Increase in Reported Prevalence of Microcephaly in Infants Born to Women Living in Areas with Confirmed Zika Virus Transmission During the First Trimester of Pregnancy — Brazil, 2015
Weekly / March 11, 2016 / 65(9);242–247
On March 8, 2016, this report was posted online as an MMWR Early Release.
Wanderson Kleber de Oliveira, MSc1; Juan Cortez-Escalante, MD2; Wanessa Tenório Gonçalves Holanda De Oliveira, MSc1; Greice Madeleine Ikeda do Carmo, MSc1; Cláudio Maierovitch Pessanha Henriques, MD1; Giovanini Evelim Coelho, PhD1; Giovanny Vinícius Araújo de França, PhD1 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
An outbreak of Zika virus disease, caused by a flavivirus transmitted by Aedes mosquitoes, occurred in Brazil in early 2015. An increase in the prevalence of infants born with microcephaly has been reported in Brazil since October 2015, in association with clusters of febrile rash illness in pregnant women.
What is added by this report?
The birth prevalence of microcephaly in Brazil increased sharply during 2015–2016. The largest increase occurred in the Northeast region, where Zika virus transmission was first reported in Brazil. This analysis of 574 cases of microcephaly, detected through a newly established ad hoc microcephaly surveillance system, identified temporal and geospatial evidence linking the occurrence of febrile rash illness consistent with Zika virus disease during the first trimester of pregnancy with the increased birth prevalence of microcephaly. The prevalence of microcephaly in 15 states with laboratory-confirmed Zika virus transmission (2.8 cases per 10,000 live births) significantly exceeded that in four states without confirmed Zika virus transmission (0.6 per 10,000).
What are the implications for public health practice?
The suggested link between maternal exposure to Zika virus infection during the first trimester of pregnancy and the increased birth prevalence of microcephaly provide additional evidence for congenital infection with Zika virus. Ongoing surveillance is needed to identify additional cases and to fully elucidate the clinical spectrum of illness. Pregnant women should protect themselves from mosquito bites by wearing protective clothing, applying insect repellents, and when indoors, ensuring that rooms are protected with screens or mosquito nets.
Altmetric:
Widespread transmission of Zika virus by Aedes mosquitoes has been recognized in Brazil since late 2014, and in October 2015, an increase in the number of reported cases of microcephaly was reported to the Brazil Ministry of Health.* By January 2016, a total of 3,530 suspected microcephaly cases had been reported, many of which occurred in infants born to women who lived in or had visited areas where Zika virus transmission was occurring. Microcephaly surveillance was enhanced in late 2015 by implementing a more sensitive case definition. Based on the peak number of reported cases of microcephaly, and assuming an average estimated pregnancy duration of 38 weeks in Brazil (1), the first trimester of pregnancy coincided with reports of cases of febrile rash illness compatible with Zika virus disease in pregnant women in Bahia, Paraíba, and Pernambuco states, supporting an association between Zika virus infection during early pregnancy and the occurrence of microcephaly. Pregnant women in areas where Zika virus transmission is occurring should take steps to avoid mosquito bites. Additional studies are needed to further elucidate the relationship between Zika virus infection in pregnancy and microcephaly.
Since late 2014, clusters of febrile rash illness have been reported from the Northeast region of Brazil (2,3). These cases were attributed to Zika virus, a flavivirus transmitted by Aedes mosquitoes, when the first cases confirmed by reverse transcription–polymerase chain reaction (RT-PCR) were reported in Bahia and Rio Grande do Norte states in April 2015 (4,5). As of January 2016, transmission had been confirmed in 22 of Brazil’s 26 states and the federal district, and in all five regions of the country.†
In Brazil, all recognized congenital anomalies are registered in the Live Birth Information System (Sistema de Informações sobre Nascidos Vivos [SINASC]), which collects information on all live births nationwide and is estimated to have >95% coverage. In SINASC, microcephaly is defined as a head circumference ≥3 standard deviations (SDs) below the mean for age and sex.§ According to the World Health Organization (WHO) Multicenter Growth Reference Study, this corresponds to a head circumference of 30.3 cm for full-term females (gestational age = 259–293 days [approximately 37–42 weeks]) and 30.7 cm for full-term males during the first week of life (6).
