*Clean Air Act Amendments of 1970. Pub. L. No. 91-604, 81 Stat. 486 (December 31, 1970).
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Unhealthy Air Quality — United States, 2006–2009
Particulate matter and ozone are two well-characterized air pollutants that can affect health and are monitored by the U.S. Environmental Protection Agency (EPA). Particulate matter (solid or liquid particles suspended in the air) varies widely in size and chemical composition and can include smoke, fumes, soot, and combustion by-products, as well as natural particles (e.g., windblown dust, pollen, and sea salt) (1,2). Particulate matter therefore represents a complex class of air pollutants that differ from other gaseous air pollutants (e.g., ozone). The transport and effect of particulate matter, both in the atmosphere and in the human respiratory tract, are governed principally by particulate size, shape, and density. Individual particles are characterized by their equivalent aerodynamic diameter: coarse particulate matter (2.5--10 µm); fine particulate matter, or PM2.5 (0.1--2.5 µm); and ultrafine particulate matter (<0.1 µm). Ozone is a gas that occurs naturally in the stratosphere, approximately 10--30 miles above the earth's surface, protecting the earth from the sun's ultraviolet rays. Ozone also exists at ground level and is the primary component of smog. At ground level, ozone is created when specific pollutants react in the presence of sunlight. In urban areas, vehicular and industrial emissions are chief contributors to ozone production. Ground-level ozone adversely affects health and damages the environment.
The association between outdoor particulate matter concentrations and acute and chronic adverse health outcomes includes premature death, lung cancer, exacerbation of respiratory and cardiovascular disease, and increased risks for cardiovascular morbidity (e.g., myocardial infarction and arrhythmia) (1--6). Data indicate that fine particulate matter is the size fraction most strongly associated with these observed health effects (1--7). Populations most susceptible to these exposures include older adults and children, as well as persons with heart and lung disease. National Ambient Air Quality Standards (NAAQS) were set forth in the Clean Air Act Amendments of 1970* requiring EPA to set air quality standards for specific pollutants, such as PM2.5 and ozone, to protect the health of the general public, as well as that of sensitive populations. States that do not meet the standards are subject to additional regulatory requirements and must develop a state implementation plan to meet the standards. State implementation plans might include control requirements and limits on emissions. In 2006, on the basis of increasing evidence of the effects of PM2.5 on human health, EPA revised its 24-hour NAAQS from 65 µg/m3 to 35 µg/m3. Throughout the United States, PM2.5 concentrations have been decreasing; more counties were in compliance with national pollution standards as of 2008 compared with previous years (8). During 2001--2008, the average annual and 24-hour PM2.5 concentrations declined by 17% and 19%, respectively (8).
Short-term exposures to ozone have been associated with an increase in mortality as well as cardiovascular- and respiratory-related hospitalizations (9--11). Ozone exposure can result in lung and throat irritation, lung inflammation, wheezing, and difficulty breathing (11--13). Exposure to ozone also exacerbates bronchitis, emphysema, and asthma (11,14,15). Populations at risk for ozone-related health effects have been characterized as those that typically spend long periods outdoors (e.g., persons with outdoor occupations and athletes), as well as sensitive groups, including infants and children, older persons, and persons with respiratory or cardiovascular disease (including asthma) (16--21).
In 2008, EPA decreased NAAQS for ozone to an 8-hour standard of 75 parts per billion (ppb) (0.075 parts per million [ppm]) from the level of 80 ppb (0.08 ppm) set in 1997. In 2008, the national average concentration of ozone was 14% lower than in 1990. This reduction has been attributed to decreasing levels of summer-time emissions of nitrogen oxides and volatile organic compounds (two key precursors to the formation of ozone) from transportation and fuel combustion sources (8).
To characterize the populations who live in areas with PM2.5 and ozone levels that exceed those allowed by the NAAQS (i.e., nonattainment areas), CDC categorized the proportions of populations who live in these areas by race/ethnicity, level of education attainment, and household income, as represented by the poverty to income ratio (PIR). Other factors, including disability status, were not examined because of limited data. Relative difference (percentage difference) was calculated by dividing the difference between the referent category and each category in the classifying variable by the value in the referent category and multiplying by 100.The referent groups selected were consistent with referent groups used in national survey summaries.
