What to know
Pain can impact almost every aspect of your life, leading to limited physical functioning, poor mental health, and reduced quality of life. No matter the cause of your pain, it is important that you receive access to safe and effective pain management options and can communicate with your doctor to make informed decisions about what is right for you.

Pain relief should be safe and effective
Many people experience pain every day. All patients with pain should receive safe and effective pain care. The goal of any pain care strategy is to safely reduce pain and increase your ability to do everyday activities.
No matter what form of treatment is used, you can discuss with your doctor what kind of pain relief and improvement you can expect overall and continue to follow up with your doctor on your progress.
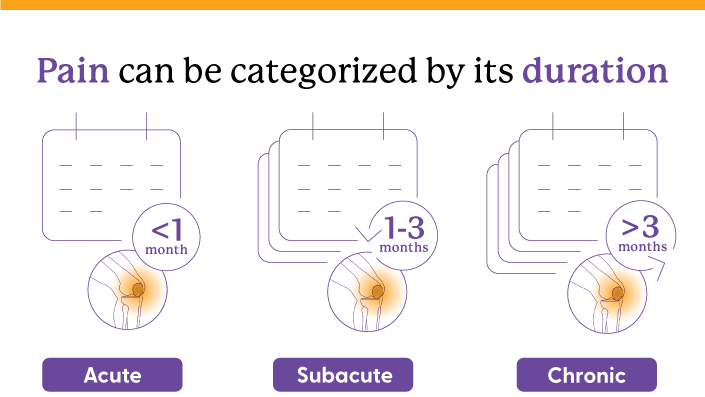
On this page, you’ll learn about the types of pain – acute, subacute, and chronic – and options for treatment.
What are prescription opioids?
Opioids are natural or synthetic chemicals that bind to receptors in your brain or body to reduce the intensity of pain signals reaching the brain. Doctors sometimes prescribe opioid medications to manage pain. Prescription opioid drugs include:
- Hydrocodone
- Oxycodone
- Morphine
Find Help and Treatment
Acute and subacute pain management
Acute pain is pain that has lasted for less than a month and has a known cause, like an injury, trauma, surgery, or infection. You may have experienced acute pain from outpatient medical procedures, like a wisdom tooth extraction, or injuries, like a broken bone. Subacute pain is pain that lasts 1 to 3 months.
Painful acute and subacute conditions include:
- Low back pain
- Neck pain
- Broken bones
- Muscle sprains or strains
- Dental pain from infection, tooth extraction
- Pain due to kidney stones
- Acute episodic migraines
- Pain after surgery
Acute pain normally gets better as your body heals. Opioid medications are one of many ways to reduce severe acute pain, but many other options can provide relief with fewer side effects, including:
- Over-the-counter medications like acetaminophen (such as Tylenol®), ibuprofen (such as Advil®, Motrin®), and naproxen (such as Aleve®)
- Application of heat or ice
- Physical therapy, acupuncture, acupressure, massage, or spinal manipulation
- Transcutaneous electrical nerve stimulation (TENS)
- Exercise
It is important to note that continuing opioid therapy during the subacute time frame might represent the start of long-term opioid therapy. You can talk to your doctor about your treatment goals and the benefits and risks of different types of treatment for subacute pain.
Chronic pain management
Chronic pain is pain lasting more than three months. It can be caused by a disease or condition, injury, medical treatment, inflammation, or even an unknown reason. Many people experience chronic pain, which can lead to impaired physical functioning, poor mental health, reduced quality of life, and contributes to substantial disability and death each year.
There are many possible options to treat your chronic pain. It is important to understand all your options and the risks and benefits of each. You and your doctor should work together to establish treatment goals for pain and function in your daily life.
Chronic pain can be managed with or without prescription opioids, but many of the nonopioid options have been shown to work better with fewer side effects. Examples include:
- Over-the-counter medications like acetaminophen (Tylenol®), ibuprofen (Advil®, Motrin®), and naproxen (Aleve®)
- Physical therapy and exercise
- Cognitive behavioral therapy (CBT)
- Certain antidepressant and antiseizure medications
Making a pain management plan
Patient safety is an important part of pain care
Before starting opioids to treat pain, you can:
- Learn about prescription opioids and know the risks.
- Consider ways to manage pain that do not include opioids. Examples include:
- Physical therapy
- Exercise
- Nonopioid medications, such as acetaminophen or ibuprofen
- Cognitive behavioral therapy (CBT)
- Physical therapy
- Work together with you doctor to make informed decisions.
Talk to your doctor about what kind of pain care is right for you
If after talking to your doctor about your pain treatment, you are prescribed opioids, be sure to ask about the risks and benefits. To help ensure your treatment is safe and effective, your doctor may:
- Prescribe the lowest effective dose of immediate-release opioids
- Check your state's prescription drug monitoring program to check if you've been prescribed other controlled substances that can interact with opioids and increase your risk of overdose
- Test your urine for the presence of drugs during your therapy
- Offer naloxone, which can reverse an overdose
- Follow up within the first few days after you start a new opioid or a new dose
- Follow up at least every 3 months if you are on a stable dose to ensure benefits of opioids continue to outweigh risks

If you are prescribed opioids for pain management
- Follow up with your doctor within the first few days of starting your prescription to ensure opioids are helping.
- You should also discuss what kind of pain relief and improvement you can expect overall. Opioids can reduce pain in the short-term but will not likely relieve all your pain.
- Also discuss any side-effects you are experiencing.
- You should also discuss what kind of pain relief and improvement you can expect overall. Opioids can reduce pain in the short-term but will not likely relieve all your pain.
- Develop your personal pain management plan with your doctor which may include:
- Your personal treatment goals, which describe what you may achieve as you make progress
- Information about treatment options
- Referral to specialists as needed
- Your personal treatment goals, which describe what you may achieve as you make progress
Side Effects of Opioid Therapy
Prescription opioids carry serious risks of opioid use disorder and overdose. Opioids can slow a person's breathing, often a sign associated with someone experiencing an opioid overdose that can cause death. The use of prescription opioids can have several side effects as well, even when taken as directed:1
- Tolerance—meaning you might need to take more of a medication for the same pain relief
- Physical dependence—meaning you have symptoms of withdrawal when a medication is stopped, or you take less
- Increased sensitivity to pain
- Constipation
- Nausea and vomiting
- Dry mouth
- Sleepiness
- Dizziness
- Confusion
- Low levels of testosterone that can result in lower sex drive, energy, and strength
- Itching
To learn more about risks of opioids and how to reduce them:
Nonopioid Therapies for Pain Management
- Benyamin R, Trescot AM, Datta S, Buenaventura RM, Adlaka R, Sehgal N, Glaser SE, Vallejo R. Opioid complications and side effects. Pain physician. 2008;11(2S):S105.