During 2000–2014, an average of 157.3 (SD = 17.7) cases of microcephaly were registered in SINASC each year.¶ On October 22, 2015, the Secretary of Health of Pernambuco state (in the Northeast region) informed the Brazil Ministry of Health (MoH) of a marked increase in the number of infants born with microcephaly in the state, where 26 cases had been reported since August 2015.** By late October, the Northeast region states of Paraíba and Rio Grande do Norte also were reporting an increase in cases of microcephaly. On October 29, 2015, MoH reported the event to the Pan American Health Organization as a potential Public Health Emergency of International Concern. On November 19, 2015, an ad hoc microcephaly surveillance system was established by MoH for identification of cases of microcephaly both prospectively, and through a retrospective review of hospital records going back to January 1, 2015. Initially, the case definition for the ad hoc system included all full-term infants with a head circumference ≤33 cm. Toward the end of 2015, the MoH defined microcephaly as a head circumference ≤32 cm in any full-term newborn; this case definition is currently used nationwide.
The MoH and Secretaries of Health from the affected states led a joint investigation to characterize and identify the etiology of the outbreak, with the support of national research institutes. This report presents temporal and geospatial evidence linking preceding Zika virus transmission with the increased prevalence of microcephaly in Brazil. Among Brazil’s 26 states and the federal capital district, the 19 jurisdictions that reported prospectively and retrospectively identified cases of microcephaly through the ad hoc microcephaly surveillance system during November 19, 2015–January 7, 2016 are included in this analysis. Two analyses were conducted. The first compared the number of cases of microcephaly identified through the ad hoc microcephaly surveillance system during January 1, 2015–January 7, 2016, with the mean number of cases reported to SINASC during 2000–2014 in those 19 jurisdictions, and compared the prevalence of microcephaly in states with documentation of laboratory-confirmed Zika virus transmission with the prevalence in states without confirmed Zika virus transmission. The second analysis examined the timing of peak occurrence of microcephaly cases in the three states with the highest reported prevalence of infants with microcephaly, relative to laboratory confirmation of Zika virus transmission in those states, to estimate the time during pregnancy when exposure to Zika virus might have occurred.
Because the SINASC case definition of microcephaly (head circumference ≥3 SDs below the mean for age and sex) was more restrictive than that of the ad hoc microcephaly surveillance system (≤32 cm in any full-term infant), the SINASC criteria were applied to cases reported to the ad hoc system for these analyses. Therefore, only cases reported to the ad hoc surveillance system with a head circumference ≥3 SDs below the mean for age and sex were included.
The annual mean number of cases of microcephaly among full-term newborns reported to SINASC during 2000–2014 was calculated and compared with the number of cases of microcephaly that occurred during January 1, 2015–January 7, 2016, and identified through the ad hoc microcephaly surveillance system. The excess number of microcephaly cases was calculated as the number of SDs above the mean number of cases reported during 2000–2014.†† Denominator data for estimation of state-level 2015 microcephaly birth prevalence were obtained by averaging the total number of live births from the SINASC 2009–2013 annual series (the most recent data available).§§ Exact binomial (F-inverse) 95% confidence intervals (CIs) for birth prevalence of microcephaly were calculated for states that did and did not report laboratory-confirmed Zika virus transmission. These two rates were compared with a Pearson’s chi-square test for heterogeneity.
To identify potential periods of maternal exposure to Zika virus during pregnancy, assuming an average gestation of 38 weeks (1), weekly counts of cases of microcephaly reported in 2015 in Bahia, Paraíba, and Pernambuco, the three states with the largest increases above the 2000–2014 mean, were reviewed. The beginning of the first trimester of pregnancy was estimated by counting back 38 weeks from the week during which the peak number of cases of microcephaly were reported in each of the three states. The earliest reports of laboratory confirmation of Zika virus transmission in the three states were used as a proxy for the beginning of Zika virus transmission. All statistical significance levels were set at p≤0.05.
