Volume 10 — August 01, 2013
ORIGINAL RESEARCH
Sustained Improvement in Clinical Preventive Service Delivery Among Independent Primary Care Practices After Implementing Electronic Health Record Systems
Navigate This Article
Jason J. Wang, PhD; Kimberly M. Sebek, MPH; Colleen M. McCullough, BA; Sam J. Amirfar, MD; Amanda S. Parsons, MD, MBA; Jesse Singer, DO, MPH; Sarah C. Shih, MPH
Suggested citation for this article: Wang JJ, Sebek KM, McCullough CM, Amirfar SJ, Parsons AS, Singer J, et al. Sustained Improvement in Clinical Preventive Service Delivery Among Independent Primary Care Practices After Implementing Electronic Health Record Systems. Prev Chronic Dis 2013;10:120341. DOI: http://dx.doi.org/10.5888/pcd10.120341.
PEER REVIEWED
Abstract
Introduction
Studies showing sustained improvements in the delivery of clinical preventive services are limited. Fewer studies demonstrate sustained improvements among independent practices that are not affiliated with hospitals or integrated health systems. This study examines the continued improvement in clinical quality measures for a group of independent primary care practices using electronic health records (EHRs) and receiving technical support from a local public health agency.
Methods
We analyzed clinical quality measure performance data from a cohort of primary care practices that implemented an EHR at least 3 months before October 2009, the study baseline. We assessed trends for 4 key quality measures: antithrombotic therapy, blood pressure control, smoking cessation intervention, and hemoglobin A1c (HbA1c) testing based on monthly summary data transmitted by the practices.
Results
Of the 151 practices, 140 were small practices and 11 were community health centers; average time using an EHR was 13.7 months at baseline. From October 2009 through October 2011, average rates increased for antithrombotic therapy (from 58.4% to 74.8%), blood pressure control (from 55.3% to 64.1%), HbA1c testing (from 46.4% to 57.7%), and smoking cessation intervention (from 29.3% to 46.2%). All improvements were significant.
Conclusion
During 2 years, practices showed significant improvement in the delivery of several key clinical preventive services after implementing EHRs and receiving support services from a public health agency.
Introduction
Since the publication of a report by McGlynn et al (1), delivery rates of clinical preventive services are increasing, but slowly. The 2012 State of Health Care Quality report from the National Committee for Quality Assurance (NCQA) shows small improvements during the past 5 years in recommended preventive services for related cardiovascular measures, which have increased from 1 to 2 percentage points per year (2). Efforts to drive improvements include the use of health information technology (health IT), transformation of primary care practices into patient-centered medical homes, and payment reform (3–9).
Although several of these initiatives have yielded financial and clinical benefits, most have been demonstrated in closed, integrated delivery systems (10,11). Demonstrations in smaller independent settings have yet to produce consistent evidence that improving the quality of care is possible, which is disconcerting given that most ambulatory office visits in the United States still occur in practices operating with fewer than 10 physicians (12). Concerns continue that small independent practices are less likely to have programs to leverage advanced information systems for improving care coordination and disease management, potentially reducing hospitalizations or emergency department visits (12–15). Furthermore, small practices are unable to pool resources as larger integrated systems do to support their delivery infrastructure and dedicate nonphysician staff to help act on missed preventive services, because these require significant financial investments (16). Small practices also lag behind large practices in the adoption of health IT systems, and this gap continues to widen (17).
In expanding the public health role with primary care, the New York City Department of Health and Mental Hygiene (NYC DOHMH) created a new bureau, the Primary Care Information Project (PCIP), whose mission is to improve the delivery of clinical preventive services through the use of data-driven approaches for improving population health (18). Supported through a mix of federal, state, city, and private funding, PCIP has assisted 3,000 primary care providers at more than 500 independent practices to adopt electronic health record (EHR) systems and guided practices in transformation activities and participation in incentive programs (18). Collectively, these providers represent approximately 25% of New York City’s primary care providers and serve more than 2.6 million patients. Practices participating with PCIP are given tools to track and trend their panel of patients’ health across the city’s health agenda, Take Care New York (TCNY) (19), which includes 10 areas of actionable recommendations for patients, health care providers, and community partners. This study describes 2-year trends in performance of 4 key clinical quality measures, a subset of the 10 areas of health recommended by TCNY in which improvement in these measures has the highest potential for reducing preventable death in New York City and in the United States (20).
