ESBL-producing Enterobacterales in Healthcare Settings
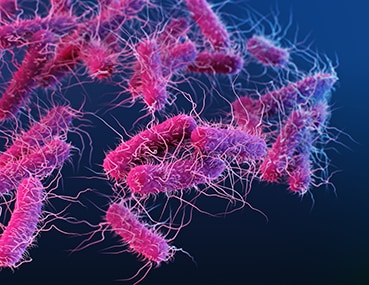
Enterobacterales are a large order of different types of bacteria (germs) that commonly cause infections both in healthcare settings and in communities. Examples of germs in the Enterobacterales order include Escherichia coli (E. coli) and Klebsiella pneumoniae.
To survive the effects of antibiotics, germs are constantly finding new defense strategies, called “resistance mechanisms.” For example, some Enterobacterales can produce enzymes called extended-spectrum beta-lactamases (ESBLs). ESBL enzymes break down and destroy some commonly used antibiotics, including penicillins and cephalosporins, and make these drugs ineffective for treating infections.
Learn about CRE
Carbapenem-resistant Enterobacterales (CRE)
This resistance means that there are fewer antibiotic options available to treat ESBL-producing Enterobacterales infections. In many cases, even common infections, such as urinary tract infections, caused by ESBL-producing germs require more complex treatments. Instead of taking oral antibiotics at home, patients with these infections might require hospitalization and intravenous (IV) carbapenem antibiotics.
See CDC’s report
Antibiotic Resistance Threats in the United States, 2019
Carbapenems are one of the few remaining antibiotics that can treat ESBL-producing germs, but resistance enzymes that destroy these antibiotics are on the rise, too. The more we rely on this important class of antibiotics, the greater the risk of spreading resistance to them.
How common are these infections?
In 2017, there were an estimated 197,400 cases of ESBL-producing Enterobacterales among hospitalized patients and 9,100 estimated deaths in the United States [Source: 2019 AR Threats Report].
Who is at risk?
These infections most commonly occur in people with exposure to healthcare, including those in hospitals and nursing homes. However, unlike many other resistant germs, ESBL-producing Enterobacterales can also cause infections in otherwise healthy people who have not been recently been in healthcare settings. In healthy people, this often means urinary tract infections.
ESBL germs have also been identified in people returning to the United States after traveling abroad, especially to places where these germs are more commonly found.
How are these germs spread?
In the United States, they can be spread from one person to another in healthcare settings through contaminated hands and surfaces. Outside the United States, they can be spread to people through contaminated food or water. The role of food and water in the spread of these germs in the United States is not clear.
How can you avoid getting an infection?
Keeping your hands clean is one of the most important steps you can take to avoid getting sick and spreading germs that can cause infections. Use soap and water or alcohol-based hand sanitizer.
ESBL-producing germs live in the gastrointestinal (GI) tract, so it is especially important to clean your hands after using the bathroom and before eating or preparing food. You should remind healthcare providers and other caregivers to clean their hands before they care for you and before they handle any medical devices. When traveling abroad, follow recommended practices for food and water safety.
How are these infections treated?
Infections caused by ESBL-producing germs are treated with antibiotics, but because they are resistant to many commonly prescribed antibiotics, treatment options might be limited. People with these infections sometimes need to be hospitalized for treatment with IV antibiotics. Carbapenem antibiotics, which are typically reserved for highly resistant infections, are often used to treat serious ESBL-producing Enterobacterales infections.
What is CDC doing to address these infections?
CDC and partners are working to assess and understand why infections caused by ESBL-producing Enterobacterales have increased since 2012.