A total of 574 cases of microcephaly that occurred during January 1, 2015–January 7, 2016, were prospectively and retrospectively identified and registered in the ad hoc microcephaly surveillance system from 19 states. Among these, 58.5% (336) were in females; this excess of female cases has been reported previously (7). The average head circumference of these infants was 29.0 cm (SD = 1.4 cm). During 2000–2014, the mean annual reported number of cases of microcephaly reported to SINASC was 157.3 (SD = 17.7), and by region, ranged from 13.0 in the Center-West to 65.2 in the Southeast (Table). During 2015–2016, 12 states reported microcephaly cases in excess of 3 SDs above the historical 2000–2014 average, including Bahia, Paraíba, and Pernambuco, each of which reported cases in excess of 20 SDs above the historical average (Figure 1).
During January 1, 2015–January 7, 2016, Zika virus transmission was laboratory-confirmed by real time quantitative RT-PCR in 15 of the 19 states included in this analysis; among these 15 states, the overall microcephaly birth prevalence was 2.80 (CI = 1.86–4.05) per 10,000 live births, compared with 0.60 (CI = 0.22–1.31) in the four states without laboratory-confirmed Zika virus transmission (p<0.001). The overall microcephaly birth prevalence in the 12 states reporting microcephaly cases >3 SDs above the historical 2000–2014 mean was 4.61 per 10,000 live births (CI = 4.19–5.05). The two states with the highest prevalence rates were Pernambuco (14.62; CI = 12.33–17.17) and Paraíba (10.82; CI = 8.86–13.04).
Pernambuco state reported the largest increase in number of reported cases of microcephaly. During epidemiologic weeks 18–39 (corresponding to mid-May–early October) 2015, Pernambuco reported 0–4 cases of microcephaly per week (Figure 2). The number of cases increased substantially during epidemiologic weeks 42–43 (late October), reaching a peak of 27 cases per week during epidemiologic week 46 (mid-November). Assuming an average full-term pregnancy of 38 weeks, the first trimester of pregnancy of mothers of infants with microcephaly born during epidemiologic week 46 occurred during epidemiologic weeks 8–20 (late February–mid May) of 2015. An outbreak of rash illness clinically compatible with Zika virus disease was reported in Pernambuco in December 2014, with laboratory confirmation of Zika virus disease in epidemiologic week 20 of 2015. The estimated first trimester of pregnancy of the mothers of the infants with microcephaly in Pernambuco coincided with occurrence of the rash illness outbreak.
Paraíba and Bahia states reported an abrupt increase in the number of infants born with microcephaly in epidemiologic weeks 45 and 47, respectively, and both states reported similar occurrences of a rash illness clinically compatible with Zika virus infection during May 2015 (Figure 2). In Bahia and Paraíba states, cases of microcephaly reported in infants born through epidemiologic week 42 in 2015 (when the first cases in Pernambuco were reported to MoH), were identified retrospectively through the ad hoc microcephaly surveillance system.
Discussion
Congenital anomalies, including microcephaly, have a complex and multifactorial etiology and can be caused by infections during pregnancy as well as chromosomal disorders, exposures to environmental toxins, and metabolic diseases.¶¶ The temporal relationship between outbreaks of Zika virus disease and increases in reported prevalence of microcephaly in Brazil, as well as the significant increase in birth prevalence of microcephaly in states with laboratory-confirmed Zika virus transmission, suggest a relationship between these two epidemiologic events. The reported occurrence of the 2015–2016 microcephaly cases, especially in Pernambuco, highlight the temporal relationship between preceding Zika virus transmission and the abrupt increase in birth prevalence of microcephaly.
This hypothesis is strengthened by recent virologic evidence. On November 17, 2015, the Flavivirus Laboratory of the Oswaldo Cruz Institute (Rio de Janeiro, Brazil) reported the detection of Zika virus RNA by real time RT-PCR in amniotic fluid samples collected from two pregnant women from Paraíba state whose fetuses were found to have microcephaly and cerebral calcifications by fetal ultrasound, and who reported symptoms compatible with Zika virus disease at 18 and 19 weeks’ gestational age.*** On November 18, 2015, the Evandro Chagas Institute (Pará, Brazil) reported that Zika virus RNA was identified in blood and tissue samples of a neonate with microcephaly who died shortly after birth.††† In addition, on January 12, 2016, MoH reported RT-PCR–confirmed Zika virus infection in two stillborn infants with central nervous system malformations and two neonates with microcephaly who died during the first hours of life, as determined by investigation by the Federal University of Rio Grande do Norte (Natal, Brazil), in collaboration with CDC.