Methods
Practices were included if they adopted the PCIP subsidized eClinicalWorks EHR system at least 3 months before the baseline data analysis period (October 2009). Practices were excluded if data were not transmitted at any of the 3 data analysis periods: October 2009 (T1), October 2010 (T2), and October 2011 (T3). Community health centers (CHCs) were defined as any PCIP practice that was either a federally qualified health center, a New York State-defined diagnosis and treatment center, or had unusual special needs such as serving a foster care, mentally disabled, or other special population. All other practices were classified as small practices (SPs).
Data shown in the analysis were derived from practice EHRs that automatically transmit quality measurement data monthly to PCIP. From these transmissions, averages of practice performance data were assembled from October 2009 through October 2011. Four key quality measures of relevance to the TCNY agenda were included in the analytical data set: antithrombotic therapy among patients aged 18 years or older with ischemic vascular disease or aged 40 years or older with diabetes; blood pressure (BP) control among patients aged 18 to 75 years with essential hypertension and no diagnosis of ischemic vascular disease or diabetes; hemoglobin A1c (HbA1c) testing in the past 6 months among patients aged 18 to 75 years with diabetes; and smoking cessation intervention in the past 12 months among patients aged 18 years or older who were “current smokers” (Table 1). These measures are similar to National Quality Forum endorsed measures (no. 0631 [antithrombotic therapy], no. 0018 [BP control], no. 0057 [HbA1c testing], and no. 0028 [smoking cessation intervention]) (21), with the exception of age ranges and the fact that patients must have had at least 1 office visit with the primary care practice to be eligible. No other rules were applied for patient inclusion to the denominator. Additional practice and provider variables included number of encounters and number of unique patients seen per month, practice location, number of providers, number of practice sites, and practice-reported percentage of patients on Medicaid or self-insured. Practice date of EHR implementation was obtained from a customer relationship management database maintained by PCIP staff.
All statistical analyses were conducted using SAS version 9.2 (22). Comparisons between groups of practices, time points, or trends were considered significant if the observed P value for a statistical test was less than .05. Practice characteristics were measured at the baseline period (October 2009). Chi-square tests, t tests and nonparametric tests were used to compare characteristics between SPs and CHCs.
Trend graphs were generated for each quality measure over time and show average monthly practice rates. Separately, a comparison of practice level performance rates on each of the 4 quality measures was conducted for 3 points: October 2009 (T1), October 2010 (T2), and October 2011 (T3); and by practice characteristics. Generalized estimating equation models with logistic link function were used to analyze the association between time and practice characteristics and performance on the selected quality measures.
Results
Of the 550 independent primary care practices assisted by PCIP with EHR implementation, 151 (140 SPs and 11 CHCs) met all of the inclusion criteria for this analysis; 309 practices were excluded because they had not been using their systems for 3 months by October 2009, and 90 additional practices were excluded because they did not transmit data for all 3 data analysis points. A comparison of practice characteristics between those included in this analysis (n = 151) and those not included (n = 399) did not show any differences, with the exception of time using EHR.
Practices included in the trend analysis had an average of 925 encounters or 742 unique patients per month (Table 2). Practice characteristics, including patient distribution by borough, number of practice sites, and the length of time using an EHR system, were similar between SP and CHC groups. SPs differed from CHCs by number of providers the practice employed (2.6 vs 29.3, P = .03) and practice-reported percentage (20% or higher) of Medicaid or self-insured patients seen by the practice (29.3% vs 81.8%, P < .001).
