil, M. and R. Prasad, Dilemmas with ethionamide susceptibility testing of Mycobacterium tuberculosis: A microbiologist & physician’s nightmare. Indian J Med Res, 2015. 142(5): p. 512-4.
- World Health Organization, Technical Report on critical concentrations for drug susceptibility testing of isoniazid and the rifamycins (rifampicin, rifabutin and rifapentine). 2021: Geneva.