The findings in this report are subject to at least four limitations. First, this is an ecologic analysis, with only limited laboratory evidence of Zika virus infection for the pregnancy outcomes described. Second, data were obtained from an ad hoc surveillance system established by MoH after the first cases possibly linked to maternal Zika virus disease were identified. The enhanced awareness regarding this event might have resulted in an increased ascertainment and reporting of cases, including identification of false positives. Third, microcephaly was probably underascertained in Brazil before this event, so the increases might not be as large as suggested by these findings; however, they are substantial increases compared with cases of microcephaly reported during 2000–2014, and in some states, such as Paraíba and Pernambuco, exceed the rate of 5.1 per 10,000 births in Brazil during 1995–2008, estimated by the Latin American Collaborative Study of Congenital Malformations (8). Finally, this study was limited to analysis of the temporal and geospatial association between the increased prevalence of microcephaly in Brazil and earlier Zika virus transmission, and other possible causes of microcephaly were not evaluated in this analysis.
The sudden and marked increase in birth prevalence of microcephaly in multiple states in Brazil temporally associated with documented widespread transmission of Zika virus provides additional evidence for the role of Zika virus infection during the first trimester of pregnancy; Zika virus has been demonstrated to cross the placenta, has been associated with congenital infection, and has been recovered in neural tissue (9,10). There is an urgent need for additional research to confirm the link between Zika virus infection and microcephaly through prospective and retrospective analytic studies, as well as to determine the critical Zika virus exposure period during pregnancy with respect to possible fetal infection and microcephaly. Pregnant women should protect themselves from mosquito bites by wearing long sleeves and long pants, applying insect repellent, and when spending time indoors, ensure that rooms are protected by screens or mosquito nets.
Acknowledgments
Health Secretaries of the states of Pernambuco, Paraíba, and Bahia; state Central Laboratories Network National Reference Laboratories; General Coordination of National Dengue Control Program; General Coordination of Surveillance and Response; General Coordination of Public Health Laboratories; CDC; Pan American Health Organization in Washington and the national office in Brazil.
Corresponding author: Giovanny Vinícius Araújo de França, giovanny.franca@saude.gov.br; +55 61 3315-3208.
References
- Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol 2012;206:331.e1–19. CrossRefexternal icon PubMedexternal icon
- Musso D, Cao-Lormeau VM, Gubler DJ. Zika virus: following the path of dengue and chikungunya? Lancet 2015;386:243–4. CrossRefexternal icon PubMedexternal icon
- Salvador FS, Fujita DM. Entry routes for Zika virus in Brazil after 2014 world cup: New possibilities. Travel Med Infect Dis 2016;14:49–51. CrossRefexternal icon PubMedexternal icon
- Campos GS, Bandeira AC, Sardi SI. Zika virus outbreak, Bahia, Brazil. Emerg Infect Dis 2015;21:1885–6. CrossRefexternal icon PubMedexternal icon
- Zanluca C, Melo VC, Mosimann AL, Santos GI, Santos CN, Luz K. First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz 2015;110:569–72. CrossRefexternal icon PubMedexternal icon
- de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull 2004;25(Suppl):S15–26. CrossRefexternal icon PubMedexternal icon
- Schuler-Faccini L, Ribeiro EM, Feitosa IM, et al. . Possible association between Zika virus infection and microcephaly—Brazil, 2015. MMWR Morb Mortal Wkly Rep 2016;65:59–62. CrossRefexternal icon PubMedexternal icon
- Nazer HJ, Cifuentes OL. [Congenital malformations in Latin America in the period 1995–2008][Spanish]. Rev Med Chil 2011;139:72–8. CrossRefexternal icon PubMedexternal icon
- Dick GW, Kitchen SF, Haddow AJ. Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg 1952;46:509–20. CrossRefexternal icon PubMedexternal icon
- Mlakar J, Korva M, Tul N, et al. Zika virus associated with microcephaly. N Engl J Med 2016. Epub ahead of print. CrossRefexternal icon
§ Castilla EE, Orioli IM, Luquetti DV, Dutra MG. Manual de Preenchimento e de Codificação de Anomalias Congênitas no Campo 34 da DN (SINASC). ECLAMC: Estudo Colaborativo Latino Americano de Malformações Congênitas. INaGeMP no IOC; Rio de Janeiro; 2010.