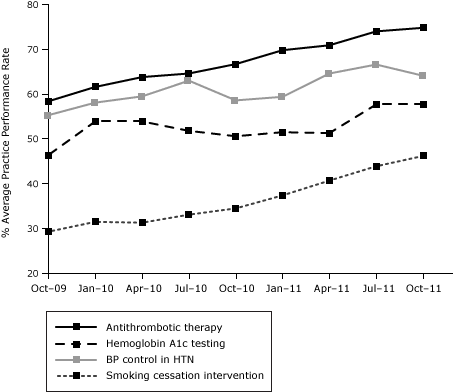
During the 2-year period, practice performance on all 4 quality measures exhibited an upward trend (Figure). Rates increased for antithrombotic therapy (58.4% to 74.8%, P < .001, standard deviation [SD] =19.7%), BP control (55.3% to 64.1%, P = .001, SD = 16.9%), HbA1c testing (46.4% to 57.7%, P = .007, SD = 29.6%), and smoking cessation intervention (29.3% to 46.2%, P < .001, SD = 27.1%). All improvements between baseline and T3 were significant. Improvements were higher in the second time interval (T3 vs T2) than in the first (T2 vs T1) for blood pressure control, HbA1c testing, and smoking cessation intervention.
Figure. Trend of individual quality measures over 3 periods: October 2009 (T1), October 2010 (T2), and October 2011 (T3). [A tabular version of this figure is also available.]
Improvement was consistently observed on all measures across practices over time. Practice characteristics, such as organization type and number of providers, were generally not associated with performance at each time point across the 4 measures. Time using the EHR (measured as months since EHR implementation) was the only factor consistently associated with improved performance, a finding that was also confirmed by a multivariate model adjusted for various practice characteristics: antithrombotic therapy (odds ratio [OR] = 1.03; 95% confidence interval [CI], 1.02–1.04); BP control (OR = 1.006; 95% CI, 1.00–1.01); HbA1c testing (OR = 1.03; 95% CI, 1.01–1.04); and smoking cessation intervention (OR = 1.04; 95% CI, 1.02–1.05) (Table 3). Practices with higher rates of self-reported Medicaid/uninsured populations achieved more significant improvement for smoking cessation intervention (OR = 1.78; 95% CI, 1.13–2.82)] than practices serving smaller Medicaid populations.
Discussion
Two-year trends of 151 independent practices showed significant gains on 4 key quality measures: antithrombotic therapy, BP control, HbA1c testing, and smoking cessation intervention. Our findings suggest that independent SPs and CHCs, with assistance from a community EHR extension program such as PCIP, can achieve clinical quality gains similar to those observed in larger, well-resourced integrated delivery systems (2). Our findings are relevant to independent practices serving resource-challenged urban areas.
Several reports in the literature indicated that practice size is associated with higher quality of care (23,24), so we also conducted analyses to ascertain whether the level of improvement differed across practice characteristics, such as whether CHCs experienced greater improvements than SPs. Of the practice characteristics we analyzed, none accounted for consistent differences in the increases observed with the exception of duration using an EHR.
Previous reports from this population suggest that short-term improvements are possible (25,26); in this study, we observed increases of several percentage points per year, suggesting that long-term improvement can also occur. This continued progress supports the idea that urban independent practices can drive long-term improvements in population health, a finding that is promising for inner-city independent practices like those served by PCIP, because they see an above-average number of patients who are uninsured and who have more severe health issues (17). At the same time, policy makers or stakeholders looking for instant quality gains should be cautious to expect early returns post-EHR implementation, because the larger increases in improvement were seen in the latter time period — between October 2010 and 2011 — when practices had been using the EHR for 25 months or more.
Our study has limitations. It was limited to the 151 practices where we received consistent quality measurement data over the 2-year period and therefore did not include all practices that joined PCIP and received similar support. Practices included in the study were generally earlier adopters of EHR, and we could not infer whether the performance trend would be similar or dissimilar to that of practices who were later adopters. We did not include specialties or other facilities that may interact with patients.
Providers working with PCIP represent a group of EHR users who have received varied assistance from PCIP staff, including training and guidance on quality improvement strategies, technical support on EHR software (upgrades, patches, and configuration), and connection for health information exchange. This type of support has been shown to positively affect the transition to an EHR system (27,28). A separate study using claims-based data suggests that improvement on quality measures can be achieved for practices that have used technical assistance (29). By the end of the analysis period in 2011, practices had been exposed to several environmental changes that were not measured or tested in this study. These include the introduction of the Centers for Medicaid and Medicare Services Meaningful Use incentives, New York State Medicaid incentives for practices achieving recognition for patient-centered medical homes, and monthly dashboards from PCIP for trending performance on selected EHR use and quality measures. Whether the introduction of these programs had an affect on the observed quality trends is unknown.