Three data sources were used for this assessment: 1) population estimates for 2007 and 2008 from the U.S. Census Bureau Population Estimates Program for U.S. counties, 2) 3-year education and income estimates from the American Community Survey (2006−2008), and 3) data on nonattainment counties for PM2.5 (2006−2008) and ozone (2007−2009) obtained from EPA (http://www.epa.gov/airtrends/values.html). EPA areas are designated as nonattainment on the basis of EPA design values (i.e., statistics derived from multiple years of data that describe the ambient air quality status of a given area relative to the level of the NAAQS). In this report, counties in nonattainment represent a location that had a design value for the 24-hour PM2.5 standard that exceeded the 2006 24-hour PM2.5 standard of 35 µg/m3; the design value was calculated as the 3-year average (2006−2008) of annual 98th percentile PM2.5 concentrations that were valid (i.e., 24-hour averages that were available for at least 75% of possible hours in a day). For ozone, counties of nonattainment had a design value (calculated as the 3-year average [2007−2009] of the annual fourth-highest daily maximum 8-hour ozone concentration) that was greater than the 2008 8-hour ozone standard of 75 ppb.
The percentage of the population living in 24-hour PM2.5 or in 8-hour ozone nonattainment counties were summarized for each category of each demographic group. Relative differences between categories were calculated as the percentage difference of each category compared with a referent category.
A total of 53 (23.3%) of 227 counties were nonattainment counties for the 2006 24-hour PM2.5 standard (Figure 1), representing 13.6% of the U.S population in 2007 (2007 U.S. population: 301,621,157). Twenty-six (49.1%) of these counties were classified as large central metropolitan counties or large fringe metropolitan counties (i.e., counties in a metropolitan statistical area [MSA] with a population of ≥1 million). Four counties (7.5%) were classified as nonmetropolitan (22), and the remaining 23 counties were classified as small to medium metropolitan counties (MSA population of 50,000--999,000). During 2007--2009, a total of 201 counties, or 36.2% of the U.S. population in 2008 (2008 U.S. population: 304,059,724), lived in nonattainment counties for 2008 8-hour ozone standard (Figure 2). The majority of counties (158 [78.6%]) in nonattainment for ozone were classified as counties in MSAs with populations of at least 250,000, of which 111 (31.5%) represented counties classified as large central metro or large fringe metro, consisting of ≥1 million population. Twenty-seven counties (13.4%) were classified as nonmetropolitan, and the remaining 16 counties were classified as small metropolitan counties (MSA population of 50,000--249,999).
Assessment of the data by race/ethnicity indicates that Asians (26.2%) and Hispanics (26.6%) had the greatest percentage of residence in 2006 24-hour PM2.5 nonattainment counties (Table). The relative difference between non-Hispanic whites and several racial/ethnic groups living in the areas was >100%: Asians (169%), Native Hawaiians/other Pacific Islanders (125%), and Hispanics (165%).
A similar pattern was observed in the proportion of Asian (50.2%) and Hispanic (48.4%) populations living in 2008 8-hour ozone nonattainment counties (Table). Compared with non-Hispanic whites, Asians were 57% more likely and Hispanics were 51% more likely to live in a nonattainment county.
The percentages of populations living in nonattainment counties also varied by household income and education level. The highest income population (PIR = 3 to ≥5) had the greatest percentage of persons in 24-hour PM2.5 nonattainment counties (13.3%) and 8-hour ozone nonattainment counties (41.1%). Similarly, compared with the referent group (PIR ≤1 [poor]), the highest income population was 2% more likely to live in a PM2.5 nonattainment county and 34% more likely to live in an ozone nonattainment county.
