Tuberculosis in the United States
NOTE: The slide set is in the public domain. You may reproduce these slides without permission; however it is requested that you include an attribution that the materials were developed by CDC (e.g., “Source: CDC” or “Slides developed by CDC”). No substantive changes should be made to the content.
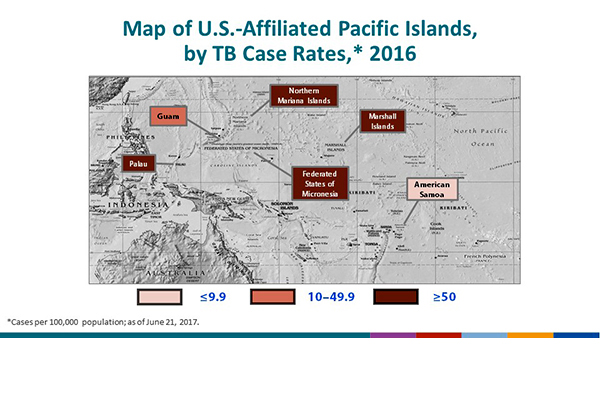
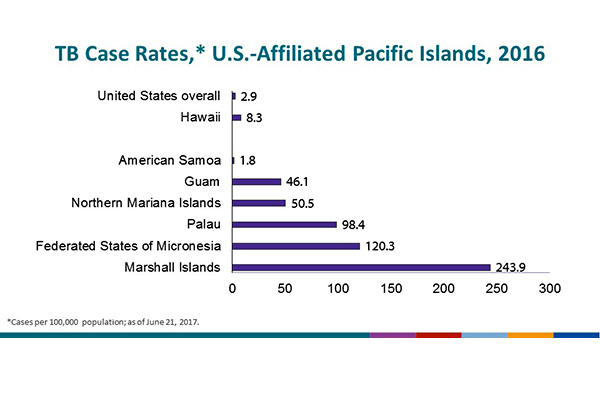
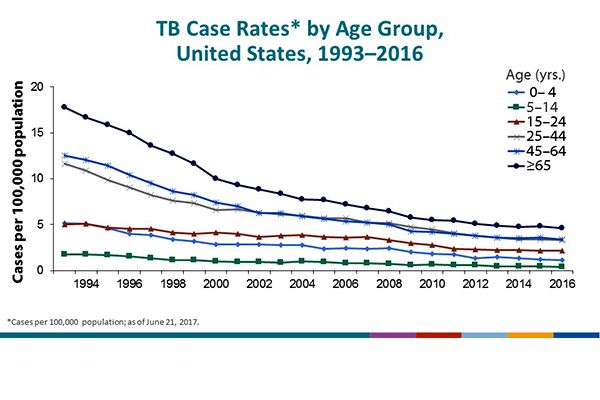
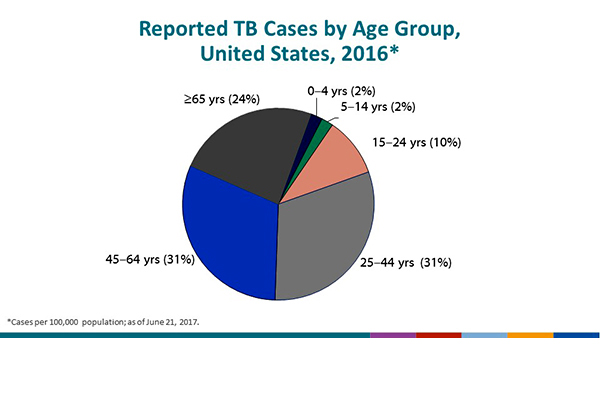
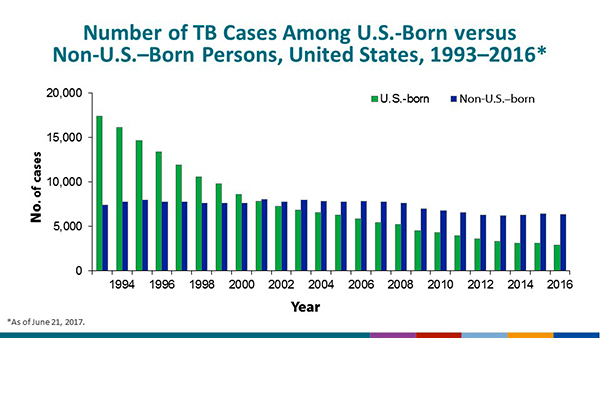
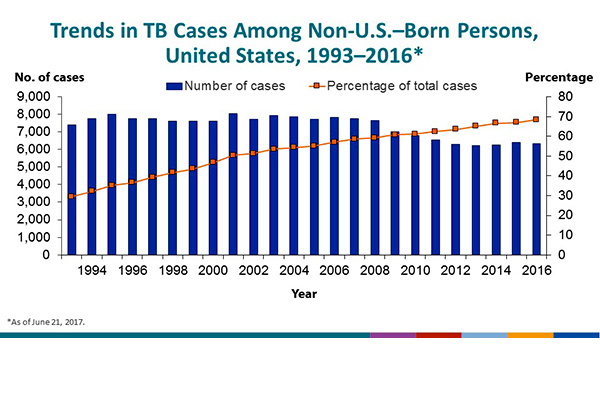
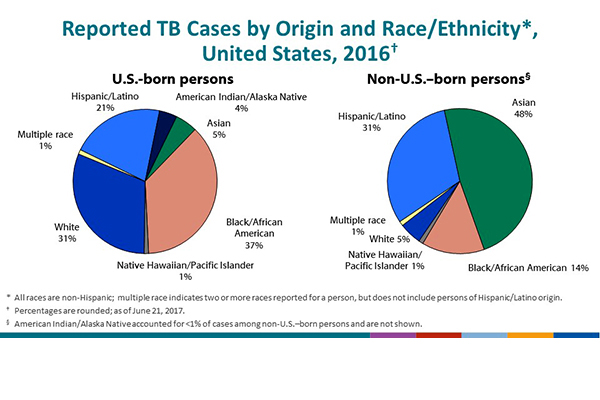
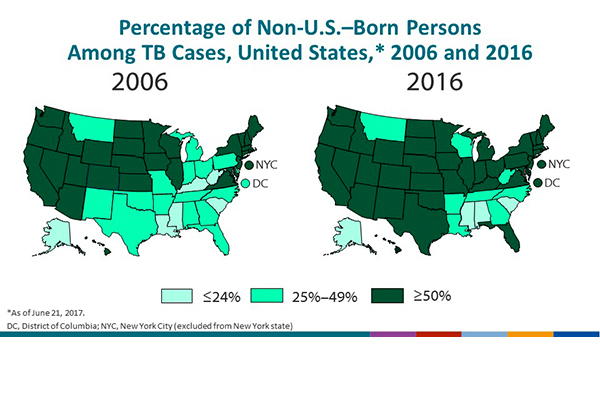
National Tuberculosis Surveillance System Highlights from 2016
This slide series was developed as an accompaniment to the document Reported Tuberculosis in the United States, 2016