Heavy Menstrual Bleeding
Menorrhagia is menstrual bleeding that lasts more than 7 days. It can also be bleeding that is very heavy. How do you know if you have heavy bleeding? If you need to change your tampon or pad after less than 2 hours or you pass clots the size of a quarter or larger, that is heavy bleeding. If you have this type of bleeding, you should see a doctor.
Untreated heavy or prolonged bleeding can stop you from living your life to the fullest. It also can cause anemia. Anemia is a common blood problem that can leave you feeling tired or weak. If you have a bleeding problem, it could lead to other health problems. Sometimes treatments, such as dilation and curettage (D&C) or a hysterectomy, might be done when these procedures could have been avoided.
Causes
Possible causes fall into the following three areas:
- Uterine-related problems
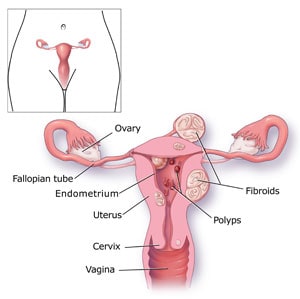
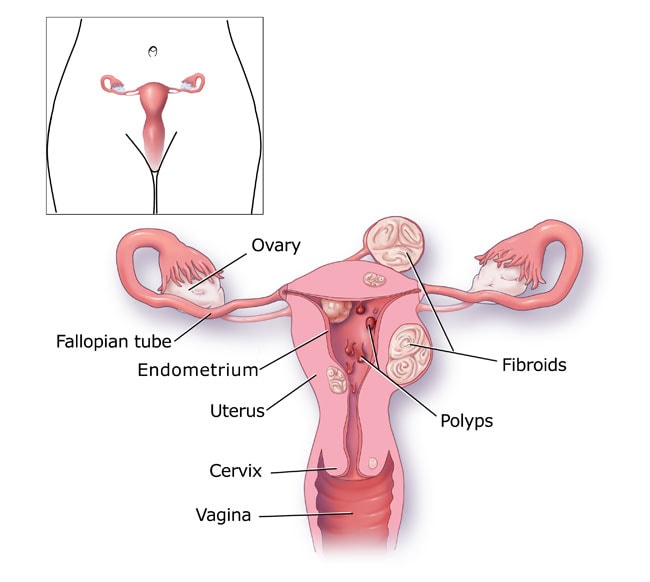
- Growths or tumors of the uterus that are not cancer; these can be called uterine fibroids or polyps.
- Cancer of the uterus or cervix.
- Certain types of birth control—for example, an intrauterine device (IUD).
- Problems related to pregnancy, such as a miscarriage or ectopic pregnancy, can cause abnormal bleeding. A miscarriage is when an unborn baby (also called a fetus) dies in the uterus. An ectopic pregnancy is when a baby starts to grow outside the womb (uterus), which is not safe.
- Hormone-related problems
- Other illnesses or disorders
- Bleeding-related disorders, such as von Willebrand disease (VWD) or platelet function disorder.
- Nonbleeding-related disorders such as liver, kidney, or thyroid disease; pelvic inflammatory disease; and cancer.
In addition, certain drugs, such as aspirin, can cause increased bleeding. Doctors have not been able to find the cause in half of all women who have this problem. If you have bleeding such as this, and your gynecologist has not found any problems during your routine visit, you should be tested for a bleeding disorder.
Signs
You might have menorrhagia if you:
- Have a menstrual flow that soaks through one or more pads or tampons every hour for several hours in a row.
- Need to double up on pads to control your menstrual flow.
- Need to change pads or tampons during the night.
- Have menstrual periods lasting more than 7 days.
- Have a menstrual flow with blood clots the size of a quarter or larger.
- Have a heavy menstrual flow that keeps you from doing the things you would do normally.
- Have constant pain in the lower part of the stomach during your periods.
- Are tired, lack energy, or are short of breath.