Improvement resulting from better documentation alone in the EHR was not tested in this study. However, we are aware that documentation and work-flow variability can result in underreporting of practice performance for some measures and not others (30). For example, HbA1c testing in patients with diabetes requires laboratory values to be returned through an electronic interface or manually entered into the patient’s record by the provider or practice staff. Practice rates on laboratory tests in which an electronic laboratory interface was not available and the practice does not routinely enter results into the patient’s record will be underreported, because EHR quality measurement programming will not detect information in scanned documents or faxes. Smoking cessation intervention is subject to appropriate documentation of counseling or prescription of smoking cessation aids; providers may not have instituted appropriate workflows to capture counseling conversations in the appropriate section of the EHR, thus underreporting the delivery of cessation intervention. In the example of antithrombotic therapy, gains in performance may be explained by improved documentation of over-the-counter medications (eg, aspirin) while continued trends represent better attention to this preventive service.
Broad adoption of EHR systems, along with technological advances and more experience with measurement using data from electronic records, may further drive improvements in primary care. However, it is promising to note that in our study, performance among independent practices was similar to or in some cases, exceeded, that of larger integrated systems. For instance, in 2011, PCIP averaged 64% on the BP control measure. For that measure in the same year, NCQA reported that nationally, commercial health maintenance organizations were averaging 65% and commercial and Medicare PPOs and Medicaid HMOs were averaging 58% to 60% (2). Both providers and policy makers should be encouraged by this indicator that independent primary care physicians can keep pace with their peers who work in integrated systems and can continue to improve, post-EHR adoption.
In our experience, the amount of support providers need to realize quality gains varies widely. Practices may require anywhere from 2 to 10 onsite visits in a year from a midlevel clinical quality specialist (29). These resources could be further sustained through local programs or through stakeholder support, such as payers or employer-based initiatives. Continued federal incentives and new payment models from Centers for Medicare and Medicaid Services may help stimulate independent primary care practices to get the most from health IT as an investment to improve health care and focus on patient-centered, outcomes-driven care and coordination.
Acknowledgments
We acknowledge Dr Thomas Farley, Commissioner of the New York City Department of Health, and Tiffany Harris and Carolyn Greene from the Bureau of Epidemiologic Services, for their valuable input on this manuscript. We also thank the PCIP staff for their tremendous dedication and participating practices’ commitment to improving health in New York City. A portion of this study was supported by the Agency for Healthcare Research and Quality (grant nos. R18HS17059 and 17294). The funder played no role in the study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
Author Information
Corresponding Author: Jason Wang, PhD, New York City Department of Health and Mental Hygiene, Primary Care Information Project, 42-09 28th St, 12th Fl, Queens, NY 11101. Telephone: 347-396-4859. E-mail: jwang5@health.nyc.gov.
Author Affiliations: Kimberly M. Sebek, Colleen M. McCullough, Sam C. Amirfar, Amanda S. Parsons, Jesse Singer, Sarah C. Shih, New York City Department of Health and Mental Hygiene, Primary Care Information Project, Queens, New York.
References
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348(26):2635–45. CrossRef PubMed
- The National Committee for Quality Assurance. The state of healthcare quality 2012: focus on obesity and Medicare plan improvement; 2012. http://www.ncqa.org/Portals/0/State%20of%20Health%20Care/2012/SOHC%20Report%20Web.pdf. Accessed March 13, 2013.
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144(10):742–52. CrossRef PubMed
- Jain A, Hayden S. Using electronic health records to collect patient-specific performance measures and outcomes. AMIA Annu Symp Proc 2008;6:1242–3. PubMed
- Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academy Press; 2001.
- Congressional Budget Office. Evidence on the costs and benefits of health information technology; 2008. http://www.cbo.gov/ftpdocs/91xx/doc9168/05-20-HealthIT.pdf. Accessed August 21, 2012.