¶ http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nvuf.defexternal icon.
** http://www2.aids.gov.br/cgi/tabcgi.exe?caumul/anoma.defexternal icon.
†† Microcephaly case excess = (reported no. cases during 2015–2016 – mean no. cases2000–2014) / standard deviation above 2000–2014.
§§ http://tabnet.datasus.gov.brexternal icon.
¶¶ http://www.who.int/nutrition/publications/birthdefects_manual/en/external icon.
††† http://www.iec.gov.br/index.php/destaque/index/762external icon.
 TABLE. Average annual number of full-term infants reported with microcephaly* during 2000–2014 compared with 2015, prevalence of microcephaly in 2015, and number of states reporting confirmed transmission of Zika virus,† by region — 19 states, Brazil, 2015
TABLE. Average annual number of full-term infants reported with microcephaly* during 2000–2014 compared with 2015, prevalence of microcephaly in 2015, and number of states reporting confirmed transmission of Zika virus,† by region — 19 states, Brazil, 2015
| Region | 2000–2014 | 2015 | ||||||
|---|---|---|---|---|---|---|---|---|
| No. states | Average annual no. cases |
SD | Total no. cases | No. SDs above mean | Average no. live births§ | Microcephaly prevalence at birth¶ | No. states reporting confirmed transmission of Zika virus | |
| North | 2 | 14.1 | 4.7 | 11 | −0.7 | 310,508 | 0.4 | 2 |
| Northeast | 9 | 43.5 | 5.6 | 471 | 76.3 | 842,270 | 5.6 | 8 |
| Southeast | 3 | 65.2 | 6.8 | 58 | −1.1 | 1,137,408 | 0.5 | 2 |
| South | 1 | 21.5 | 6.2 | 3 | −3.0 | 376,599 | 0.1 | 0 |
| Center-West | 4 | 13.0 | 5.1 | 31 | 3.5 | 226,500 | 1.4 | 3 |
| Total | 19 | 157.3 | 17.7 | 574 | 23.6 | 2,893,285 | 2.0 | 15 |
Abbreviation: SD = standard deviation.
* Defined as head circumference ≥3 SDs below the mean for age and sex.
† Confirmed by real time reverse transcription–polymerase chain reaction.
