
Monthy Case Studies - 1999
Case #3 - January, 1999
A 42-year-old woman was seen in a New York City hospital for a fever that developed three days after her return from a two-week visit to Haiti. She had visited Montauk on Long Island, NY the previous summer. She also had a previous splenectomy. Figures A, B, and C are from Giemsa stained blood smears taken prior to treatment. Approximately two percent of the erythrocytes were infected, with the majority of parasites looking similar to those shown in Figure A. Occasional forms looked like those in Figures B and C. What is your diagnosis? Based on what criteria?
The patient was treated with chloroquine with good results. However, based on the blood smears taken after treatment, and given the history of her visit to Long Island and of her splenectomy, the hospital staff strongly considered an additional diagnosis of Babesia. Figures D and E are from blood smears taken three days after initiation of therapy (no more forms similar to those in A, B and C were seen). Do you think Babesia is present? Why?
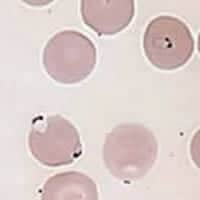
Figure A
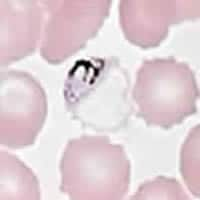
Figure B
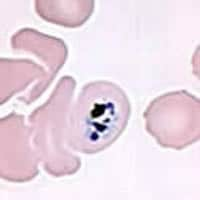
Figure C
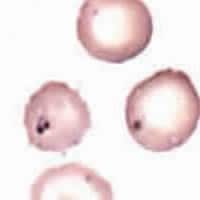
Figure D

Figure E
Answer to Case #3
The parasites shown in Figure A below raise a strong suspicion of Plasmodium falciparum: ring stages with double chromatin dots (blue arrow) and accolé forms (red arrows), and multiply infected erythrocytes (red arrows). This diagnosis is confirmed by stages shown in Figure B on the case studies page: P. falciparum gametocytes. Interestingly, the gametocytes seen in this smear are not the mature crescents usually found in the peripheral blood; they are younger, still developing, gametocytes. Young gametocyte stages usually remain in the deep tissues (e.g., bone marrow, spleen), and only after completing their development do they circulate, as mature gametocytes. The finding of developing gametocytes in the peripheral blood is most probably due to the absence of a spleen in this patient. Also associated with post-splenectomy status is the presence of occasional forms shown in Figure C: trophozoites that are not usually found in the peripheral blood in P. falciparum, except in severe malaria, high parasitemia, or postsplenectomy. Thus, the pretreatment smears indicate a P. falciparum infection with atypical presentation in a splenectomized patient (circulation of developing gametocytes and trophozoites).
On the post-treatment smear, forms as shown in Figure B below and Figure E on the case studies page, raised a strong suspicion that there was also an infection with Babesia. These forms (arrows in Figure B below) are most compatible with dead or dying malaria parasites, not unusual three days after initiation of treatment. There are no findings suggestive of Babesia (such as ring-like parasites that vary in size and shape, dividing forms, and the oft mentioned but rarely seen tetrads). Interestingly, we found no more developing P. falciparum gametocytes, but did see one mature gametocyte (Figure C below). This fits with the known fact that blood schizonticidal drugs (such as the chloroquine used here) are active against developing gametocytes of P. falciparum, but not against mature ones. Thus, the persistence of mature gametocytes following treatment does not imply drug-resistant P. falciparum; such diagnosis rests on the persistence of asexual parasites.
Serology performed at CDC showed the following titers: P. falciparum 1:16,384; P. vivax 1:4,096; P. malariae 1:16,384; P. ovale 1:1,024 and B. microti 1:256. The B. microti results are due probably to cross-reactivity with Plasmodium. PCR performed at CDC was positive for P. falciparum and negative for Babesia, thus confirming the morphologic diagnosis.
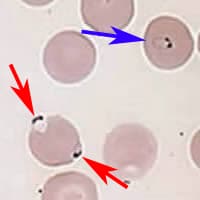
Figure A
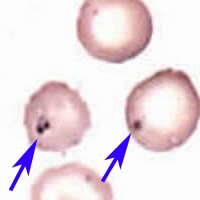
Figure B

Figure B
More on: Malaria
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
 ShareCompartir
ShareCompartir