- Takach M. Reinventing Medicaid: state innovations to qualify and pay for patient-centered medical homes show promising results. Health Aff (Millwood) 2011;30(7):1325–34. CrossRef PubMed
- Case study — developing an electronic prescribing incentive program: lessons learned from New York Medicaid (AHRQ publication no. 10-0096-EF). Rockville (MD): Agency for Healthcare Research and Quality; 2010.
- Goroll AH, Schoenbaum SC. Payment reform for primary care within the accountable care organization: a critical issue for health system reform. JAMA 2012;308(6):577–8. CrossRef PubMed
- Ballard DJ, Nicewander DA, Qin H, Fullerton C, Winter FD Jr, Couch CE. Improving delivery of clinical preventive services: a multi-year journey. Am J Prev Med 2007;33(6):492–7. CrossRef PubMed
- Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med 2011;365(9):825–33. CrossRef PubMed
- Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2004 summary. Adv Data 2006;(374):1–33. PubMed
- Reschovsky JD, O'Malley AS. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Aff (Millwood) 2008;27(3):w222–31. CrossRef PubMed
- Bach PB. Racial disparities and site of care. Ethn Dis 2005;15(2, Suppl 2):S31–3. PubMed
- Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med 2004;351(6):575–84. CrossRef PubMed
- Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care; 2002. http://www.nap.edu/catalog.php?record_id=10260. Accessed March 20, 2012.
- Decker SL, Jamoom EW, Sisk JE. Physicians in nonprimary care and small practices and those age 55 and older lag in adopting electronic health record systems. Health Aff (Millwood) 2012;31(5):1108–14. CrossRef PubMed
- Mostashari F, Tripathi M, Kendall M. A tale of two large community electronic health record extension projects. Health Aff (Millwood) 2009;28(2):345–56. CrossRef PubMed
- Take care New York: a policy for a healthier New York City: fourth year progress report. New York City Department of Health and Mental Hygiene; 2009. http://www.nyc.gov/html/doh/downloads/pdf/tcny/tcny-4yr-ar.pdf. Accessed March 26, 2012.
- Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in use of clinical preventive services. Am J Prev Med 2010;38(6):600–9. CrossRef PubMed
- National Quality Forum website. http://www.qualityforum.org/QPS/. Accessed March 19, 2013.
- SAS Software version 9.2, Copyright 2002-2008. Cary (NC): SAS Institute Inc.
- Pham HH, Schrag D, Hargraves JL, Bach PB. Delivery of preventive services to older adults by primary care physicians. JAMA 2005;294(4):473–81. CrossRef PubMed
- Moon JH, Weiser R, Highsmith N, Somers SA. The relationship between practice size and quality of care in Medicaid. Hamilton (NJ): Center for Health Care Strategies, Inc; 2009.
- Shih SC, McCullough CM, Wang JJ, Singer J, Parsons AS. Health information systems in small practices. Improving the delivery of clinical preventive services. Am J Prev Med 2011;41(6):603–9. CrossRef PubMed
- De Leon SF, Shih SC. Tracking the delivery of prevention-oriented care among primary care providers who have adopted electronic health records. J Am Med Inform Assoc 2011;18(Suppl 1):i91–5. CrossRef PubMed
- Pan Q, Meng YX, Gibbons GH, Strayhorn G. Effectiveness of an intervention to improve the documentation required for diagnosis of metabolic syndrome in clinics serving African-American patients. Qual Prim Care 2009;17(3):191–6. PubMed
- Loo TS, Davis RB, Lipsitz LA, Irish J, Bates CK, Agarwal K, et al. Electronic medical record reminders and panel management to improve primary care of elderly patients. Arch Intern Med 2011;171(17):1552–8. CrossRef PubMed
- Ryan AM, Bishop TF, Shih S, Casalino LP. Small physician practices in New York needed sustained help to realize gains in quality from use of electronic health records. Health Aff (Millwood) 2013;32(1):53–62. CrossRef PubMed
- Parsons A, McCullough C, Wang J, Shih S. Validity of electronic health record-derived quality measurement for performance monitoring. J Am Med Inform Assoc 2012;19(4):604–9. CrossRef PubMed
Tables
 Table 1. Description of Quality Measures, New York City Primary Care Practices (N = 151)
Table 1. Description of Quality Measures, New York City Primary Care Practices (N = 151)
| Measure | Eligible Patient (Denominator) | Patient Goal (Numerator) |
|---|---|---|
| HbA1c testing | Patients aged 18 to 75 years with diabetes | HbA1c test recorded in the past 6 months |
| Antithrombotic therapy | Patients aged 18 years or older with ischemic vascular disease or aged 40 years or older with diabetes | Taking antithrombotic/other antithrombotic therapy |
| Blood pressure control | Patients aged 18 to 75 years with hypertension and no diagnosis of ischemic vascular disease or diabetes | Systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg |
| Smoking cessation intervention | Patients aged 18 years or older with a “current smoker”a smoking status | Smoking cessation intervention (prescription or counseling) received in the past 12 months |
Abbreviation: HbA1c, hemoglobin A1c.
