Climate Change and Fungal Diseases
Climate change poses many threats to biological, ecological, and societal systems. Shifting temperatures and weather patterns over time are leading to changes in the environment and fungal habitats. Although the impact of climate change on fungal infections is not fully understood due to limiting factors such as a lack of long term fungal datasets, there are several ways that changes in the environment can lead to changes in fungi, where fungi live, and how fungi interact with humans, animals, and plants.1
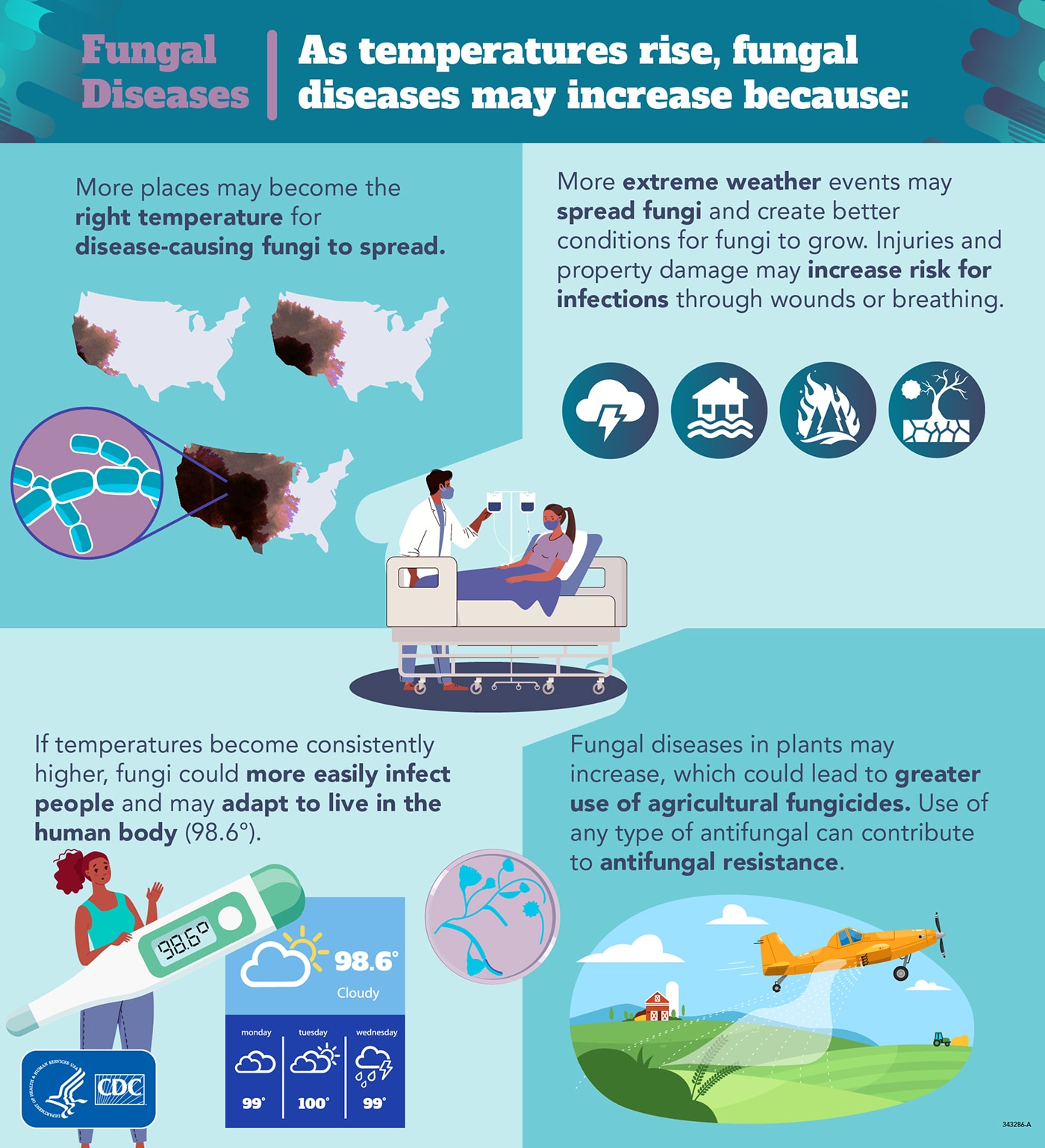
Geographic expansion
Changes to the environment
Increases in temperature and precipitation (e.g., rain and snow) may expand the areas where some fungi can survive in the environment.2,3 For example, the fungus that causes Valley fever, Coccidioides, is known to live in the soil in hot and dry regions. Coccidioides is usually found in the southwestern United States as well as parts of Mexico and Central and South America, but presence of the fungus in Washington state was documented in 2015.4,5 Changes to the environment may also extend the regions where fungi that cause blastomycosis and histoplasmosis are able to survive. The same is true for fungi usually found in tropical or subtropical climates, such as Cryptococcus gattii.3,6
Population movement
The effects of climate change may cause displacement of people (move from one region or part of the world to another) because of unlivable environments. This could lead to overcrowding and poor living conditions, factors that are associated with the risk of ringworm transmission, especially in hot and humid settings.
Extreme weather events
The frequency and intensity of extreme weather events, including large storms, heat waves, droughts, and wildfires, are increasing in some areas.1 These events create conditions that promote the growth and spread of fungal spores. Flooding from heavy rainfall leads to substantial moisture that can facilitate indoor mold growth.7
Other severe weather events, such as dust storms, tornadoes, and wildfires, cause environmental disruptions that can spread fungal spores into the air and potentially transport them to new locations.8–10 Injuries caused by severe weather, including cuts and lesions, can get infected with fungi when they are exposed to contaminated water, soil, or other elements.
