FIGURE. Cases of Shiga toxin--producing Escherichia coli O157 (STEC O157) in two outbreaks linked to a single beef slaughter facility, by subtype pattern and onset date* --- United States, June--August 2008
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Two Multistate Outbreaks of Shiga Toxin--Producing Escherichia coli Infections Linked to Beef from a Single Slaughter Facility --- United States, 2008
During May--August 2008, state and local health and agriculture departments, the U.S. Department of Agriculture's Food Safety and Inspection Service (FSIS), and CDC investigated two multistate outbreaks of Shiga toxin--producing Escherichia coli O157 (STEC O157) with distinct pulsed-field gel electrophoresis (PFGE) patterns. Investigations into each outbreak included epidemiologic analysis of food exposures, microbiologic testing, and food distribution tracebacks. This report summarizes the results of those investigations. During May 27--August 25, 2008, a total of 99 persons (64 from the first outbreak and 35 from the second outbreak) from 18 states had confirmed illness with an STEC O157 isolate indistinguishable from the outbreak PFGE patterns. A case-control study conducted as part of the first investigation found a statistically significant association with purchase of ground beef from one large grocery chain (matched odds ratio [mOR] = 9.3). Traceback investigations for both outbreaks led to the same slaughter facility, resulting in multiple nationwide recalls of ground beef, intact beef, and beef products used to produce ground beef. This is the first report of two distinct STEC O157 outbreaks traced to a single slaughter facility and the first documented report of outbreaks linked to STEC O157 contamination of intact beef cuts ground by a retail chain. To help reduce the risk for outbreaks of STEC O157, the public health community should continue to educate consumers regarding the proper measures to take when handling and consuming ground beef.
Outbreak 1
On June 14, 2008, the Ohio Department of Health posted a cluster of seven STEC O157 isolates with an indistinguishable PFGE pattern (pattern 1)* on PulseNet, the national molecular subtyping network for foodborne disease surveillance. Most of the ill patients resided in an urban area of central Ohio. At approximately the same time, the Michigan Department of Community Health was interviewing patients in an STEC O157 cluster with the same PFGE pattern as the patients in Ohio. Several Michigan patients reported consuming ground beef before their illness, and some reported purchasing it at one of several stores belonging to a large national retail grocery chain (chain A). On June 18, state and local health and agriculture departments, FSIS, and CDC's OutbreakNet Team initiated an investigation to determine the extent and source of the outbreak.
A confirmed case was defined as illness in a person with an STEC O157 isolate having both a PFGE pattern indistinguishable from PFGE pattern 1 and multiple-locus variable-number tandem repeat analysis (MLVA) pattern 1,† and illness onset (or specimen collection date, if onset date was unavailable) after May 26. Sixty-four confirmed cases were identified in 12 states: Alabama (one case), Florida (one), Georgia (eight), Indiana (three), Kentucky (one), Michigan (23), New Jersey (one), New York (one), Ohio (21), Texas (one), Utah (two), and West Virginia (one). Illness onset dates ranged from May 27 to August 7 (Figure). Median age of patients was 21 years (range: 1--71 years); 40 (63%) were female. Thirty-two (59%) of 54 patients with available information were hospitalized, and two developed hemolytic uremic syndrome. No deaths were reported.
During June 20--25, the Ohio and Michigan state health departments and CDC conducted a case-control study examining ground beef and several other exposures linked to STEC O157 infections in previous outbreaks. All patients in Ohio and Michigan identified through June 25 were eligible for interview. Controls were identified through reverse-digit directory and matched on neighborhood, as identified by reverse directory, and age group (<18, 18--60, and >60 years); controls were asked about their food exposures for the week preceding the onset date of their matched case-patient. Data were analyzed using a conditional logistic regression model with exact methodologies because of the small sample size. Twenty-five case-patients and 65 controls from Michigan and Ohio were interviewed with a goal of three controls per case. Twenty-one case-patients were matched: 18 with three controls, two with two controls, and one with one control. Illness was significantly associated with purchasing ground beef from a store owned by chain A (mOR = 9.3) (Table). Seven samples of ground beef purchased at chain A stores, collected from patient homes, yielded STEC O157 with PFGE pattern 1 and MLVA pattern 1.
Traceback investigation of the ground beef from chain A identified a single large beef slaughter facility in Nebraska that supplied beef to chain A stores in outbreak-associated areas of Michigan and Ohio. On June 25, chain A issued a recall of all ground beef sold by its Michigan and Ohio stores in the regions where patients resided.§ On June 30, the slaughter facility initiated a nationwide recall, which was expanded July 3 to encompass beef products used to produce ground beef totaling 5.3 million pounds.¶
Outbreak 2
On July 28, 2008, PulseNet alerted CDC regarding a cluster of STEC O157 isolates from eight states with an indistinguishable PFGE pattern (pattern 2).** Initial telephone calls by local and state health departments revealed that several patients reported consuming undercooked ground beef. On July 29, local and state health and agriculture departments, FSIS, and CDC initiated an investigation to determine the extent and source of the outbreak.
