What to know
The project used video calls and patient navigation to improve health care for people with cancer in rural areas.

Overview
People living in rural areas of the United States face higher cancer mortality than people living in urban areas, despite lower overall cancer incidence.1 People in rural areas typically have limited access to cancer care specialists and rely on primary care providers for ongoing care.
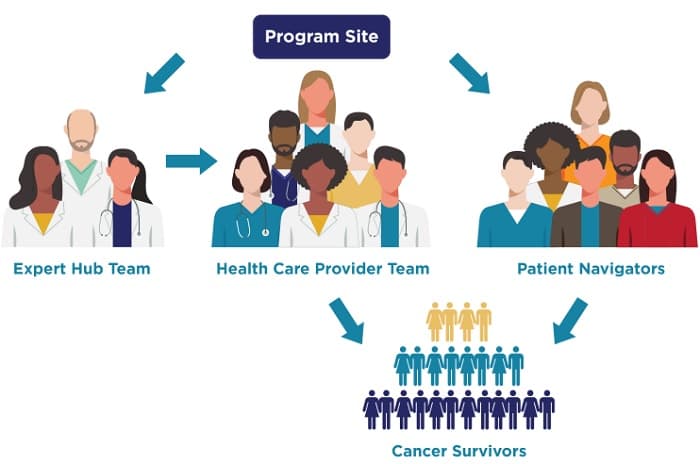
Telementoring through Project ECHO (Extension for Community Healthcare Outcomes) and patient navigation are two promising approaches to improve health care for people with cancer in rural areas.2–5 Project ECHO uses telementoring within communities of practice to increase workforce capacity and enhance rural health care providers' knowledge and skills. At the same time, patient navigation aims to remove barriers to care across the cancer care continuum and connect people with the community resources they need.
CDC's pilot program
CDC's Division of Cancer Prevention and Control selected four National Comprehensive Cancer Control Program award recipients (pilot sites) to conduct a pilot project called Improving the Health and Wellness of Cancer Survivors in Rural Communities.
The pilot project's goal was to bridge the health equity gap experienced by people with cancer in rural communities. For 12 months, each pilot site implemented telementoring and patient navigation strategies aligned with the needs and resources of its rural population. The pilot project provided valuable insight into the successful implementation of these strategies. This practice guide highlights four keys to success that health practitioners can use.
Pilot sites
- Kansas Department of Health and Environment
- Montana Department of Public Health and Human Services
- Nevada Cancer Coalition
- South Carolina Department of Health and Environmental Control
Keys to success
Collaborate with Partners That Have Similar Goals
Tailor Program Services to Local Needs and Resources
Recruit and Educate Health Care Providers and Patients
Monitor and Evaluate Program Implementation
References
1Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker B, Richardson LC. Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties—United States. MMWR Surveill Summ. 2017;66(14):1–13.
2Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(15 Suppl.):3539–3542.
3Alverson DC. An introduction to project ECHO. Rural Health Quarterly. 2017.
4Bhavaraju N, Nanni JE, Carlson C, Sholk J, Peterson K, Smith LA. Breaking the barriers to specialty care: practical ideas to improve health equity and reduce cost. 2016.
5O'Neil ME, Henley SJ, Rohan EA, Ellington TD, Gallaway MS. Lung cancer incidence in nonmetropolitan and metropolitan counties—United States, 2007–2016. MMWR Morb Mortal Wkly Rep. 2019;68:993–998.