The greatest percentage of persons living in PM2.5 nonattainment counties were those with less than a high school education (16.4%). In contrast, the greatest percentage of persons in ozone nonattainment counties was college graduates or those who received advanced degrees (39.6%). Compared with persons who received less than a high school education, persons who received a high school diploma were 28% less likely to live in a nonattainment PM2.5 county, and persons who received an advanced degree were 10% more likely to live in an ozone nonattainment county. No differences were observed between the percentages of males and females living in PM2.5 nonattainment counties or ozone nonattainment counties.
The findings in this report are subject to at least two limitations. First, residence in a nonattainment county does not necessarily indicate a person's exposure or potential severity of exposure to air pollution. Second, ambient air monitoring sites often are located in counties that are more populated and as a result tend be more representative of air quality in urban areas and might not reflect conditions outside the urban monitoring areas. Likewise, demographic trends observed in this analysis are more likely to closely reflect residents in urban areas than those in rural areas.
The results in this report indicate that minority groups, including Asians and Hispanics, were more likely to live in PM2.5 and ozone nonattainment counties. This finding might be a result of the larger percentage of these populations that live in urban areas (23). In 2007, an estimated 55% of all Asians lived in the 10 metropolitan areas with the largest Asian populations, and 49% of all Hispanics lived in the 10 metro areas with the largest Hispanic populations. The majority of these metropolitan areas (e.g., Los Angeles, California, and New York City, New York) were also designated as nonattainment areas for PM2.5 and ozone (24). In addition, 15.4% of the nonattainment counties for either or both pollutants were in California, where Asians represented 12.5%, and Hispanics represented 36.6% of the total population in California 2008 (25).
Study of other demographic characteristics indicates that persons in the highest income category and in the highest and lowest categories of education attainment have the largest percentages of persons in PM2.5 and ozone nonattainment counties. These results also likely reflect the demographic distribution of persons who live in predominantly urban areas. The populations in urban centers and metropolitan areas tend to be diverse, with areas of wealth integrated with those in poverty (26--30).
Nonattainment areas often are affected by pollution sources such as heavy traffic and other environmental hazards (e.g., industrial emissions) that can affect health. A growing body of research demonstrates that proximity to sources such as traffic can have adverse health effects, especially with respect to vehicular emissions, including PM2.5. In a recent review, the Health Effects Institute concluded that sufficient evidence exists to indicate that traffic exposure exacerbates asthma among children, and suggestive but not sufficient evidence indicates that these exposures cause other adverse health effects (e.g., impaired lung function and increased cardiovascular morbidity and mortality) (31). Zones most affected by traffic-related exposures are estimated to be 300--500 m away from major roads (i.e., roads with intermediate levels of traffic volumes that are less than highways, freeways, and motorways); calculated for large cities, >33% of the U.S. population live in these affected areas (31).
Certain segments of the population, such as very young children and older adults, are particularly susceptible to the effects of air pollution. Because industrial facilities and motor vehicles are key contributors to the levels of PM2.5 and ozone production (7,11), public health efforts should continue to focus on measures to reduce sources of pollution (e.g., promotion of mass transit and development of technology to reduce mobile and stationary source emissions), which in turn should reduce population exposures to unhealthy air quality (32--35).
References
- Dockery D. Health effects of particulate pollution. Ann Epidemiol 2009;19:257--63.
- Pope CA 3rd, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 2006;56:709--42.
- Brook RD, Rajagopalan S, Pope CA 3rd, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 2010;121:2331--78.
- Pope CA 3rd, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med 2009;360:376--86.
- Pope CA 3rd, Burnett RT, Thun MJ, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002;287:1132--41.
- Dockery DW, Pope CA 3rd, Xu X, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med 1993;329:1753--9.
- US Environmental Protection Agency (EPA). Integrated science assessment for particulate matter (final report). Washington, DC: US EPA; 2009. Publication no. EPA/600/R-08/139F. Available at http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=216546.
- US Environmental Protection Agency (EPA). National air quality: status and trends through 2008. Research Triangle Park, NC: US EPA; 2010. Publication no. EPA-454/R-09-002. Available at http://www.epa.gov/airtrends/2010.
- Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F. Ozone and short-term mortality in 95 U.S. urban communities, 1987--2000. JAMA 2004;292:2372--8.