Diagnosis
Finding out if a woman has heavy menstrual bleeding often is not easy because each person might think of “heavy bleeding” in a different way. Usually, menstrual bleeding lasts about 4 to 5 days and the amount of blood lost is small (2 to 3 tablespoons). However, women who have menorrhagia usually bleed for more than 7 days and lose twice as much blood. If you have bleeding that lasts longer than 7 days per period, or is so heavy that you have to change your pad or tampon nearly every hour, you need to talk with your doctor.
To find out if you have menorrhagia, your doctor will ask you about your medical history and menstrual cycles.
He or she may ask you questions like the following:
- How old were you when you got your first period?
- How long is your menstrual cycle?
- How many days does your period usually last?
- How many days do you consider your period to be heavy?
- How do your periods affect your quality of life?
Your doctor may also ask if any of your family members have had heavy menstrual bleeding. He or she may also have you complete this questionnaire [PDF – 127 KB] to help determine if you need to be tested for a possible bleeding disorder.
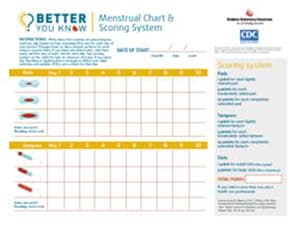
You might want to track your periods by writing down the dates of your periods and how heavy you think your flow is (maybe by counting how many pads or tampons you use). Do this before you visit the doctor so that you can give the doctor as much information as possible. Above is a picture of a chart that is used by some doctors to track your period. You can make your own chart based on the one shown. Your doctor also will do a pelvic exam and might tell you about other tests that can be done to help find out if you have menorrhagia.
Tests
Your doctor might tell you that one or more of the following tests will help find out if you have a bleeding problem:
- Blood test. In this test, your blood will be taken using a needle. It will then be looked at to check for anemia, problems with the thyroid, or problems with the way the blood clots.
- Pap test. For this test, cells from your cervix are removed and then looked at to find out if you have an infection, inflammation, or changes in your cells that might be cancer or might cause cancer.
- Endometrial biopsy. Tissue samples are taken from the inside lining of your uterus or “endometrium” to find out if you have cancer or other abnormal cells. You might feel as if you were having a bad menstrual cramp while this test is being done. But, it does not take long, and the pain usually goes away when the test ends.
- Ultrasound. This is a painless test using sound waves and a computer to show what your blood vessels, tissues, and organs look like. Your doctor then can see how they are working and check your blood flow.
Using the results of these first tests, the doctor might recommend more tests, including,
- Sonohysterogram. This ultrasound scan is done after fluid is injected through a tube into the uterus by way of your vagina and cervix. This lets your doctor look for problems in the lining of your uterus. Mild to moderate cramping or pressure can be felt during this procedure.
- Hysteroscopy. This is a procedure to look at the inside of the uterus using a tiny tool to see if you have fibroids, polyps, or other problems that might be causing bleeding. You might be given drugs to put you to sleep (this is known as “general anesthesia) or drugs simply to numb the area being looked at (this is called “local anesthesia”).
- Dilation and Curettage (D&C). This is a procedure (or test) that can be used to find and treat the cause of bleeding. During a D&C, the inside lining of your uterus is scraped and looked at to see what might be causing the bleeding. A D&C is a simple procedure. Most often it is done in an operating room, but you will not have to stay in the hospital afterwards. You might be given drugs to make you sleep during the procedure, or you might be given something that will numb only the area to be worked on.
Treatment
The type of treatment you get will depend on the cause of your bleeding and how serious it is. Your doctor also will look at things such as your age, general health, and medical history; how well you respond to certain medicines, procedures, or therapies; and your wants and needs. For example, some women do not want to have a period, some want to know when they can usually expect to have their period, and some want just to reduce the amount of bleeding. Some women want to make sure they can still have children in the future. Others want to lessen the pain more than they want to reduce the amount of bleeding. Some treatments are ongoing and others are done one time. You should discuss all of your options with your doctor to decide which is best for you. Following is a list of the more common treatments.
Drug Therapy
- Iron supplements. To get more iron into your blood to help it carry oxygen if you show signs of anemia.