Fungal adaptation to heat
Only a small percentage of the estimated millions of fungi on earth can infect people. Currently most fungi cannot survive at human body temperatures (around 98.6 degrees F) and need cooler environments. With shifting temperatures, fungi may be evolving (changing and adapting) to live in warmer conditions, including the human body. New fungal diseases may emerge as fungi become more adapted to surviving in humans.11,12 Heat may also cause other genetic changes that can affect the ability of fungi to infect people.
Antifungal resistance
The use of fungicides in the environment may be contributing to an increase in antifungal resistance, meaning more disease-causing fungi are not killed by the medications designed to treat fungal infections. Triazole antifungal drugs are the main treatment for numerous fungal infections, including aspergillosis. Triazole fungicide use in plant agriculture is linked to triazole-resistant Aspergillus infections that don’t respond to certain antifungal treatment in the clinic.13 Agricultural fungicide use is expected to continue increasing due to rising temperatures, which could lead to new resistant strains of disease-causing fungi.14,15
Further research
It is important to better understand the impact of a changing climate on fungal diseases. CDC is monitoring trends in fungal diseases, particularly geographic spread, and to detect new types of infectious fungi that may affect human health. In addition, CDC is supporting statistical modeling work to explore the effects of climate change on fungi, their habitats, seasonality, and fungal infections. Learn more about key work that CDC National Center for Emerging and Zoonotic Infectious Diseases identified that may be helpful to limit the climate-related threats to human, animal, and plant health [PDF – 4 pages].
How to Protect Yourself From Fungal Diseases
- Learn about fungal diseases and their expanding geographic ranges.
- Some fungal infections can cause symptoms similar to pneumonia. Ask your doctor to be tested for fungal infections if your symptoms are not improving after antibiotic treatment.
- Follow guidance to safely clean up mold in your home after disasters.
- Always follow your doctor’s instructions when taking antifungal medications; avoid using over-the-counter antifungals without a diagnosis.
- https://www.cdc.gov/climateandhealth/effects/default.htm
- https://www.cdc.gov/onehealth/index.html
- https://www.cdc.gov/fungal/fungal-one-health.html
- https://www.cdc.gov/ncezid/what-we-do/climate-change-and-infectious-diseases/index.html
- https://www.cdc.gov/mold/invasive-mold-infections.htm
- https://www.cdc.gov/disasters/psa/hurricane-mold.html
References
- USGCRP. Fourth National Climate Assessment [Internet]. U.S. Global Change Research Program, Washington, DC; 2018 [cited 2023 Jan 6]. Available from: https://nca2018.globalchange.gov
- Gorris ME, Treseder KK, Zender CS, Randerson JT. Expansion of Coccidioidomycosis Endemic Regions in the United States in Response to Climate Change. GeoHealth 2019;3(10):308–27.
- Maiga AW, Deppen S, Scaffidi BK, et al. Mapping Histoplasma capsulatum Exposure, United States. Emerg Infect Dis 2018;24(10):1835–9.
- Oltean HN, Etienne KA, Roe CC, et al. Utility of Whole-Genome Sequencing to Ascertain Locally Acquired Cases of Coccidioidomycosis, Washington, USA. Emerg Infect Dis 2019;25(3):501–6.
- Litvintseva AP, Marsden-Haug N, Hurst S, et al. Valley Fever: Finding New Places for an Old Disease: Coccidioides immitis Found in Washington State Soil Associated With Recent Human Infection. Clinical Infectious Diseases 2015;60(1):e1–3.
- Byrnes EJ, Bildfell R, Frank SA, Mitchell TG, Marr K, Heitman J. Molecular Evidence that the Vancouver Island Cryptococcus gattii Outbreak has Expanded into the United States Pacific Northwest. J Infect Dis 2009;199(7):1081–6.
- Benedict K, Park BJ. Invasive Fungal Infections after Natural Disasters. Emerg Infect Dis 2014;20(3):349–55.
- Tong DQ, Gorris ME, Gill TE, Ardon-Dryer K, Wang J, Ren L. Dust Storms, Valley Fever, and Public Awareness. GeoHealth 2022;6(8):e2022GH000642.
- Neblett Fanfair R, Benedict K, Bos J, et al. Necrotizing Cutaneous Mucormycosis after a Tornado in Joplin, Missouri, in 2011. New England Journal of Medicine 2012;367(23):2214–25.
- Kobziar LN, Thompson GR. Wildfire smoke, a potential infectious agent. Science 2020;370(6523):1408–10.
- Casadevall A, Kontoyiannis DP, Robert V. On the Emergence of Candida auris: Climate Change, Azoles, Swamps, and Birds. mBio 2019;10(4):e01397-19.
- Garcia-Solache MA, Casadevall A. Global Warming Will Bring New Fungal Diseases for Mammals. mBio 2010;1(1):10.1128/mbio.00061-10.
- Toda M, Beer KD, Kuivila KM, Chiller TM, Jackson BR. Trends in Agricultural Triazole Fungicide Use in the United States, 1992-2016 and Possible Implications for Antifungal-Resistant Fungi in Human Disease. Environ Health Perspect 2021;129(5):55001.
- Delgado-Baquerizo M, Guerra CA, Cano-Díaz C, et al. The proportion of soil-borne pathogens increases with warming at the global scale. Nat Clim Chang 2020;10(6):550–4.
- Rhodes LA, McCarl BA. An Analysis of Climate Impacts on Herbicide, Insecticide, and Fungicide Expenditures. Agronomy 2020;10(5):745.