- Kinney PL, Ozkaynak H. Associations of daily mortality and air pollution in Los Angeles County. Environ Res 1991;54:99--120.
- US Environmental Protection Agency (EPA). Air quality criteria for ozone and related photochemical oxidants (2006 final). Washington, DC: US EPA; 2006. Publication no. EPA/600/R-05/004aF-cF. Available at http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=149923.
- Adams WC. Human pulmonary responses with 30-minute time intervals of exercise and rest when exposed for 8 hours to 0.12 ppm ozone via square-wave and acute triangular profiles. Inhal Toxicol 2006;18:413--22.
- McDonnell WF, Stewart PW, Andreoni S, Smith MV. Proportion of moderately exercising individuals responding to low-level, multi-hour ozone exposure. Am J Respir Crit Care Med 1995;152:589--96.
- Anderson HR, Atkinson RW, Peacock JL, Marston L, Konstantinou K. Meta-analysis of time-series studies and panel studies of particulate matter (PM) and ozone (O3): report of a WHO task group. Geneva, Switzerland: World Health Organization, Europe; 2004. Available at http://www.euro.who.int/__data/assets/pdf_file/0004/74731/e82792.pdf.
- Gent JF, Triche EW, Holford TR, et al. Association of low-level ozone and fine particles with respiratory symptoms in children with asthma. JAMA 2003;290:1915--67.
- Giardot SP, Ryan PB, Smith SM, et al. Ozone and PM2.5 exposure and acute pulmonary health effects: a study of hikers in the Great Smoky Mountains National Park. Environ Health Perspect 2006;114:1044--52.
- Triche EW, Gent JF, Holford TR, et al. Low-level ozone exposure and respiratory symptoms in infants. Environ Health Perspect 2006;114:911--6.
- Höppe P, Peters A, Rabe G, et al. Environmental ozone effects in different population subgroups. Int J Hyg Environ Health 2003;206:505--16.
- McConnell R, Berhane K, Gilliland F, et al. Asthma in exercising children exposed to ozone: a cohort study. Lancet 2002;359:386--91.
- Korrick SA, Neas LM, Dockery DW, et al. Effects of ozone and other pollutants on the pulmonary function of adult hikers. Environ Health Perspect 1998;106:93--9.
- Spektor DM, Lippmann M, Thurston GD, et al. Effects of ambient ozone on respiratory function in healthy adults exercising outdoors. Am Rev Respir Dis 1988;138:821--8.
- CDC, National Center for Health Statistics (NCHS). 2006 NCHS urban-rural classification scheme for counties. Hyattsville, MD: NCHS. Available at http://www.cdc.gov/nchs/data_access/urban_rural.htm.
- US Department of Agriculture, Economic Research Service. Minorities represent growing share of tomorrow's work force. Rural Conditions and Trends 1999;9(2):9--13. Available at http://www.ers.usda.gov/publications/rcat/rcat92/rcat92b.pdf.
- Frey WH, Berube A, Singer A, Wilson JH. Getting current: recent demographic trends in metropolitan America. Washington DC: Brookings Institution; 2009. http://www.brookings.edu/reports/2009/03_metro_demographic_trends.aspx.
- US Census Bureau. American factfinder. 2008 population estimates. Available at http://factfinder.census.gov.
- DeNavas-Walt C, Proctor B, Smith J. Income, poverty, and health insurance coverage in the United States: 2008. Current population reports (P60-236[RV]). Washington DC: US Census Bureau; 2009. Available at http://www.census.gov/prod/2009pubs/p60-236.pdf.
- Byun S, Meece J, Irvin, M. Rural-nonrural differences in educational attainment: results from the National Educational Longitudinal Study of 1988-2000. Paper presented at the annual meeting of the American Educational Research Association, Denver, CO; May 2010. Available at www.nrcres.org/Byun%20et%20al_rural_nonrural_differences_in_ educational_attainment_2010_AERA.doc.
- McLaughlin D. Income inequality in America. Rural America 2002;17:14--20.