A confirmed case was defined as illness in a person with an STEC O157 isolate indistinguishable from both PFGE pattern 2 and MLVA pattern 2 with an isolation date on or after July 1. Thirty-five cases were identified in eight states: Colorado (one case), Connecticut (one), Massachusetts (eight), New Jersey (two), New York (two), Ohio (seven), Pennsylvania (eight), and Virginia (six), with illness onset dates ranging from June 29 to August 25 (Figure). Median age was 18.5 years (range: 1--70 years). Median age was 18.5 years (range: 1--70 years). Of the 35 patients, 19 (54%) were female. Nineteen (63%) of 30 patients with available information were hospitalized, and one developed hemolytic uremic syndrome. No deaths were reported.
Thirty patients were interviewed using the questionnaire used in outbreak 1. Twenty-four (80%) patients reported eating ground beef in the home, and 13 (54%) of those reporting ground beef consumption indicated that it was raw, bloody, or pink. Seventeen (57%) of 30 patients had exposure to ground beef purchased from one of two grocery chains (chain B and chain C). One sample of raw ground beef purchased at chain B (a regional upscale chain) and three samples of ground beef purchased at chain C (a national upscale chain), all collected from patient homes, and one sample of intact beef collected from chain B before grinding yielded STEC O157 with PFGE pattern 2 and MLVA pattern 2.
Traceback investigations indicated that the same slaughter facility linked to outbreak 1 was the sole source of the contaminated beef from chain B and was one of multiple suppliers to chain C. On July 28, chain B announced a retail-level recall of ground beef products.†† Chain C announced a recall on August 8,§§ and the slaughter facility initiated a nationwide recall of beef products linked to outbreak 2. This recall was expanded on August 14 to include approximately 1.36 million pounds of additional intact beef cuts.¶¶
Slaughter Facility Control Measures
In addition to the traceback investigations and recall actions described above, FSIS also performed investigations of the slaughter facility. During both outbreaks, FSIS concluded that the production practices employed by the slaughter facility were insufficient to effectively control STEC O157 and that the products subject to recall in both outbreaks might have been produced under unsanitary conditions. As a result of the outbreaks, FSIS microbiologists evaluated beef testing procedures at the facility. Recommendations were made to modify testing procedures to improve the ability to detect contamination in beef products produced by the facility. In addition, the facility implemented corrective and preventative measures regarding its production practices.
Reported by
S Nowicki, MPH, E Brandt, Ohio Dept of Health. K Sheline, MPH, S Bidol, MPH, J Collins, MPH, Michigan Dept of Community Health. M Toblin-D'Angelo, MD, C Drenzek, DVM, J Jenkins, Georgia Div of Public Health. E Harvey, Massachusetts Dept of Public Health. J Marsden, MA, Montgomery County Health Dept, Norristown; A Weltman, MD, Pennsylvania Dept of Health. B Kissler, MPH, WS Chen, MD, S Seys, MPH, Food Safety and Inspection Svc, US Dept of Agriculture. E Hyytia-Trees, PhD, DVM, M Leeper, M Viray, MD, E Cavallaro, MD, K Wannemuehler, PhD, MJ Sotir, PhD, Div of Foodborne, Bacterial, and Mycotic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases, CDC.
Editorial Note
Continued advances in the ability to detect and identify STEC O157 outbreaks and their sources of contamination have provided opportunities to improve food safety. However, despite beef testing and monitoring (1) and interventions at beef slaughtering and processing facilities aimed at preventing STEC O157 contamination, contaminated beef continues to cause outbreaks (2). In the two outbreaks described in this report, 99 cases were identified. Because an estimated 20 STEC illnesses occur for every one reported, the number of cases reported in the outbreaks likely represent a small proportion of the actual number of persons who became ill (3).
The outbreaks were notable because of two findings. First was the discovery in outbreak 2 of STEC O157 bacterial contamination of an intact cut of beef intended for grinding at a retail chain. Ground beef (and mechanically tenderized steaks) can be contaminated during processing throughout the product, resulting in a risk to consumers if ground beef is only cooked at the surface. STEC O157 is considered an adulterant in nonintact products such as ground beef, and FSIS considers its presence unacceptable in intact products intended for use as ground beef (4). Contamination of intact cuts of beef generally occurs as a consequence of handling during hide removal and dressing of carcasses. Meat contamination at slaughter facilities can indicate that the facility is not adequately addressing contamination from hides.
The second notable finding was that the two outbreaks caused widespread illness and were linked to multiple contaminated meat products, but were traced to a single beef slaughter facility. The detection of two STEC O157 outbreaks linked to the same beef slaughter facility suggests that improved processing controls were needed within the plant. FSIS recommended changes designed to improve the ability to detect contamination events, both within that facility and industrywide, including the initiation of a testing program at establishments processing trim derived from intact cuts, because trim is often converted into ground beef, and institution of new verification procedures by inspectors aimed at further minimizing contamination during slaughter.