a A “current smoker” was identified through the most recent documented status located in a structured form in the electronic health record. Providers selected either “current smoker,” “former smoker,” or “never smoker.”
 Table 2. Practice Characteristics of Small Practices (SPs) and Community Health Centers (CHCs) at Baseline, New York City, October 2009
Table 2. Practice Characteristics of Small Practices (SPs) and Community Health Centers (CHCs) at Baseline, New York City, October 2009
| Characteristic | Mean Practice Value | ||
|---|---|---|---|
| All Practices (n = 151) | SPs (n = 140) | CHCs (n = 11) | |
| No. of sites | 1.4 | 1.2 | 3.1 |
| No. of providers | 4.5 | 2.6 | 29.3a |
| No. of encounters per month | 925 | 749 | 3,169 |
| No. of unique patients per month | 742 | 612 | 2,392 |
| % of Medicaid/self-insured ≥20 (practice-reported) | 33.1 | 29.3 | 81.8b |
| Months using EHR up to October 2009 | 13.7 | 13.8 | 13.0 |
| Bronx | 12.6 | 12.9 | 9.1 |
| Brooklyn | 33.1 | 34.3 | 18.2 |
| Manhattan | 31.1 | 29.3 | 54.6 |
| Queens | 18.5 | 18.6 | 18.2 |
| Staten Island | 4.6 | 5 | 0 |
Abbreviation: EHR, electronic health record.
a P = .03
b P < .001.
 Table 3. Association Between EHR Use and Practice Characteristics and Performance, by Quality Measure, New York City, 2009–2011
Table 3. Association Between EHR Use and Practice Characteristics and Performance, by Quality Measure, New York City, 2009–2011
| Practice Characteristics | Quality Measure | |||
|---|---|---|---|---|
| Antithrombotic Therapy | BP Control | HbA1c Testing | Smoking Cessation Intervention | |
| Odds Ratio (95% Confidence Interval) | ||||
| Months since implementing EHR | 1.03 (1.02–1.04) | 1.006 (1.00–1.01) | 1.03 (1.01–1.04) | 1.04 (1.02–1.05) |
| CHC | 0.84 (0.43–1.63) | 0.56 (0.38–0.81) | 1.13 (0.32–3.98) | 0.58 (0.28–1.20) |
| Months since EHR*CHCa | 1.003 (0.98–1.02) | 1.01 (1.002–1.02) | 1.02 (0.99–1.06) | 1.006 (0.96–1.05) |
| Medicaid/self-pay ≥20% | 1.21 (0.89–1.66) | 1.08 (0.89–1.31) | 1.21 (0.83–1.78) | 1.78 (1.13–2.82) |
| Practice has >1 provider | 1.24 (0.83–1.85) | 0.93 (0.76–1.13) | 1.12 (0.74–1.70) | 0.70 (0.45–1.08) |
Abbreviations: EHR, electronic health record; BP, blood pressure; HbA1c, hemoglobin A1c; EHR, electronic health record; CHC, community health center.
a Interaction between months since implementing an EHR and CHC status.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.