- Ibuprofen (Advil). To help reduce pain, menstrual cramps, and the amount of bleeding. In some women, NSAIDS can increase the risk of bleeding.
- Birth control pills. To help make periods more regular and reduce the amount of bleeding.
- Intrauterine contraception (IUC). To help make periods more regular and reduce the amount of bleeding through drug-releasing devices placed into the uterus.
- Hormone therapy (drugs that contain estrogen and/or progesterone). To reduce the amount of bleeding.
- Desmopressin Nasal Spray (Stimate®). To stop bleeding in people who have certain bleeding disorders, such as von Willebrand disease and mild hemophilia, by releasing a clotting protein or “factor”, stored in the lining of the blood vessels that helps the blood to clot and temporarily increasing the level of these proteins in the blood.
- Antifibrinolytic medicines (tranexamic acid, aminocaproic acid). To reduce the amount of bleeding by stopping a clot from breaking down once it has formed.
Surgical Treatment
- Dilation and Curettage (D&C). A procedure in which the top layer of the uterus lining is removed to reduce menstrual bleeding. This procedure might need to be repeated over time.
- Operative hysteroscopy. A surgical procedure, using a special tool to view the inside of the uterus, that can be used to help remove polyps and fibroids, correct abnormalities of the uterus, and remove the lining of the uterus to manage heavy menstrual flow.
- Endometrial ablation or resection. Two types of surgical procedures using different techniques in which all or part of the lining of the uterus is removed to control menstrual bleeding. While some patients will stop having menstrual periods altogether, others may continue to have periods but the menstrual flow will be lighter than before. Although the procedures do not remove the uterus, they will prevent women from having children in the future.
- Hysterectomy. A major operation requiring hospitalization that involves surgically removing the entire uterus. After having this procedure, a woman can no longer become pregnant and will stop having her period.
Menorrhagia is common among women. But, many women do not know that they can get help for it. Others do not get help because they are too embarrassed to talk with a doctor about their problem. Talking openly with your doctor is very important in making sure you are diagnosed properly and get the right treatment.
Who is Affected
Heavy bleeding (menorrhagia) is one of the most common problems women report to their doctors. It affects more than 10 million American women each year. This means that about one out of every five women has it.
References
- Fast Facts for Your Health: Menorrhagia. National Women’s Health Resource Center (NWHRC), Washington, D.C. http://www.healthywomen.org.
- Menstruation: Heavy Bleeding (Menorrhagia). PreventDisease.com. http://preventdisease.com/diseases/menstruation_heavy_bleeding.html.
- Women with Inherited Bleeding Disorders: Surgical Options for Menorrhagia. Canadian Hemophilia Society. http://www.hemophilia.ca.
- Menorrhagia (heavy menstrual bleeding). CNN.com. http://www.cnn.com/HEALTH/library/DS/00394.html.
- Phillip CS, Faiz A, Dowling NF, Beckman M, Owens S, Ayers C, Bachmann G. Development of a screening tool for identifying women with menorrhagia for hemostatic evaluation. American Journal of Obstetrics & Gynecology 2008;198:163.e1–163.e8.
- Apgar BS, Kaufman AH, George-Nwogu U, Kittendorf A. Treatment of menorrhagia. American Family Physician 2007;75:1813–1819,1820. http://www.aafp.org/afp/20070615/1813.html.
- Heavy Bleeding and Endometrial Ablation. FertilityAnswers.com. http://www.fertilityanswers.com/endometrial_ablation.htm.
- Menorrhagia (heavy menstrual bleeding). MayoClinic.com Health Library. http://www.riverside-online.com/health_reference/Womens-Health/DS00394.cfm.
National Collaborating Centre for Women’s and Children’s Health. National Institute for Health and Clinical Excellence (NICE). Heavy menstrual bleeding. London: Royal College of Obstetricians and Gynaecologists Press; 2007. - Higham JM, O’Brien PM, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. British Journal of Obstetrics and Gynaecology. 1990;97:734–739.