Public health agencies should continue to educate consumers regarding the dangers associated with handling raw ground beef and consuming undercooked ground beef or other undercooked nonintact beef products. Consumers should know that preventive measures include thorough hand washing after handling raw beef; washing any surfaces that have come into contact with raw beef with hot, soapy water; keeping raw beef separate from other food products; and cooking ground beef to 160.0°F (71.1°C), as measured by a food thermometer.***
Acknowledgment
This report is based, in part, on contributions by J Achenbach, MPH, CM Baysinger, MPH, J Daly, P Lawn, K Smith, Montgomery County Health Dept, Norristown, Pennsylvania; M Moore, P Neves, Massachusetts Dept of Public Health Bur of Environmental Health --- Food Protection Program, Jamaica Plain, Massachusetts; and KG Holt, DVM, US Dept of Agriculture Food Safety and Inspection Svc, Atlanta, Georgia.
References
- Naugle AL, Holt KG, Levine P, et al. Food safety and inspection service regulatory testing program for Escherichia coli O157:H7 in raw ground beef. J Food Prot 2005;68:462--8.
- CDC. Multistate outbreak of Escherichia coli O157:H7 infections associated with eating ground beef---United States, June--July 2002. MMWR 2002;51:637--9.
- Mead PS, Slutsker L, Dietz V, et al. Food-related illness and death in the United States. Emerg Infect Dis 1999;5:607--25.
- US Department of Agriculture. Microbiological testing program and other verification activities for Escherichia coli O157:H7 in raw ground beef products and raw ground beef components and beef patty components. FSIS Directive 10,010.1. Washington, DC: US Department of Agriculture, Food Safety Inspection Service; 2004.
* XbaI/BlnI pattern EXHX01.0047/EXHA26.0332.
† Included were isolates that were either indistinguishable from MLVA pattern 1 or different at a single locus by one repeat. MLVA testing was included as a criterion because PFGE pattern 1 was commonly reported to PulseNet.
§ USDA Food Safety Inspection Service. Retail recall release FSIS-R01-2008. Available at http://www.fsis.usda.gov/news_&_events/r01-2008_release/index.asp.
¶ USDA Food Safety Inspection Service. Recall release FSIS-RC-022-2008. Available at http://www.fsis.usda.gov/news_&_events/recall_022_2008_release/index.asp.
** XbaI/BlnI pattern EXHX01.0008/EXHA26.0569.
†† Dorothy Lane Market. Recalled products. Available at http://www.dorothylane.com/company/product%20recalls/2008-07-28_groundbeef.html.
§§ Whole Foods. Whole Foods Market voluntarily recalls fresh ground beef. August 8, 2008. Available at http://www.wholefoodsmarket.com/nutrition/product-recalls.php#self.
¶¶ USDA Food Safety Inspection Service. Recall release FSIS-RC-029-2008. Available at http://www.fsis.usda.gov/news_&_events/recall_029_2008_release/index.asp.
*** USDA Food Safety Inspection Service. Food safety education: is it done yet? Available at http://www.fsis.usda.gov/is_it_done_yet.
What is already known on this topic?
Infection with Shiga toxin-producing Escherichia coli O157 (STEC O157) has been linked to consumption of undercooked ground beef.
What is added by this report?
Two separate outbreaks of STEC O157 were linked to the same beef slaughter facility, and contamination was found in intact beef that was intended for grinding at a retail grocery chain.
What are the implications for public health practice?
To help reduce the risk for outbreaks of STEC O157, the public health community should continue to educate consumers regarding the proper measures to take when handling and consuming ground beef.
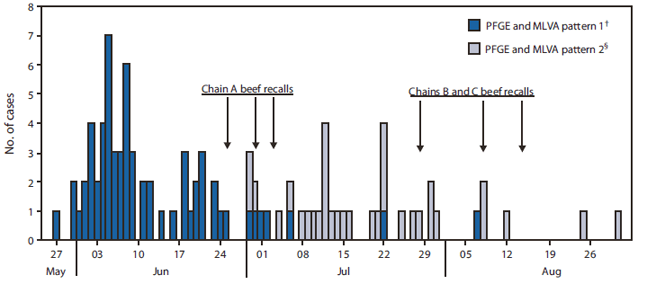
Abbreviations: PFGE = pulsed-field gel electrophoresis, MLVA = multiple-locus variable-number tandem repeat analysis.
* For patients with unreported onset dates (n = 8), onset dates were estimated using the date of STEC O157 isolation minus 3 days. Two patients were excluded because no reliable onset or isolation dates were available.
† Sixty-four confirmed cases were identified in 12 states: Alabama (one case), Florida (one), Georgia (eight), Indiana (three), Kentucky (one), Michigan (23), New Jersey (one), New York (one), Ohio (21), Texas (one), Utah (two), and West Virginia (one).
§ Thirty-five cases were identified in eight states: Colorado (one case), Connecticut (one), Massachusetts (eight), New Jersey (two), New York (two), Ohio (seven), Pennsylvania (eight), and Virginia (six).
Alternate Text: The figure above shows cases of Shiga toxin-producing Escherichia coli O157 (STEC O157) in two outbreaks linked to a single beef slaughter facility, by subtype pattern and onset date, in the United States, during June-August 2008. Illness onset dates ranged from May 27 to August 7.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


