Your Risk of C. diff
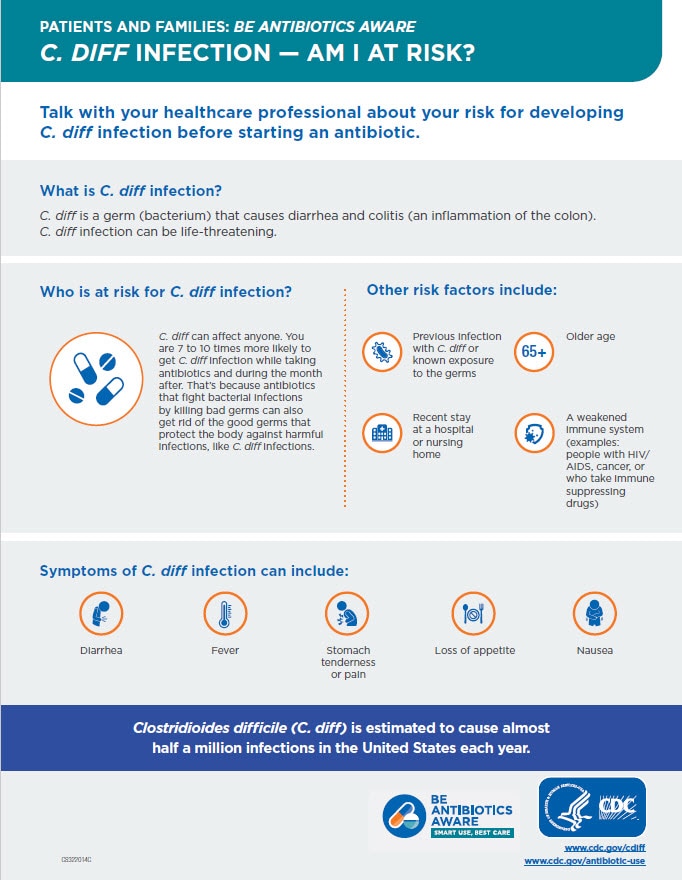
Talk with your healthcare professional about your risk for developing C. diff.
C. diff bacteria are commonly found in the environment, but most cases of C. diff occur while you’re taking antibiotics or not long after you’ve finished taking antibiotics. People are 7 to 10 times more likely to get C. diff while on antibiotics and during the month after.
That’s because antibiotics that fight bacterial infections by killing bad germs can also get rid of the good germs that protect the body against harmful infections, like C. diff infection. If you take antibiotics for more than a week, you could be even more at risk.
Other C. diff risk factors include:
- older age (65 and older)
- recent stay at a hospital or nursing home
- a weakened immune system, such as people with HIV/AIDS, cancer, or organ transplant patients taking immunosuppressive drugs
- previous infection with C. diff or known exposure to the germs
You can still get C. diff even if you have none of these risk factors.

The microbiome is the neighborhood of good and bad germs that live in or on your body—including your stomach and intestines, your mouth, and your urinary tract—and on your skin.
Some of those germs can cause illness, but others are very important in keeping you healthy. A healthy microbiome helps protect you from infection, but antibiotics disrupt your microbiome, wiping out both the good and the bad bacteria. The effect of antibiotics can last as long as several months. If you come in contact with C. diff germs during this time, you can get sick.
Common complications of C. diff

Dehydration

Inflammation of the colon, known as colitis

Diarrhea
Rare complications of C. diff

Serious intestinal condition, such as toxic megacolon

Sepsis, the body’s extreme response to an infection

Death
You may be wondering… What is sepsis?
Sometimes when healthy people come into contact with C. diff, they will begin to carry C. diff germs in or on their body, but they won’t get sick.
In medical terms, they are said to be “colonized” with C. diff. This is also sometimes called “C. diff carriage,” and a person might be said to be a “C. diff carrier.”
Someone who is colonized has NO signs or symptoms.
Colonization is more common than C. diff infection and does not require treatment. Once your body is colonized, you can remain colonized for several months.
If you are colonized with C. diff, you can spread the infection to others.
Some reasons you might become colonized are:
- You’ve recently recovered from C. diff.
- You have a history of taking antibiotics.
- You’ve recently been hospitalized.
Once your body is colonized with C. diff, you can remain colonized for several months. Colonization is more common than C. diff infection and does not require treatment.
Because it’s possible to spread C. diff to others while you’re colonized, it’s important to always practice good hand hygiene, making sure to wash your hands well with soap and water every time you use the bathroom and always before you eat.