- UN Habitat: State of the world's cities 2010/2011. Bridging the urban divide. Nairobi, Kenya: United Nations Human Settlements Programme; 2010. Available at http://www.unhabitat.org/documents/SOWC10/L8.pdf.
- Bauman KJ, Graf NL. Educational attainment: 2000. Census 2000 brief. Washington DC: US Census Bureau; 2003. Publication no. C2KBR-24. Available at http://www.census.gov/prod/2003pubs/c2kbr-24.pdf.
- Health Effects Institute. Traffic-related air pollution: a critical review of the literature on emissions, exposure, and health effects. Boston, MA: Health Effects Institute; 2010. Publication no. HEI special report 17.
- Cirera L, Rodriguez M, Gimenez, J, et al. Effects of public health interventions on industrial emissions and ambient air in Cartagena, Spain. Environ Sci Pollut Res 2009;16:152--61.
- Johansson C, Burman L, Forsberg B. The effects of congestions tax on air quality and health. Atmospheric Environment 2009;43:4843--54.
- Pope CA 3rd. Respiratory hospital admissions associated with PM10 pollution in Utah, Salt Lake, and Cache Valleys. Arch Environ Health 1991;46:90--7.
- Wang S, Zhao M, Xing J, et al. Quantifying the air pollutants emission reduction during the 2008 Olympic games in Beijing. Environ Sci Technol 2010;44:2490--6.
FIGURE 1. Counties in 24-hour fine particulate matter (PM2.5) nonattainment areas* --- United States, 2006--2008
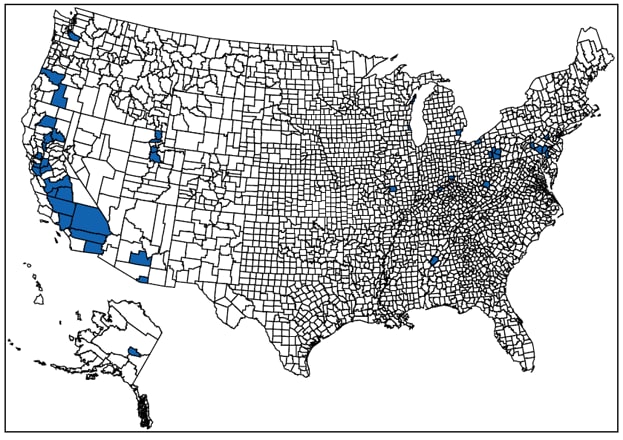
Source: U.S. Environmental Protection Agency (EPA).
* Counties that did not meet the EPA 2006 PM2.5 standard of 35 µg/m3 from 2006--2008.
Alternate Text: The figure shows a county-level map of the United States, indicating the 53 counties that did not meet the EPA 2006 PM2.5 standard of 35 μg/m3 from 2006-2008. Clusters of counties appear in the western region, especially, California and the northeastern region.
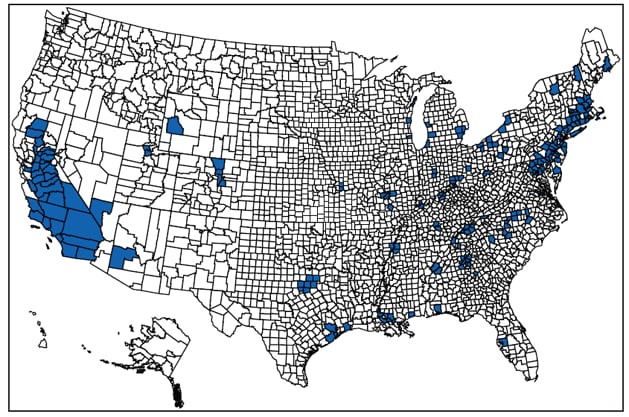
Source: U.S. Environmental Protection Agency (EPA).
* Counties that did not meet the EPA 2008 ozone standard of 75 ppb from 2007--2009.
Alternate Text: The figure shows a county-level map of the United States, indicating the 201 counties that did not meet the EPA 2008 ozone standard of 75 ppb from 2007-2009. Clusters of counties appear in California and northeastern coast.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