§ From Brazil’s Live Birth Information System, 2009–2013 annual series.
¶ Cases of microcephaly per 10,000 live births.
 FIGURE 1. Locations of nine states with reported cases of microcephaly in 2015 exceeding 3 standard deviations and three states exceeding 20 standard deviations above the mean number of cases reported annually during 2000–2014 — Brazil, January 1, 2015–January 7, 2016
FIGURE 1. Locations of nine states with reported cases of microcephaly in 2015 exceeding 3 standard deviations and three states exceeding 20 standard deviations above the mean number of cases reported annually during 2000–2014 — Brazil, January 1, 2015–January 7, 2016
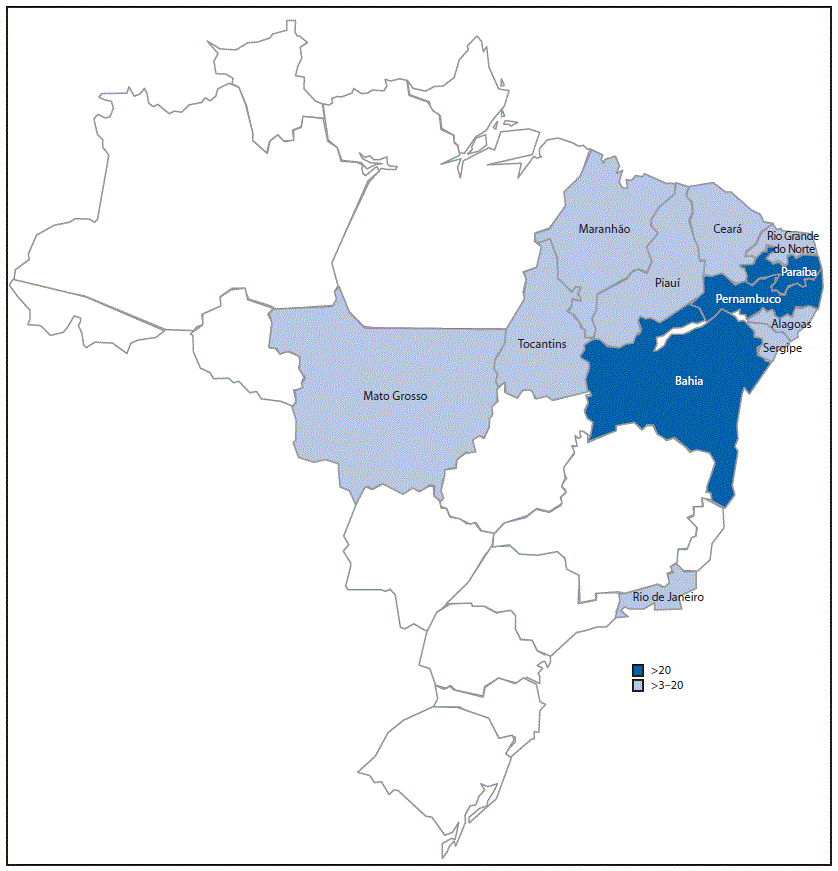
 FIGURE 2. Number of reported cases of microcephaly* in full-term† newborns following laboratory-confirmed Zika virus transmission§ — Pernambuco, Paraíba, and Bahia states, Brazil, 2015
FIGURE 2. Number of reported cases of microcephaly* in full-term† newborns following laboratory-confirmed Zika virus transmission§ — Pernambuco, Paraíba, and Bahia states, Brazil, 2015
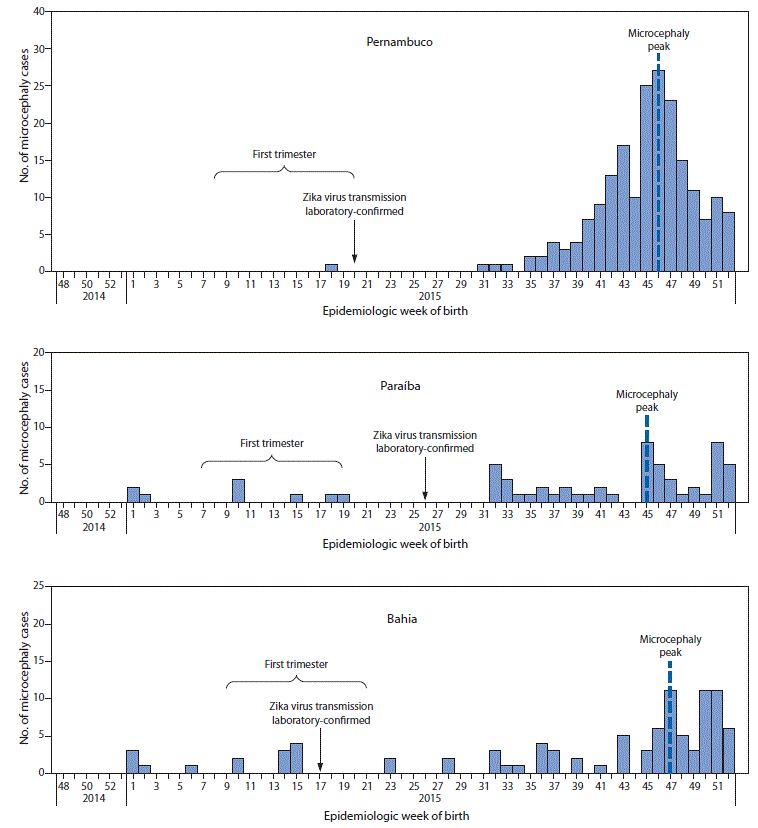
* Defined as head circumference =3 standard deviations below the mean for age and sex.
† The beginning of the first trimester indicator is estimated as 38 weeks preceding the peak period of reported cases of microcephaly.
§ Confirmed by real time reverse transcription–polymerase chain reaction.
Suggested citation for this article: Kleber de Oliveira W, Cortez-Escalante J, De Oliveira WT, et al. Increase in Reported Prevalence of Microcephaly in Infants Born to Women Living in Areas with Confirmed Zika Virus Transmission During the First Trimester of Pregnancy — Brazil, 2015. MMWR Morb Mortal Wkly Rep 2016;65:242–247. DOI: http://dx.doi.org/10.15585/mmwr.mm6509e2external icon.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.